The employment rate of people with mental illness is substantially lower than the rate among the general population (
1), particularly among those with serious mental illnesses (about 15%) (
2,
3). Many people with disabling mental illnesses are eligible to receive cash assistance from the Social Security Administration (SSA) through Social Security Disability Insurance (SSDI) or Supplemental Security Income (SSI). SSDI provides cash benefits to individuals with established work histories who have long-lasting medical impairments that preclude engagement in “substantial gainful activity.” In 2015, SSA defined substantial gainful activity for nonblind individuals as earning at least $1,090 per month. SSI provides income support to individuals who are aged, blind, or disabled (also defined on the basis of ability to engage in substantial gainful activity) and who have limited income and resources. In 2016, almost one-quarter (24.7%) of beneficiaries ages 18–64 receiving SSDI, SSI, or both had mood disorders, “schizophrenic and other psychotic disorders,” or other mental disorders (
4,
5). A large percentage of beneficiaries with psychiatric disabilities want to work, but they face many barriers (
6).
To date, considerable research has demonstrated that the individual placement and support (IPS) model of supported employment can improve employment outcomes among people with serious mental illness relative to standard mental health care and vocational services (
7). High-fidelity IPS focuses on competitive employment, systematic job development, rapid job search, integrated clinical and vocational services, benefits planning, zero exclusion (i.e., no exclusions on the basis of an individual’s readiness, diagnoses, symptoms, substance use history, psychiatric hospitalizations, homelessness, level of disability, or legal system involvement), time-unlimited supports, and worker preferences (
8). More than 20 randomized controlled trials of IPS have shown significant positive employment outcomes for adults with serious mental illness compared with outcomes of standard mental health care and vocational services. However, these studies typically have a follow-up period of 1 to 2 years (
9), and little is known about IPS’s long-term effects.
Two small uncontrolled studies of employment outcomes in the 8 to 12 years after IPS enrollment showed that almost half of those interviewed had been employed for at least 50% of the follow-up months (
10,
11). Only in two other studies have researchers investigated the long-term impact of evidence-based supported employment services for individuals with psychiatric conditions (
12,
13). Both studies showed that supported employment has a positive impact on long-term outcomes, such as employment, earnings levels, and job tenure. However, the sample size for one of these studies was limited, and the generalizability of the findings to SSA disability beneficiaries is unknown (
12). Although the other study included only SSA disability beneficiaries, only two of the six programs included in the study strictly adhered to the IPS model (
13).
The Mental Health Treatment Study (MHTS) was an SSA demonstration that provided intervention services for a 2-year period from 2006 to 2010 to SSDI beneficiaries with psychiatric conditions (including those with concurrent SSI). A total of 2,238 beneficiaries who were between the ages of 18 and 55, had a primary impairment of schizophrenia or affective disorder, expressed interest in working, and volunteered to participate after completing an informed consent process were randomly assigned to a treatment or control group.
The treatment group received IPS; systematic medication management services; coordination of medical and psychiatric care from a nurse care coordinator; access to other evidence-based behavioral health and related services; payment of the beneficiary’s share of health insurance premiums, copayments for behavioral health–related services, and premiums for any supplemental health insurance required to ensure coverage comparable with Medicare parts A, B, and D; payment of other out-of-pocket service expenses and for noncovered services; and suspension of medical continuing disability reviews for 3 years after study enrollment. For participants in the treatment group, average per-person spending for services and support other than IPS averaged about $1,776 per year. Participants enrolled in MHTS as early as 2006 or as late as 2008. The control group did not receive any study-provided services or benefits. Instead, the group received a resource manual listing available local and national services and resources for people with mental illness and up to $100 for participation in interviews.
On the basis of self-reported data, during the study period beneficiaries in the MHTS treatment group were significantly more likely to be employed at any point (60.5% vs. 40.2% in the control group, p<0.001), were employed more total months (6.23 vs. 3.65 in the control group, p
<0.001), and had higher average past month’s earnings ($148.16 vs. $97.41 in the control group, p<0.001) (
14,
15). Given the focus on SSDI beneficiaries, the MHTS also examined the effect of the intervention on substantial gainful activity and disability income.
