Suicide is a major public health burden, with over 6,000 deaths in the United Kingdom annually (
1). Over 90% of people who die by suicide may have had a psychiatric disorder at the time of their death (
2), and over one-quarter had been in contact with mental health services in the preceding year (
3). Effective treatment of psychiatric disorder may therefore be a key issue in suicide prevention (
4), and long-term pharmacological treatments such as lithium (
5) and clozapine (
6) are known to reduce suicide risk among patients with severe mental illness. Data on antidepressants are more equivocal: evidence suggests increased suicide risk in the early phase of treatment among young people (
7), but on balance, antidepressant treatment probably prevents suicide deaths (
8). In addition, psychological treatments such as cognitive-behavioral therapy (CBT) have the potential to reduce suicidal thoughts (
9).
Previous work has examined the “treatment gap” (i.e., the proportion of people with an illness who do not receive the treatment they need) as a measurement of health care (
10). Efforts to close this gap among people with mental, neurological, and substance use disorders have centered on access to services (
11) rather than on the psychotropic drugs received (
12). Furthermore, little is known about how prescribed treatment is related to medication adherence prior to suicide among people with mental illness, yet studies have shown that adherence to pharmacological treatment may be associated with a 33% lower risk of suicide compared with nonadherence or inadequate treatment (
13).
In England, the National Institute for Health and Clinical Excellence (NICE) provides guidance on best practice in the treatment of mental illness with pharmacological and psychological treatment. Similar clinical practice guidelines have been developed by the American Psychiatric Association and the European Psychiatric Association. However, evidence on the extent to which recommended treatment guidance is followed by clinicians is insufficient, and data suggest that some patients are untreated for their mental illness (
14,
15).
Further research is needed into the role of treatment among patients with psychiatric disorder who die by suicide. With their proximity to mental health services, these individuals may be the group most amenable to intervention. To our knowledge, no recent work has examined levels of treatment prior to patient suicide nor adherence levels in relation to specific psychiatric diagnoses. In this study, we therefore aimed to quantify the level of treatment in a population of people who died by suicide and who had been in recent contact with mental health services in England and Wales. Our objectives were to describe the levels of treatment prior to suicide among patients with different psychiatric disorders, to delineate levels of nontreatment due to nonprescription and nonadherence, and to explore the factors associated with receipt of treatment.
Methods
Participants and Setting
Data were collected as part of the National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH). Data collection comprised three steps: the collection of a comprehensive national sample of suicides from the Office for National Statistics, identifying those who had been in contact with mental health services in the 12 months prior to death (referred to as “patient suicide deaths”) from administrative contacts in each mental health organization, and collecting clinical information via a questionnaire sent to the clinician responsible for the patient’s care (as identified by the administrative contact at the health service organization). The questionnaire covered sociodemographic characteristics; suicide details; clinical history; and clinical care, including type of prescribed medications, receipt of psychological therapy (e.g., CBT, group therapy), and nonadherence to medication in the month before suicide. The rates of completion and return of the questionnaires by clinicians were high, with at least 95% return rates in almost all specialist mental health services and across all years.
All patient deaths in England and Wales that occurred between January 1, 2001, and December 31, 2016, with a conclusion at inquest of suicide or undetermined death formed the study sample. Suicide research in the United Kingdom conventionally includes deaths with open conclusions in order to avoid underreporting or misclassification of suicides (
16). Other inclusion criteria were patients who had received a primary diagnosis at last contact with services of schizophrenia and other delusional disorders (hereafter referred to as schizophrenia), bipolar affective disorder, depression, or anxiety disorders (including anxiety, phobias, panic disorder, posttraumatic stress disorder, and obsessive compulsive disorder). This information was collected from the questionnaire completed and returned by the treating mental health team and comprised clinical diagnoses based on
ICD-10 categories (equivalent to
DSM-5 criteria).
These diagnoses were selected because they are among the most common psychiatric disorders and have existing recommended treatment guidelines in the United Kingdom. We did not include personality disorder because NICE guidelines relate only to borderline or antisocial personality disorder and the NCISH questionnaire does not distinguish among subtypes. We also excluded substance use disorders because, in the United Kingdom, many patients with these conditions are not cared for by mental health services but by individual or private health care providers. NCISH received ethical approval from the North West Research Ethical Committee and has approval under Section 251 of the National Health Service Act 2006 for the collection of patient identifiable data.
