Effectiveness of Suicide-Focused Psychosocial Interventions in Psychosis: A Systematic Review and Meta-Analysis
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Methods
Search Strategy
Study Selection
Data Extraction
Quality Assessment
Statistical Analysis
Moderator Analysis via Meta-Regression
Results
Search Results, Study Characteristics, and Quality of Studies
| Study | Samplea | Demographic factorsb | Control descriptionc | Intervention providers | Treatment descriptiond | Suicide outcomee | Psychosis and suicide measurementf | Setting and duration of psychosisg |
|---|---|---|---|---|---|---|---|---|
| Agius et al., 2007 (29)h | T=40; C=40 | Age, 24.5; female, 30%; white, 42% | TAU | Multidisciplinary team (psychiatrists, nurses, social workers, and psychologists) | Early psychosis intervention, including assertive treatment and individual and family psychoeducation for 3 years; frequency and session length, NR | SA | BPRS, PANSS | NHS; first-episode psychosis |
| Albert et al., 2017 (30)h | T=197; C=203 | Age, 25.6±4.3; female, 46.2%; race-ethnicity, NR | TAU | Interdisciplinary team (psychiatrists, psychologists, nurses, social workers, physiotherapists, and vocational therapists) | SEI program entitled OPUS, includes modified assertive treatment, family involvement, and social skills training for 5 years; sessions and duration per week, NR | SI | SCAN 2.1, SAPS, SANS, SI assessed by a single self-report item | CBMH; first-episode psychosis |
| Bateman et al., 2007 (31) | T=46; C=44 | Age, 39; female, 33%; white, 87% | Befriending intervention (providing company and general conversation on neutral topics) | Therapist (not defined) | CBT for 20 individual sessions over 9 months | SI | CPRS | CBMH; chronic schizophrenia (≥14 years) |
| Chan et al., 2015 (32)h | T=148; C=148 | Age, 21.9±3.1; female, 49.7%; Chinese, 94.5% | TAU | Teams of psychiatrists, clinicians (psychologists), and case managers (social workers) | EASY program for 2 years, followed by case management and outpatient treatment in year 3 | SA, SD | PANSS, SANS, CDSS | CBMH; first-episode psychosis |
| Chan et al., 2018 (33)h | T=617; C=617 | Age, 21.2±3.4; female, 48.5%; Chinese, 94.5% | TAU | Clinicians (not defined) | EASY program for 2 years; frequency and session length, NR | SA, SD | CGI-SCH | CBMH; first-episode psychosis |
| Chen et al., 2011 (34)h | T=700; C=700 | Age, 21.1±3.4; female, 48.6%; race, NR | TAU | Teams of clinicians (psychologists) and case managers (social workers) | EASY program for 3 years; frequency and session length, NR | SA, SD | CGI-S | CBMH; first-episode psychosis |
| Cunningham Owens et al., 2001 (35) | T=61; C=53 | Age, 21.1±10.6; female, 48.6%; race, NR | TAU | Psychiatrist | Intervention package with multiple components, including educational video and booklets | SI | ITAQ | HIO; second- or later-episode schizophrenia |
