Nonfatal deliberate self-harm has emerged as a significant public health problem in the United States and is now the second leading cause of violence-related injury among 10- to 19-year-olds (
1). Emergency departments (EDs), where most seriously injured adolescent self-harm patients seek care, are at the front line for triaging these young patients and linking them with social and psychological services. Such services typically focus on reducing their risk of subsequent suicidal behavior (
2,
3). A small but growing literature also reports, however, that deliberate self-harm among adolescents—especially suicide attempt, as distinguished from nonsuicidal self-injurious behavior—is associated with other adverse mental health, physical health, and economic outcomes over the life course, suggesting that self-harming adolescents may have broader health-related needs that currently receive little attention (
4–
8).
One approach to understanding these health needs and to informing the design and focus of future intervention programs is to examine self-harming youths’ patterns of health service utilization. Service utilization is a key indicator of need for medical care, propensity to seek care, and barriers to receipt of care and is frequently used as a metric for guiding resource allocation and developing interventions (
9–
11). At the system level, excess health service utilization contributes to strained provider resources and financial burden (
12). It also has implications for young people’s educational attainment, labor market success, and financial independence during the critical transition to adulthood, because obtaining frequent medical care impedes youths’ ability to attend school and work and can involve costly medical expenditures (
13–
17). To date, however, studies of health service use and associated costs among self-harming youths remain scarce.
Why might self-harming adolescents have higher rates of health care use and costs when compared with their peers? Perhaps most obviously, deliberate self-harm is typically accompanied by serious psychological problems (including a confluence of internalizing psychopathology, externalizing psychopathology, and impaired executive functioning) (
18–
21) and family dysfunction (
22), factors that independently increase risk of poor health outcomes, poor adherence to medical treatments, and increased health care use (
4,
23–
27). However, associations between self-harm and subsequent self-reported health care use appear to persist even after control for psychiatric diagnoses and family-level characteristics (
5,
7). Other potential explanations include self-harming adolescents’ disproportionate risk of receiving ineffective outpatient care (
27–
30), as well as self-reinforcing cycles wherein an adolescent’s history of self-harm (especially if it results in hospitalization) drives caregivers and ED clinicians to interpret new health crises as serious and to preferentially recommend emergency treatment or admission (
31). Such processes could result in higher rates of hospital-based health care utilization, an outcome that is particularly important to understand because it reflects the costliest and most medically severe component of health care (
32).
To expand the limited evidence base on the population-level health care burden associated with adolescent self-harm, this study used contemporary data from California, a large state with considerable demographic heterogeneity (
33), to investigate ED utilization, inpatient admissions, and inpatient costs among adolescent patients presenting to an ED with a diagnosis of deliberate self-harm (with or without intent to die). Because the design of future intervention programs depends on the nature of adolescents’ health needs, the study also examined the respective contributions of psychiatric versus nonpsychiatric complaints to patterns of utilization and inpatient costs.
Methods
Data
This study was approved by the University of California, Merced, Institutional Review Board (IRB) and the California Department of Public Health IRB. The California Office of Statewide Health Planning and Development provided nonpublic, deidentified, individual-level ED and inpatient admission patient encounter data from all California-licensed hospital facilities, excluding federal hospitals, for years 2006–2015 (
29,
30).
The study sample consisted of all adolescents ages 10 to 19 who had an ED encounter in 2010 that included a unique identifier (encrypted Social Security number) and a California residential zip code (
34). To construct the cohort, each patient’s unique identifier was used to link all ED and inpatient visits made after his or her index 2010 visit to any California hospital facility for the years 2010–2015. Links were also made to patients’ prior ED visits for the years 2006–2009.
Study Groups
Patients with deliberate self-harm were defined as those who presented in 2010 to any ED with an
ICD-9-CM (
31) external cause of injury code (E-code) of E950.0–E958 in any diagnostic position, indicating self-inflicted injury by poisoning, strangulation or suffocation, submersion, firearm, cutting or piercing, jumping, or other method (
32).
ICD-9-CM E-codes E950–E958 do not distinguish between events involving self-inflicted injury with intent to die and those involving no intent to die (i.e., nonsuicidal self-injury) (
33,
34); therefore, this case definition captured both true suicide attempts as well as self-harm injuries with no suicidal intent.
The main comparison group (hereafter referred to as general control patients) comprised a randomly selected sample of adolescent patients who presented to any ED in 2010 for any reason other than self-harm; they were matched 3:1 to self-harm patients. Matching factors comprised patient sex, age (within 1 year), residential zip code, and month of the index visit to control for basic sociodemographic characteristics and seasonality. At least one matched general control patient from the same zip code was identified for 94.0% of self-harm patients. Where no exact zip code match was available, general control patients were sought from adjacent zip codes most closely matching that of the self-harm patient in terms of absolute proportional differences in population density and median income (adjacencies defined by queen’s contiguity; population and income differences equally weighted). This procedure identified general control patients for an additional 3.6% of self-harm patients.