Recommended Treatment
The definition of “recommended medication” for each disorder was based on NICE guidelines. We included major drug categories only rather than treatments that might be used for few patients in specialist settings. For depression, included categories were antidepressants (selective serotonin reuptake inhibitors [SSRIs], tricyclics, and “other” antidepressants) and lithium; for schizophrenia, oral (first-generation and second-generation) or depot antipsychotics; for bipolar disorder, oral or depot antipsychotics, antidepressants, lithium, and other mood stabilizers; and for anxiety disorders, SSRIs and other antidepressants. We also included psychological interventions that are recommended by NICE, such as CBT, in the treatment of each of the main diagnoses.
Main Outcome Measures
We first assessed the number of patients within each diagnostic group who were receiving relevant treatment. For those who were not receiving treatment, we identified those who had not been prescribed the treatment and those who had been prescribed the treatment but had not been adherent.
Statistical Analysis
The clinical and sociodemographic characteristics investigated in relation to treatment receipt were selected a priori and based on previous research (
17). These were age; gender; unemployment; black, Asian, and minority ethnic (BAME) group membership; living alone; imprisonment; history of self-harm; comorbid personality disorder; history of alcohol or drug misuse; and comorbid physical illness. Prevalence of specific mental disorders, description of treatment received, and extent of undertreatment were analyzed by using descriptive statistics, presented as frequencies and proportions. In general, valid percentages were used (i.e., if a response was missing, it was excluded from the analysis of that item). We assumed that prescribed treatment would be known to the clinical teams, so if there was no record of treatment, we assumed no treatment had been prescribed. Univariate analysis (chi-square tests and odds ratios [ORs] with 95% confidence intervals [CIs]) was used to examine the patient characteristics associated with receiving treatment. Stepwise multivariate analysis, adjusted for main primary diagnosis, was then performed to determine independent predictor variables for treatment receipt, and p values less than 5% were considered significant. Analyses were conducted with Stata, version 15.1 (
18).
Results
Between 2001 and 2016, a total of 77,698 suicides occurred in the general population in England and Wales, of whom 20,346 (26.2%) were patients (i.e., had been in contact with mental health services in the 12 months prior to death). Of the patients, 19,967 (98.1%) received a primary psychiatric diagnosis at the time of death. Two-thirds (N=12,909, 64.7%) had one of the main diagnoses that were the focus of this study: depression (N=6,832, 52.9%), schizophrenia (N=3,409, 26.4%), bipolar affective disorder (N=1,807, 13.9%), or an anxiety disorder (N=861, 6.7%). These patients were included for analysis. The remaining 35% (N=7,058) of patients who were excluded received other diagnoses, including unspecified personality disorder, alcohol or drug dependence/misuse, dementia, and adjustment disorders.
Two-thirds of the sample were male (N=8,346, 64.7%) and the median age was 48 years (range 10–96). A majority were unmarried or not cohabiting (N=8,520, 67.3%), lived alone (N=5,593, 43.3%), or were unemployed (N=4,838, 37.5%). A total of 904 (7.3%) patients had a history of imprisonment. Previous self-harm (N=8,184, 64.8%), alcohol misuse (N=4,578, 36.4%), and drug misuse (N=3,379, 26.9%) were common features of patients who died by suicide.
Treatment of Mental Illness
Of the 12,909 patients who died by suicide, 9,644 (74.7%) were receiving recommended pharmacological treatment, and 2,120 (16.4%) were receiving psychological treatment at the time of death. Psychological treatment was more common among patients with anxiety disorders (N=231, 26.8%) and depression (N=1,318, 19.3%) than among those with bipolar affective disorder (N=236, 13.1%) and schizophrenia (N=335, 9.8%).
