Aside from emotional and physical burdens, depression can cause considerable social burdens, such as shame and stigma, which can lead to social isolation and withdrawal (
1,
2). Such negative social pressures may be partially responsible for low rates of treatment seeking by individuals with depression (
3,
4). If left untreated, depression is likely to result in significant negative outcomes in terms of health, social consequences, and economic burdens (
5).
Factors that are associated with lower likelihood of treatment seeking include demographic characteristics, such as being male and being single (
6,
7), and social factors, such as lower education level, limited understanding of symptoms, and low knowledge of available resources (
6,
8,
9). Interestingly, improving symptom recognition and knowledge of treatment can increase the likelihood of treatment seeking (
7,
9).
Interpersonal relationships may play a unique role in an individuals’ understanding of their own emotional or mental problems as well as their attitudes toward treatment. Having family members who disclose a history of mental health issues and treatment increases understanding of one’s own emotional problems; similarly, one’s peers can influence attitudes toward depression and decisions about treatment (
10). Indeed, some research suggests that social support (e.g., from confidants) may be a preferred source of help and information for individuals with emotional problems (
11). Conversely, both self-stigma and a perception of stigma from others about depression and treatment may have an adverse effect on both recognizing depression and seeking care for it. Attitudes toward treatment and depression in general have been shown to affect individuals’ perceptions about whether treatment is needed for themselves or others (
12).
Given the importance of one’s family and social circle for support and information about emotional problems and treatment, the aim of this study was to examine whether people who screened positive for depression were more likely to seek treatment if they had personal knowledge of other individuals with emotional or mental problems or of those who had sought treatment for such problems.
Methods
A total of 239 participants were recruited from an international Internet-based depression screening study (
13). Participants eligible for invitation were ≥18 years of age, were able to read English, and had screened positive for current major depression.
Eligibility was determined based on data collected by the referring study (see online supplement). Approximately one week after taking part in the referring study, eligible individuals were sent an invitation e-mail with a link to the current study. Once on the study Web site, participants read and electronically signed the consent document and proceeded to the study questionnaires described below. Participants also completed other measures that are not part of this report. Participants completing over 80% of the questions were paid US$10. All procedures were approved by the institutional review board of the University of California, San Francisco.
Demographic characteristics, including age, gender, relationship status (partnered or unpartnered), employment status (employed or unemployed), years of education, and residential setting (urban, rural, or neither), were taken from the referring study. Participants were asked, “Did you ever seek professional help or treatment for depression?” and responded either yes or no. Participants were also asked two questions about the number of people they personally knew who had “emotional or mental problems.” One question assessed for the number of people with such problems within the participant’s family, and the other for the number of people with such problems outside of the participant’s family. Similarly, participants were asked the number of people they personally knew, both within and outside of their families, who had sought treatment for emotional or mental problems. For this study, these data were dichotomized (knows no one versus knows ≥1 person).
The 32-item Depression Self-Stigma Scale (
14) was used to measure facets of depression self-stigma, including internalized stigma, stigmatizing experiences, treatment stigma, public stigma, and secrecy. The 12-item Multidimensional Scale of Subjective Social Support (
15) was used to assess perceived social support from family, friends, and a significant other.
Four binary logistic regression models were constructed, one for each of the four knowledge questions (knowledge of people with emotional or mental problems both within the family and outside of the family and knowledge of people who sought treatment for emotional or mental problems within the family and outside of the family), which were the main predictors in the models. For each model, the dependent variable was treatment seeking (have or have not sought treatment for depression), and one of the knowledge questions was the main predictor. Each model controlled for factors previously found to be associated with treatment seeking: age, gender, level of education, relationship status, employment status, living setting, stigma, and social support. Additionally, a similar model was constructed with all four predictors of interest entered simultaneously.
Results
A total of 73% of participants were female, mean±SD age was 32.2±12.5 years, and participants reported being from 44 different countries. They reported a mean education level of 15.1±3.6 years. A majority of participants (62%, N=147) reported having sought treatment for depression. Individuals who had sought treatment for depression were likely to be older than those who had not (t=−5.90, df=242, p<0.001). No other significant demographic differences were found between those who had and had not sought depression treatment (see online supplement).