To assess whether patients with deliberate self-harm experienced study outcomes at a higher rate than patients with other mental health problems, we also identified a secondary comparison group, comprising adolescent ED patients who presented in 2010 with a principal diagnosis code indicating a mental disorder but not with deliberate self-harm. These psychiatric control patients were matched 3:1 to self-harm patients on sex, age, and month of index visit. Clinical Classification Software (CCS) codes, which aggregate
ICD-9-CM diagnoses into a smaller number of discrete, clinically meaningful categories (
35), were used to identify mental disorder visits (CCS codes 650–659, 662–663, and 670, comprising diagnoses for anxiety, mood, behavioral, personality, and psychotic disorders). Patients with suicidal ideation could be included in the psychiatric control group.
Index visits were defined as follows: for self-harm patients as their first self-harm visit in 2010, for general control patients as their first ED visit for any condition in 2010, and for psychiatric control patients as their first qualifying mental disorder visit in 2010. Patients who died at their index visit were excluded.
Outcome Variables
Study follow-up for each patient began on the day after his or her index ED visit in 2010 and ended September 30, 2015, to avoid potential reason-for-visit misclassification problems related to the mandatory transition from ICD-9-CM to ICD-10-CM coding on October 1, 2015. Three primary study outcomes were examined. Emergency department utilization was defined as the patient’s total number of ED visits during follow-up. Inpatient admissions were defined as the total number of times the patient was hospitalized overnight during follow-up, regardless of length of stay. All hospital facilities (community, psychiatric, etc.) and admission types (planned and unplanned, including admissions resulting from an ED visit) were included in this count. To determine whether psychiatric complaints accounted for any excess utilization among self-harming adolescents, each ED and inpatient visit was identified as psychiatric or nonpsychiatric, with psychiatric visits defined as those with a primary diagnosis of anxiety, mood, behavioral, personality, or psychotic disorder (CCS codes 650–659, 662, 663, or 670). This information was used to create psychiatric and nonpsychiatric versions of the ED utilization and inpatient admissions outcome variables.
Total inpatient costs were estimated by using annually determined Medicare Severity Diagnosis-Related Group (MS-DRG) payment rates associated with the principal
ICD-9-CM diagnosis code at each hospitalization, summed over follow-up. Medicare per-discharge base payment rates and MS-DRG relative weights were obtained from the Centers for Medicare and Medicaid Services Web site (
36). Use of Medicare cost estimates for each visit allowed for standardizing the amount that different hospitals charge for the same reason for visit, which may vary considerably based on the facility’s geographic location, contractual agreements with insurance companies, and other factors. Cost data were not available for ED visits, and thus this outcome underestimates study patients’ costs associated with hospital-based care.
Covariates
Patient race-ethnicity (white, black, Hispanic, Asian/Pacific Islander, and other), payer type (private, Medicaid, self-pay, and other), and disposition (discharged home, admitted as inpatient, and other) were assessed at each patient’s index visit. Controlling for disposition accounted for both severity of the patient’s medical-psychological condition and the possibility that an index hospitalization may have resulted in a greater likelihood of an ED visit or admission in the future (
34). To account for baseline group differences in health status and propensity to obtain care from the ED, several utilization history variables based on patients’ linked ED records from 2006–2009 were constructed: total number of prior ED visits; any prior visit for a mental health problem, including deliberate self-harm (CCS codes 650–659, 662, 663, or 670 in any diagnostic position); and any prior visit for substance use (CCS codes 660–661 in any diagnostic position) (
34).
Statistical Analyses
Descriptive statistics were calculated for all variables, and characteristics were compared between self-harm patients and control patients. Because all service utilization outcomes were overdispersed count variables, negative binomial regression (the Stata command
nbreg) was used to estimate incidence rate ratios (IRRs) (
37) comparing self-harm patients with matched general control patients and then, separately, with matched psychiatric control patients. Akaike information criterion fit indices and the statistically significant dispersion parameters confirmed that negative binomial models were a better fit for the data than were Poisson models. For these outcomes, all study patients were included.
For inpatient costs, analyses were restricted to patients who had any inpatient admission during follow-up, because patients without an inpatient admission were not at risk of this outcome. A generalized linear model with a gamma distribution and logarithmic transformation was used for this outcome (
38,
39), with coefficients interpreted as the percentage change in inpatient costs associated with being in the self-harm group.
Patient characteristics assessed at the index visit and patient history of ED utilization during 2006–2009 (total visits, any visit for mental health, and any visit for substance use) were included as covariates in each regression model. All models used robust standard errors to account for the matched cohort design and repeated-measures data (
40,
41) and included an offset term defined for each patient as (September 30, 2015 minus patient’s index visit date) to account for differences in follow-up time. Statistical analyses were conducted by using Stata 14.0.