If SSDI beneficiaries are able to work above the substantial gainful activity level for more than 9 months in a rolling 60-month window, SSA suspends their cash benefits for each month in the next 36 months in which earnings exceed the substantial gainful activity level after 3 grace period months. Starting in the 37th month, SSA terminates benefits in the first month that earnings exceed the substantial gainful activity level. For concurrent SSDI-SSI beneficiaries, SSA may also reduce monthly SSI payments if an individual earns more than the substantial gainful activity level. The treatment and control groups in MHTS did not differ in the percentage of participants reporting average monthly earnings above the substantial gainful activity level (8.18% in the treatment group vs. 8.76% in the control group, p=0.739) or in average monthly income from SSDI or SSI (
15).
In the original MHTS analyses, researchers did not determine whether the short-term improvements in employment and earnings were maintained or improved over time. If employment and earnings among the treatment group improved over time at a greater rate than those of the control group, the percentage of treatment group participants exceeding the substantial gainful activity level might also increase at a faster rate and eventually lead to reductions in disability benefits received. In this study, we assessed the long-term impact of MHTS (the largest randomized controlled trial of evidence-based supported employment and the only study that examined IPS as part of a support package that included systematic medication management) on employment, earnings, and suspension/termination of disability benefits due to work.
Methods
Participants
The study included 23 sites selected from among more than 50 IPS programs already in operation in 2005 (
15). Sites were selected in part to ensure diversity with regard to Census region, urbanicity, population composition, and the way the site was organized. The long-term analysis included 2,160 participants: 1,062 in the treatment group and 1,098 in the control group. In the original MHTS, 2,238 participants were randomly assigned to the treatment or control group, but 46 participants assigned to the treatment group were dropped from the analysis because they did not complete the general medical examination required by SSA for participation or did not meet other initial study requirements (e.g., moved out of the country). In addition to these 46 participants, we dropped 32 participants from the long-term analysis because they died during the original study period and, as a result, had no data for the long-term study period. Mortality did not differ significantly between groups during the study period.
Several university and other institutional review boards approved and monitored the original MHTS, and all participants provided written informed consent at enrollment. As a way to protect participant confidentiality and comply with restrictions applicable to the SSA data, SSA employees conducted the analyses and provided aggregate results to non-SSA authors; personal identifiers and long-term earnings data were not accessible to non-SSA authors, and aggregate data were protected through a memorandum of agreement between SSA and coauthors.
Data Sources
Two authors (K.F. and T.H.) linked MHTS participant identifiers and baseline demographic data to SSA’s Master Earnings File and Disability Analysis File. The Master Earnings File contains annual data on earnings that employers and self-employed individuals report to the Internal Revenue Service (
16). The Disability Analysis File contains monthly measures, derived from SSDI and SSI program administration files, of the suspension or termination of cash disability benefits because of work. This analysis included data from 2011 to 2015. Because beneficiaries were enrolled in the study on a rolling basis, the time between completion of participation in the original study and the start of the follow-up period varied from less than 1 year to 3 years.
Statistical Analysis
We analyzed outcomes using both cross-sectional and longitudinal statistical methods. We used the cross-sectional analyses to examine whether demographic characteristics and the following summary outcomes were significantly different between the treatment and control groups over the course of the follow-up period: odds of any earnings, average total earnings, average total earnings among workers, odds of SSDI or SSI benefit suspension or termination for at least 1 month because of work, number of months in which SSDI or SSI benefits were suspended or terminated because of work, average estimated benefits forgone for work, and average total cash payments from SSDI and SSI. Because of the preponderance of zero values for average total earnings, months suspended or terminated for work, and benefits forgone for work, we used the nonparametric Kruskal-Wallis test to assess differences in significance across these variables. For other continuous variables, we used the F test; for categorical variables, we used the chi-square test.
We used generalized linear mixed-effects regression models to analyze the long-term (longitudinal) effects of MHTS on a limited set of outcomes, including odds of any earnings, average earnings, average earnings among workers, and odds of SSI or SSDI benefit suspension or termination for at least 1 month in the year because of work. In addition to the intent-to-treat model examining average earnings among all participants, we also analyzed average earnings among workers to disentangle the effects on working at all from the effects on earnings themselves among those who worked; however, it should be noted that workers in the treatment and control groups may differ in nonspecified ways because workers in the control group obtained employment without the benefit of MHTS services.