Levels of Treatment and Adherence
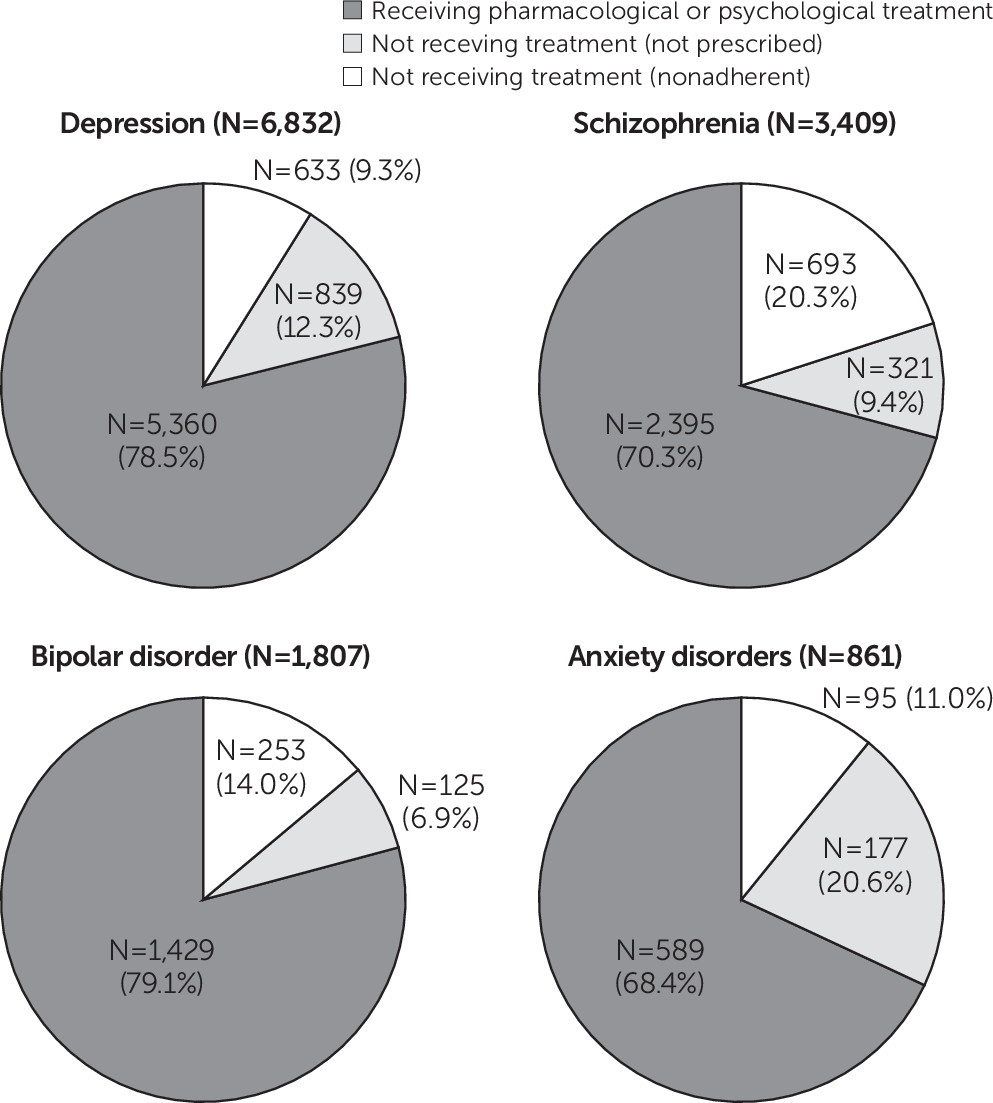
In total, 3,136 (24.3%) patients had not received relevant medication or psychological treatment prior to death. The relative proportions varied by diagnosis; fewer patients with anxiety disorders (N=272, 31.6%) or schizophrenia (N=1,014, 29.7%) received treatment compared with patients with bipolar disorder (N=378, 20.9%) or depression (N=1,472, 21.5%) (
Figure 1). Furthermore, 1,463 (11.3% of all patient suicide deaths) had not been prescribed the recommended treatment, and 1,673 (13.0%) had not adhered to the treatment. The highest proportion of patients not prescribed treatment was found among those with anxiety disorders (N=177, 20.6%) and depression (N=839, 12.3%), and the lowest among patients with bipolar disorder (N=125, 6.9%) and schizophrenia (N=321, 9.4%) (
Figure 1).