Results
Sample Characteristics
Of the 481,915 unique patients in the study data set who presented to a California ED in 2010, a total of 5,533 received an E-code indicating deliberate self-harm injury. Of these self-harm patients, 5,396 (97.6%) were matched to at least one general control patient (total general control patients, N=14,921) and 5,284 (95.5%) were matched to at least one psychiatric control patient (psychiatric control patients, N=15,835). The most common E-codes among self-harm patients were for self-poisoning (N=3,210, 59.5%) and cutting or piercing (N=1,349, 25.0%) injuries. The diagnostic codes most frequently present among general control patients at the index visit were sprains or strains (N=1,097, 7.4%) and superficial injury (N=945, 6.3%). Among psychiatric control patients, the most frequent diagnostic codes at the index visit were anxiety disorder (N=5,316, 33.6%) and mood disorder (N=4,270, 27.0%). Demographic characteristics assessed at patients’ index visits, as well as patient histories of ED utilization between 2006 and 2009, are shown in
Table 1.
ED Utilization
Deliberate self-harm patients had a mean of 7.2 ED visits during the follow-up period, compared with 4.3 visits among general control patients and 6.6 among psychiatric control patients (
Tables 2 and
3). In negative binomial regression models controlling for sociodemographic characteristics and histories of ED utilization, rates of overall ED utilization were approximately 40% higher among self-harm versus general control patients (IRR=1.39) (
Table 2). The relative magnitude of the two groups’ differences in ED visit rates was greater for psychiatric visits (IRR=3.62) than for nonpsychiatric visits (IRR=1.27). However, because both patient groups presented to the ED much more frequently for nonpsychiatric reasons than for psychiatric reasons, the excess burden of ED utilization associated with deliberate self-harm was greater for nonpsychiatric visits than for psychiatric visits.
Rates of overall ED utilization did not differ significantly between self-harm and psychiatric control patients, and self-harm patients’ ED utilization rate for psychiatric complaints was slightly lower (
Table 3). Self-harm patients’ rate of ED visits for nonpsychiatric complaints, however, was 8% higher, compared with the rate for psychiatric control patients (IRR=1.08). (Full model results for both comparisons, with covariate estimates and dispersion parameters, are provided in an
online supplement.)
Inpatient Admissions
The proportions of patients with any inpatient admission during follow-up were as follows: self-harm patients, 50.2% (N=2,711); general control patients, 29.7% (N=4,432); and psychiatric control patients, 43.0% (N=6,802). The mean number of inpatient visits during follow-up was 1.7 among self-harm patients, compared with 0.6 among general control patients and 1.3 among psychiatric control patients (
Tables 2 and
3).
In adjusted negative binomial regression models, rates of overall inpatient admission were approximately 80% higher among deliberate self-harm versus general control patients (IRR=1.81) (
Table 2). After admissions were divided into those for psychiatric and for nonpsychiatric reasons, only psychiatric admission rates were significantly higher for the self-harm group, compared with the general control group (IRR=5.55). Rates of both types of inpatient admissions were significantly higher (14% to 17%) among self-harm patients, compared with psychiatric control patients (
Table 3) (see
supplement for full model results).
Inpatient Costs
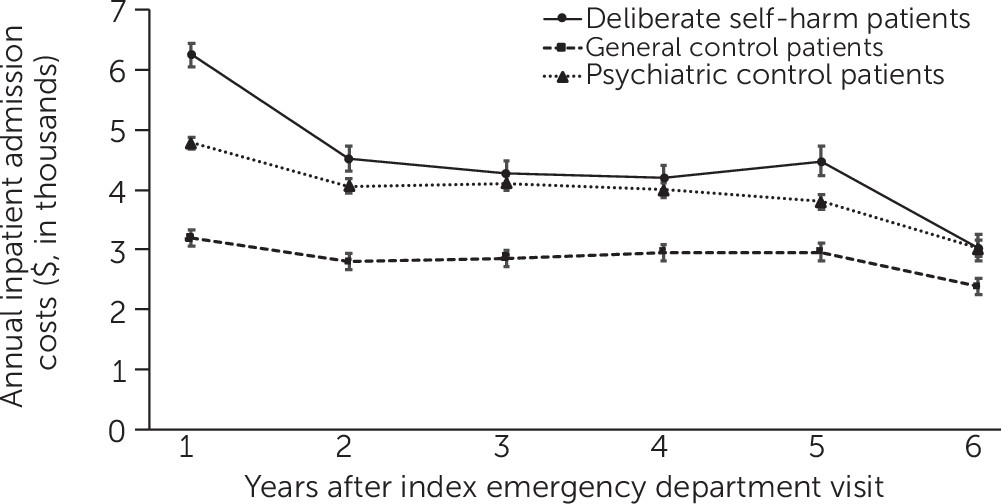
Among hospitalized patients, inpatient costs accrued by patients with deliberate self-harm were higher compared with costs among general control patients in each year of follow-up and higher in most years compared with psychiatric control patients (
Figure 1). Mean total accrued inpatient costs were $16,571 for self-harm patients, compared with $9,976 for general control patients, a 21% difference after covariate adjustment (
Table 2). However, this excess cost burden was driven by psychiatric admissions: self-harming adolescents’ psychiatric inpatient costs were four times those of general control patients, but their costs for nonpsychiatric admissions were significantly lower than those of general control patients.