In all models, we adjusted for serial correlation due to repeated measures of an individual over time and accommodated data with missing values (assuming missing at random). The models included treatment group, time, and group × time interaction terms as fixed effects. The treatment effect (or benefit of the MHTS intervention vs. control) was reflected by the significance of the interaction term. As in the original MHTS (
14,
15), we did not control for other variables because the randomization ensures that the two groups are balanced in terms of measured and unmeasured factors, with any differences between groups occurring by chance (
17). We conducted the analyses using the SAS, version 9.4, PROC GLIMMIX procedure.
Results
A summary of participant characteristics can be found in
Table 1. Consistent with the original analyses of short-term MHTS results, the treatment group had a slightly higher percentage of participants with a diagnosis of schizophrenia than did the control group, and there was a small difference between groups in the race distribution. Participants in the two groups did not differ significantly on sex, education, age, or marital status.
A summary of the differences in outcomes between the two groups can be found in
Table 2. During the follow-up period, participants in the treatment group were statistically significantly more likely than those in the control group to realize any earnings. In addition, for both the full intent-to-treat sample and the subset that worked, the treatment group had higher average total earnings. None of the disability benefit outcomes differed significantly between groups.
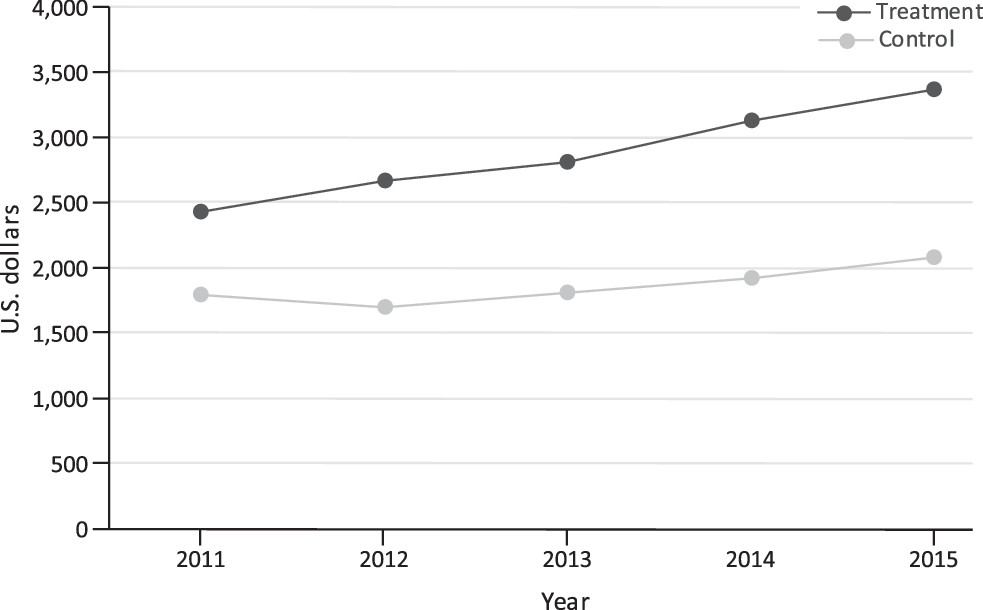
The results of the generalized linear mixed-effects model indicate that, in 2011, participants in the treatment group were 2.6 times more likely than those in the control group to report any earnings (p<0.001); moreover, they earned $737 more in that year than the control group (p=0.017;
Table 3). Over time, earnings grew by $134 more per year in the treatment group than in the control group (p=0.004;
Figure 1 and
Table 3). Among only those who worked, the treatment group did not earn significantly more in 2011 than did the control group; however, average earnings increased by $261 more per year in the treatment group than in the control group (p=0.015), exceeding the annual increase in the full intent-to-treat sample. Participants in the two groups did not differ in their likelihood of suspension or termination of disability benefits due to work (odds ratio=1.11, 95% confidence interval=.68–1.80, p=0.690).
Discussion
Our findings suggest that the service package offered through MHTS, which had IPS as its centerpiece, had a long-term positive impact on the likelihood of employment, average earnings, and the trend in average earnings over time for SSDI beneficiaries with psychiatric disabilities and an interest in working. Furthermore, the low rate of benefit suspension indicates that the MHTS interventions did not affect disability benefit receipt from 5 to 7 years after participation in the original study. Although significant, the difference in average annual earnings between groups was quite small, particularly from the perspective of payers seeking more substantial long-term cost benefits from the 2-year intervention. However, the finding of continued effects that increased up to 5–7 years after the intervention ended is striking because the typical expectation is that such effects would decay over time (
13). Analyses of the long-term cost benefits of IPS and other employment supports would enrich the understanding of the cost implications of providing such interventions.