In terms of adherence, patients with schizophrenia (N=693, 20.3%) and bipolar disorder (253, 14.0%) were less often adherent to treatment compared with those with anxiety disorders (N=95, 11.0%) and depression (N=633, 9.3%) (
Figure 1). Adverse psychotropic side effects from medication were more commonly reported among patients with schizophrenia (N=448, 13.9%) and bipolar disorder (N=176, 10.3%) than among those with anxiety disorders (N=67, 8.7%) and depression (N=439, 7.0%).
Factors Associated With Receipt of Recommended Treatment
Being under age 40, male gender, unemployment, and living alone were demographic characteristics associated with a decreased likelihood of receiving treatment (
Table 1). Patients from a BAME group were also less likely to receive treatment, although this association was no longer statistically significant after adjustment for psychiatric diagnosis. Those with a history of alcohol or drug misuse, imprisonment, or a comorbid personality disorder were less likely to have received treatment. Medication side effects were associated with a large decrease in the odds of receiving treatment but were relatively uncommon compared with other factors we considered. In contrast, patients with a comorbid physical illness were more likely to receive treatment. We found no association between self-harm and receiving treatment.
We examined whether the associations differed when separately considering those not receiving treatment due to nonadherence or nonprescription. The findings for the nonadherent group were similar to the findings for the sample as a whole. The findings for the nonprescribed group were also similar to the findings of the sample overall, except that living alone and having a comorbid personality disorder were no longer associated with a reduced likelihood of treatment receipt (AOR [adjusted odds ratio]=1.03, 95% CI=0.92–1.16 and AOR=1.02, 95% CI=0.85–1.23, respectively). Furthermore, as might be expected, medication side effects were less strongly associated with nontreatment (AOR=0.87, 95% CI=0.68–1.13).
Factors that were significantly associated at the univariate level with whether treatment was received overall were entered into a multivariate logistic model (
Table 2). Being under age 40, unemployment, living alone, psychotropic side effects, comorbid personality disorder, and a history of drug misuse were all independently associated with a decreased likelihood of receiving treatment. These associations remained statistically significant after adjustment for diagnosis.
Discussion
Our results suggest that in a clinical sample of patients who died by suicide and had been in recent contact with mental health services, not all were receiving appropriate pharmacological or psychological treatment at the time of death. Levels of nontreatment ranged from around 20% among patients with depression or bipolar affective disorder to around 30% among those with schizophrenia or anxiety disorders. The reasons for not receiving treatment were a combination of either not being prescribed treatment or not adhering to it, and the relative contribution of these factors varied by diagnosis. Levels of nonprescription were highest for patients with anxiety and depressive disorders, while levels of nonadherence were highest for patients with schizophrenia and bipolar disorder. We found that certain patient characteristics were associated with undertreatment, including demographic (gender, age), social (living alone, unemployment), behavioral (substance misuse), and clinical (comorbid personality disorder, medication side effects) factors.
Although our study reported on a national case series of patient suicide deaths, the findings should be considered in the context of several methodological limitations. The case-series methodology prevents examination of causal relationships between clinical factors and treatment receipt. Clinical information was collected retrospectively on the basis of the account of the clinician involved, with diagnoses based on
ICD-10 criteria and not standardized interviews. However, clinicians used both case notes and personal knowledge of the patient to provide information, and the validity of NCISH questionnaire data has been established (
19). Missing treatment data were interpreted to mean the patient had not received treatment. However, the health care team likely would have knowledge of relevant prescribed treatment. We restricted our analysis to NICE-recommended treatment so we could investigate treatment received by patients with the most common psychiatric diagnoses in comparison with national guidelines. We therefore did not include other treatments recommended in national and international guidelines, such as those from the British Association for Psychopharmacology or the American Psychiatric Association. We were unable to examine treatment specifically received for comorbid substance use disorders, although this treatment would apply to only a minority of patients in our sample. A lack of available information prevented a detailed examination of nonpharmacological treatments and adherence prior to suicide, and we could not break down treatment by modality or number of treatment sessions.