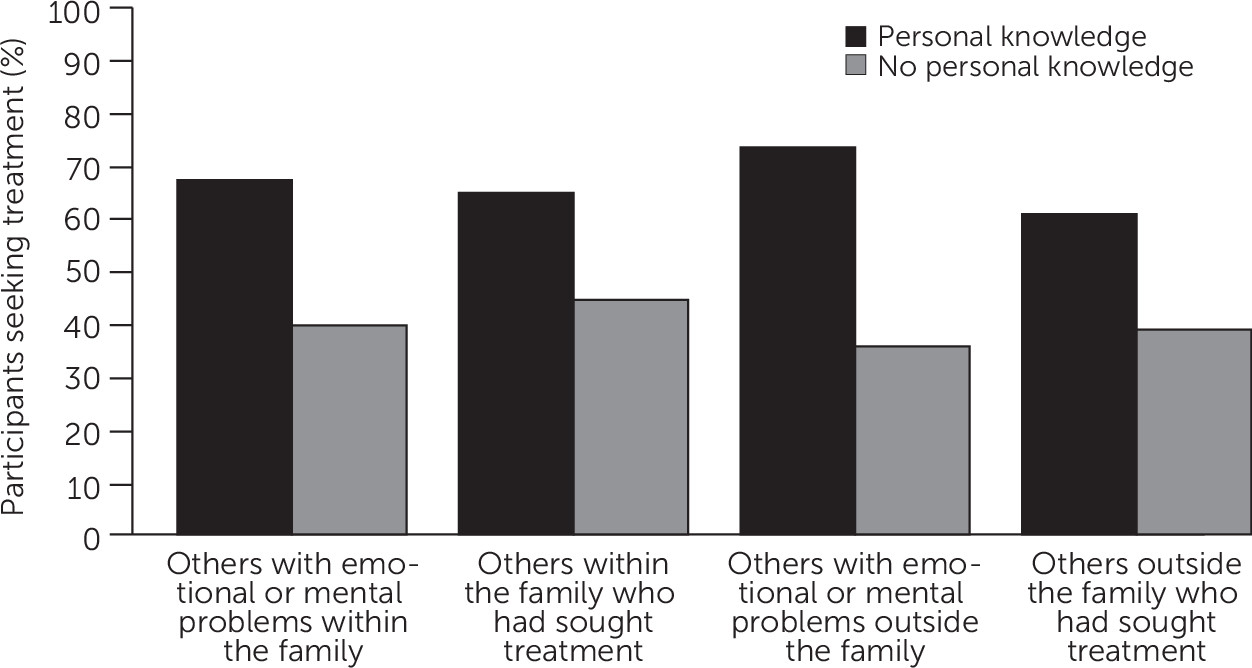
Results are illustrated in
Figure 1. Individuals who knew at least one person in their family with emotional or mental problems had higher odds of having sought depression treatment (Wald χ
2=12.67, df=1, p<0.001, odds ratio [OR]=3.66, 95% confidence interval [CI]=1.79–7.46). Similarly, knowing at least one person with emotional or mental problems outside of the family was related to higher odds of having sought treatment for depression (Wald χ
2=12.71, df=1, p<0.001, OR=4.98, 95% CI=2.06–12.03). In both models, age was positively related to greater odds of seeking depression treatment (within the family, Wald χ
2=19.65, df=1, p<0.001, OR=1.08, 95% CI=1.04–1.11; outside the family, Wald χ
2=22.88, df=1, p<0.001, OR=1.08, 95% CI=1.05–1.12). Other variables were not significant.
Knowing at least one person within one’s family who had sought treatment for emotional or mental problems was related to higher odds of treatment seeking (Wald χ2=14.62, df=1, p<0.001, OR=2.04, 95% CI=1.80–6.18). Similarly, knowing at least one person outside of one’s family who had sought treatment for such problems was related to higher odds of having sought treatment (Wald χ2=13.05, df=1, p<0.001, OR=3.43, 95% CI=1.76–6.68). Age was also positively related to treatment seeking (within the family, Wald χ2=14.75, df=1, p<0.001, OR=1.06, 95% CI=1.03–1.10; outside the family, Wald χ2=19.40, df=1, p<0.001, OR=1.07, 95% CI=1.04–1.11). Women had higher odds of having sought treatment compared with men (within the family only, Wald χ2=4.24, df=1, p<0.05, OR=2.04, 95% CI=1.04–4.00).