The results showing enduring effects of better employment outcomes for clients receiving the MHTS intervention are consistent with the findings of the original MHTS (
14,
15) and several other short- and long-term studies of supported employment (
7,
12,
13). Two unique strengths of the study were that earnings outcomes were based on data submitted by employers to the Internal Revenue Service rather than on self-report or other less reliable sources of such information, and attrition was exceptionally low: data for 96.5% (N=2,160/2,238) of the original intent-to-treat sample were available for the analyses, a much higher rate than in most published IPS studies, except those with short follow-up periods. Furthermore, this is the first published long-term controlled study of high-fidelity IPS conducted in the United States.
Although earnings may not be sufficient to suspend or terminate disability benefits, individuals with serious mental illness may still benefit from employment. For example, a descriptive study of the personal economies of people with psychiatric disabilities showed that for people with low incomes, even low levels of employment can mean the difference between meeting and not meeting monthly expenses, and increases as low as $20–$100 per month can contribute meaningfully to paying for monthly transportation, utilities, food, loan repayment, or entertainment (
18). Several previous studies suggest that employment may also have a positive impact on mental health, self-esteem, and illness management for individuals with serious mental illness (
19,
20).
A study in the general population showed that “even a small number of working hours generates significant mental health and well-being benefits for previously unemployed or economically inactive individuals” (
21). Studies of long-term effects of IPS and other employment supports on clinical outcomes and participant perspectives on their financial status, quality of life, and other outcomes would be helpful for assessing the long-term value of such services and supports. In spite of the positive outcomes associated with IPS, these services are still largely unavailable to those who might benefit from them (
9). Data reported by state mental health authorities suggest that only 2% of adults with serious mental illness have access to IPS and that identifying and securing funding for these services continue to pose a challenge (
22). Improving access to IPS may have important employment implications for individuals with serious mental illness.
The results of the study should be interpreted in light of its limitations. First, the MHTS was not nationally representative: sites were selected with a convenience sample to help ensure IPS services were fully operating at high fidelity to the evidence-based practice, and individuals had to be interested in working to participate. Therefore, the sample and results may not generalize to all sites delivering supported employment or to all SSDI beneficiaries with psychiatric disabilities or all individuals with serious mental illness. Second, because MHTS offered IPS as part of a package of services and supports, it was not possible to determine the extent to which components other than IPS drove favorable long-term employment outcomes. However, an extensive literature has demonstrated that when used alone, IPS has better short-term effectiveness than standard mental health care and vocational services available to clients of community mental health centers, and we know of no studies demonstrating significant effects of the other components of the MHTS intervention on employment outcomes. Nevertheless, the MHTS intervention was generous, and the level of positive long-term results, particularly for the population of SSDI beneficiaries with psychiatric conditions (many of whom are not otherwise connected to mental health services), may not be replicable if the full package of services and supports is not available.
Finally, participants entered the study on a rolling basis, so the period of follow-up is not directly comparable across all study participants. This variation, however, was applied equally to the treatment and control groups, so it would not be expected to affect the impact estimates. Because data collection ended after 24 months, we do not know whether any of the participants (treatment or control) received IPS or other vocational services after their participation in the original study ended. If control group participants received such services, the likelihood of finding significant differences in long-term employment outcomes between groups would be reduced; if treatment group participants received such services, the effect would be amplified.
Conclusions
People with psychiatric disabilities are one of the largest impairment groups participating in SSDI and SSI, representing approximately 37% of all beneficiaries when both primary and secondary impairments are considered (
6). Although beneficiaries with psychiatric disabilities often want to work, they are more likely than their counterparts with other disabilities to report various employment barriers (
6). IPS provided in combination with systematic medication management and other support demonstrated statistically significant, positive long-term effects on employment and earnings for SSDI beneficiaries with psychiatric conditions; however, differences in earnings between the treatment and control groups were small and may not be clinically significant. Although providing access to IPS did not influence the receipt of disability benefits, previous literature shows that employment can have short-term effects on mental health and self-esteem. These previous studies suggest that long-term positive effects on employment and earnings may also yield long-term nonfinancial benefits.
Acknowledgments
This research was supported by grant 1 DRC12000001-01-00 from the U.S. Social Security Administration (SSA). The findings and conclusions are solely those of the authors and do not necessarily represent the views of SSA.