Our focus in this study was on a clinical sample, in particular patients in recent contact with mental health services before death. Our diagnostic inclusion criteria meant that 65% of this sample were included in the study. Our definition of recent contact as contact within the 12 months prior to death meant we could not generalize findings to all psychiatric patients; this time frame was selected because of proximity of care and the potential for services to intervene and prevent suicide. Our sample represented 17% of all general population suicide deaths during the study period. We did not examine treatment receipt among people who had died by suicide and who were not in contact with secondary mental health services, many of whom likely had been treated solely by their general practitioner. This population warrants further study.
One of the assumptions underlying the study rationale was that pharmacological and psychological treatment helps to prevent suicidal behavior, and the more people who are being actively treated the better. The latter assertion in particular might be regarded as contentious, given international concerns about overprescription and the medicalization of normal human emotion (
20,
21). Moreover, this study was not designed to explore the potential positive effects of patient autonomy in treatment selection; for some patients, nonadherence may be an active choice taken after careful consideration.
We found that nonadherence levels were higher among patients with more severe mental disorders. Factors known to affect nonadherence in clinical populations include characteristics of the medication itself (e.g., extrapyramidal symptoms or weight gain) (
22) and sedation (
23). We found that medication side effects were associated with nonreceipt of treatment, although these were less common in our sample than some of the other factors examined. Nonadherence may also be a direct consequence of the illness itself, for example during manic episodes among patients with bipolar disorder (
24), as well as a result of personal choice by the patient (
25). Although self-harm might be expected to influence nonreceipt of treatment (e.g., fewer people with a history of self-harm being prescribed psychotropic medication), our findings did not show this association. This finding could reflect the clinical severity of the overall sample, which comprised only patients recently treated in specialist mental health services.
Our finding that certain patient characteristics influenced the receipt of treatment support a recent Adult Psychiatric Morbidity Survey (
26), which found fewer men than women and younger than older people receiving medication and psychological therapy. This finding may reflect lower levels of service contact in these groups. Inequalities in access to treatment for BAME groups, including lower rates of prescribed antidepressants in primary care (
27) and fewer individuals receiving psychological therapies (
28), have also been previously demonstrated. We found that a history of alcohol and drug misuse was an important predictor of nonreceipt of treatment. The impact of comorbid substance misuse on adherence has been studied extensively, and conclusions are consistent with prior research in showing an association with poorer treatment outcomes (
29).
Conclusions
Our findings suggest that mental illness may be undertreated among patients who have been in recent contact with specialist mental health services prior to suicide. Undertreatment is likely to be even higher among people who have not been in contact with specialist care (
26). Previous research has shown that variables such as living alone (
30), male gender, and a history of alcohol and drug misuse (
31) can be associated with undertreatment. Part of the impact of these factors may be a lack of access to services (e.g., young men being reluctant to seek psychiatric help) (
32). However, our findings indicate that even when certain groups are in contact with services, they may still be less likely to receive treatment, supporting a recent review of the challenges in health equity for marginalized individuals (
33).
Clinicians should be aware that undertreatment can result from a lack of recommended prescribing as well as nonadherence and that the relative importance of these factors varies by psychiatric diagnosis. For patients with schizophrenia and bipolar affective disorder, improving adherence may be more important, whereas for patients with anxiety disorders and depression, strategies to improve recognition of symptoms and treatment may be helpful. Interventions to improve adherence include enhancing the therapeutic alliance (
34) and promoting positive attitudes toward medication (
35). Of course, appropriate and targeted prescribing of treatment can also play a role in enhancing adherence (
36), as can improving patient engagement and supporting informed choice (
37). Motivational interventions, such as electronic reminder systems and motivational enhancement therapy, may be particularly useful for younger patients, those living alone, and those at risk of relapse (
38,
39). We have previously identified 10 ways to potentially improve safety for mental health patients (
3). Some of these may function by ensuring that patients get the treatments they need. For example, outreach teams can help ensure treatment receipt and engagement, and specialist services for people with co-occurring disorders can focus on treatment for underlying mental illness as well as substance misuse. Individualized treatment plans with involvement of the family may also help in ensuring that we provide the best treatment we can and minimize the risk of suicide for our patients.