When knowledge variables were entered into the model as simultaneous predictors, the only knowledge variable associated with higher odds of having sought treatment was knowledge of at least one person within the family who had sought treatment (Wald χ2=4.83, df=1, p<0.05, OR=2.22, 95% CI=1.09–4.52). Age was likewise associated with treatment seeking (Wald χ2=15.44, df=1, p<0.001, OR=1.07, 95% CI=1.03–1.11).
Discussion and Conclusions
Our findings suggest an association between personal knowledge of others with emotional or mental problems or of others who had sought treatment for them and likelihood of seeking treatment for depression. Furthermore, the association of treatment seeking and personal knowledge of someone who had sought treatment for emotional problems specifically within the family appears especially important. Depression is a heritable illness (
1,
10), and it is possible that individuals growing up in a family with a history of emotional problems are better able to recognize the symptoms and have more knowledge of treatment options. If future research identifies a causal link between these factors, it may suggest that normalizing social influences positively affects treatment-seeking behavior.
Past research suggests that such a causal link is possible. Improving mental health literacy can positively affect treatment-seeking attitudes and behavior (
7,
9). Knowing others with mental health problems may improve mental health literacy by enhancing recognition of depressive symptoms. Likewise, knowing someone who has sought treatment may add to knowledge of available treatments and increase the acceptability of seeking treatment.
Importantly, the observed associations between treatment seeking and knowing others with mental health problems or those who had sought treatment for them were detected even when controlling for both known predictors of treatment seeking and for factors related to personal knowledge of others, such as social support. Theorists have previously suggested the importance of social networks for treatment seeking (
16), mainly in the context of encouraging individuals to seek care. Our findings suggest that mere personal knowledge may carry unique importance for treatment seeking beyond other well-studied social factors, such as social support and perceived stigma. Indeed, aside from age, which was expected to positively relate to past treatment seeking because older age allows for more time to seek treatment for depression, personal knowledge was the sole consistent predictor of greater odds of treatment seeking. Consistent with prior research (
7), one of the four models showed that women were more likely than men to have sought treatment.
This study had several limitations. Because our findings were correlational, it is unknown whether treatment seeking was the result of or a precursor to personal knowledge of others with mental health issues. It is possible that treatment seeking leads to increased recognition of emotional or mental problems in others or that people receiving treatment are more likely to meet others who are receiving treatment. It is also possible that those who have sought treatment may speak more openly about their experiences, leading others to speak more openly about their own experiences. Participants were recruited from an Internet-based depression screening study, which may have excluded individuals with lower socioeconomic status, those who were unable to use the Internet, or those who were uninterested in or unaware of their depression. Although our sample represented numerous countries, the results may not generalize to all populations. Cultural differences that may influence attitudes toward mental illness and treatment seeking were not analyzed in this study.
The results of this study suggest that knowing others with mental problems or those who had sought treatment for such problems is strongly related to treatment seeking among individuals with depression. Future research should investigate whether this relationship is causal and if so, the direction of this relationship. If this relationship is found to be causal, encounter-based interventions can be developed for individuals at risk for depression, wherein they may meet others who have received treatment. Encouraging the disclosure of one’s mental health treatment to others may serve to normalize treatment and, consequently, reduce societal stigma. In addition, to the extent that cultural norms and attitudes are likely to affect treatment-seeking behavior, determining whether the associations we have observed generalize to specific populations would be valuable. Given the pervasive undertreatment of depression, with fewer than half of individuals with depression receiving care (
3), any effort to increase treatment seeking would benefit public health and help reduce suffering among individuals with depression.
Acknowledgments
The authors gratefully acknowledge the Center for Health and Community for providing office space and additional resources and the contributions of research assistants and participants.