Total and psychiatric inpatient costs for self-harm patients were only marginally higher than those for psychiatric control patients, but their inpatient costs for nonpsychiatric complaints were 11% higher than those for psychiatric control patients, a significant difference (
Table 3).
Discussion
This is the first population-based U.S. study to examine objective measures of long-term health service utilization and inpatient cost patterns among adolescents who presented to the ED for deliberate self-harm. Results indicate that adolescent ED patients presenting with deliberate self-harm had substantially higher rates of subsequent ED use, inpatient admissions, and inpatient costs over 5 years of follow-up, compared with patients who presented with other complaints. Many of these differences persisted, albeit reduced in magnitude, when self-harm patients were compared with patients with other mental health problems, suggesting that deliberate self-harm confers a certain amount of unique vulnerability.
Psychiatric problems were involved in most of self-harming adolescents’ excess inpatient admissions and associated costs. However, both psychiatric and nonpsychiatric complaints contributed to their excess ED utilization—indeed, nonpsychiatric complaints were the primary diagnoses for approximately 84% of ED visits among self-harming adolescents after the index visit. These findings indicate the need for greater clinical and public health attention to the full spectrum of self-harming youths’ health-related needs, including both somatic and psychiatric problems.
This work builds on previous studies showing that deliberate self-harm is associated with higher rates of self-reported ED use and psychiatric hospitalization (
5,
7), poor physical health (
5,
6,
8), poor mental health (
5,
42,
43), poor social and economic outcomes (
5,
42,
44), and excess mortality (
45–
47). Many of these studies relied on non-U.S. samples or cohorts born in the 1970s, whose experiences (particularly with health care systems) may not be generalizable to those of contemporary U.S. youths. This study expands this literature by demonstrating, in a contemporary and diverse population-based U.S. sample, that adolescent self-harm was also associated with objectively measured health care utilization and associated costs, even after control for multiple confounding variables, including prior ED use (
34).
This study has implications for clinical quality monitoring and intervention planning among self-harming adolescents. High rates of ED and hospital use likely have a significant impact on self-harming adolescents’ daily lives and future prospects. Time spent in the ED or hospital may disrupt schooling and employment trajectories, result in social isolation from family and peer networks (
48), and encourage overreliance on EDs for medical care (
49). Excess hospital-based service use may be an indicator of fragmented and irregular medical care.
However, higher rates of service utilization may also reflect appropriate use of emergency and inpatient care among seriously distressed adolescents, whose mental health needs may be too severe for management in outpatient settings. Families and providers caring for adolescents who deliberately self-harm must balance youths’ health needs with the possibility of social disruptions resulting from inpatient care. Future research should investigate whether high rates of utilization among self-harming adolescents stem from true medical need, barriers to receiving outpatient care, overall higher levels of engagement with the mental health system, or other factors. From a clinical perspective, integrated care models that use mental health specialists to support primary care providers in delivering mental health care, disease management, and client education may be well suited to addressing the broad health needs observed among adolescent patients with deliberate self-harm (
50,
51). Universal suicide risk screening and mental health assessment of adolescent ED patients may also result in clinical benefit (
52,
53).
This study had several limitations. The principal diagnostic position was used to categorize a visit’s primary complaint as psychiatric or nonpsychiatric. Medical coders do not always accurately record the patient’s primary complaint, which may have resulted in misclassification of this variable. Visits occurring out of state were not observable (
34), and information on many important aspects of adolescents’ health and health care, including their outpatient visits, prescription medications, and untreated illness, was not available (
9). The comparison groups comprised other ED patients; however, we believe that this likely biased the estimated associations toward the null because ED patients are less healthy than the general population (
54).
Conclusions
Results from this study demonstrate that deliberate self-harm among adolescents is associated with long-lasting and costly patterns of health service utilization, especially for psychiatric complaints. In light of increasing rates of adolescent self-harm, future research with this patient population should investigate the mechanisms underlying this pattern, identify any factors that confer excess risk among self-harming youths (
55), and consider incorporating health care utilization as a key patient outcome.