| Färdig et al., 2011 (36)h | T=21; C=20 | Age, 40.38±6.6; female, 38%; race, NR | TAU | Mental health practitioners (details NR) | IMR program, including psychoeducation, social skills training, relapse prevention, behavioral tailoring for treatment adherence, and coping skills training for managing stress and symptoms; 40 60-minute sessions of mixed interventions over 36 weeks | SI | PECC | MHC; psychosis duration, NR |
| Kasckow et al., 2016 (37)h | T=25; C=26 | Age, 51.1±11.5; female, 4%; white, 76% | TAU | Social workers and mental health nurses | 10 15-minute weekly assessment sessions over 12 weeks, accompanied by daily telehealth monitoring via Health Buddy program | SI | BSSI, SAPS, SANS | HIO; recently admitted VA inpatients with psychosis; duration, NR |
| Moritz et al., 2018 (38) | T=46; C=46 | Age, 36.91±1.9; female, 54.3%; race, NR | Cognitive training program (CogPack) | Psychologists | MCT for 12 sessions over 6 weeks | Details NRi | MINI, PANSS, PSYRATS | HIO; psychosis duration, NR |
| Nordentoft et al., 2002 (39)h | T=121; C=106 | Age, 27.0±6.3; female, 39.9%; race, NR | TAU | Psychiatrist, psychologist, nurse, vocational therapist, and social worker | Integrated treatment offered for 2 years, including assertive community treatment, antipsychotic medication, psychoeducational family treatment, and social skills training over 2 years | SI, SP, SA | SAPS, SANS, SCAN 2.0 | CBMH; first-episode psychosis |
| Peters et al., 2010 (40)h | T=36; C=38 | Age, 36.9±9.8; female, 37.8%; race, NR | Waitlist | Nonexpert cognitive-behavioral therapist for psychosis, full-time roles: psychologist, nurses, or psychiatrist | 6 months of CBT for psychosis by CBT therapist under supervision; 16 weekly individual sessions of up to 1 hour per session | Details NRj | BSI | CBMH; median 6 years of schizophrenia diagnosis |
| Power et al., 2003 (41) | T=31; C=25 | Age, NR; gender, NR | TAU | Mental health practitioners (details NR) | 8–10 sessions of cognitive therapy over 10 weeks | SI, SA | SIQ, SIS, RFL-24, BPRS, SANS | MHC; psychosis duration, NR |
| Tarrier et al., 2006 (42) | T=101; C=102 | Age, NR; female, 30%; white, 88.7% | TAU | 3 clinical psychologists and 2 nurse therapists | 15–20 hours of treatment within 5 weeks of admission, plus “booster” session at 2 weeks and at 1, 2, and 3 months after the initial treatment | SA | HoNOS | HIO; first-episode and early schizophrenia; first admission or within 2 years of first admission |
| Tarrier et al., 2014 (3)h | T=25; C=24 | Age, 34.9±13.1; female, 36.7%; white, 85.7% | TAU | Psychologists | CBT for 24-sessions over 12 weeks | SI, SP | ASIQ, BSSI, SPS, PANSS, PSYRATS | CBMH; psychosis duration, NR |
| Turkington et al., 2002 (43)h | T=257; C=165 | Age, 40.47±.35; female, 22.9%; white, 88.9% | TAU | Community psychiatric nurses | CBT for 6 60-minute sessions over 2 or 3 months | SI | SCS, CPRS | CBMH; psychosis duration, NR |
Overall Pooled and Subgroup Meta-Analysis Result
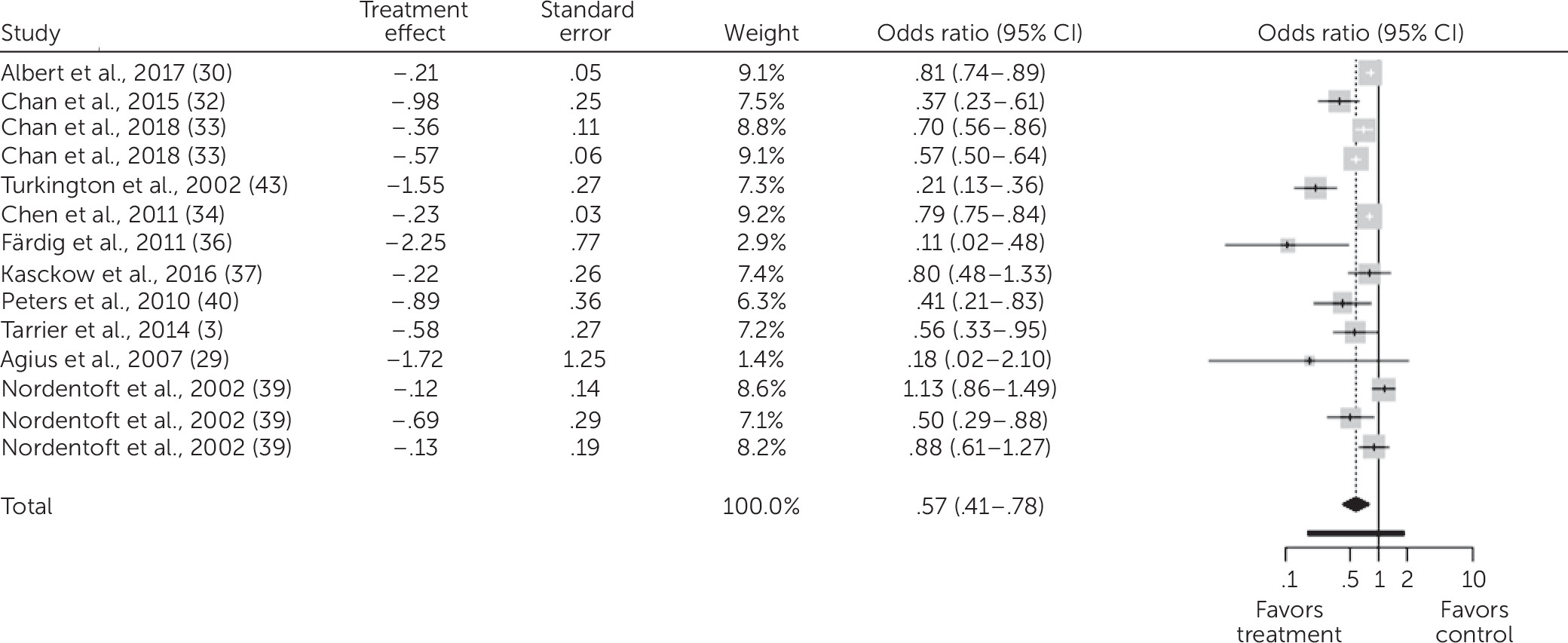
Exploratory Moderator and Subgroup Analysis
Discussion
Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 316.31 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).