That access to psychiatric beds is a topic of national urgency is an understatement. Emergency physicians regularly issue grim reports on the boarding of psychiatric patients in emergency departments (EDs), and states are being sued, sometimes repeatedly, over bed waits (
1). In the academic literature and mass media, psychiatric bed shortages are often blamed for homelessness, mass incarceration, mass violence, and a host of other individual and societal consequences. At times, it can appear that there is no poor outcome or social system failure that cannot be attributed to reductions in the number of psychiatric beds—in state hospitals in particular—and the trend known as deinstitutionalization.
The National Association of State Mental Health Program Directors (NASMHPD) is a membership organization of the state executives responsible for the nation’s public mental health delivery system, including state hospitals. In the current environment, leaders of the organization are frequently asked questions such as the following: How many psychiatric beds exist in the United States, where are they, who operates them, and whom do they serve? How many psychiatric beds does the nation need, of what kind, and where? What is the quality of care in these inpatient settings, and what are the outcomes such settings produce for patients, staff, and the public? Why do states continue eliminating psychiatric beds (or why are they not creating more) if these beds are in short supply? To what degree can homelessness, mass incarceration, violence (including suicide and homicide), substance use disorder prevalence, and a host of other clinical, social, and public health issues be attributed to the number of psychiatric beds available?
Some progress toward answers is being made. By early 2019, a total of 23 states were participating in an initiative funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) and NASMHPD to create a comprehensive registry of psychiatric crisis intervention beds for people with serious mental illness (
2). The effort does not yet extend to all the other bed categories that serve psychiatric patients (e.g., child and adolescent, adult and geriatric, forensic, public, and private beds), nor is there a comparable initiative under way for a national database. What’s more, no evidence-based target exists for the number of psychiatric beds needed at each level of care, either in the United States or elsewhere. A consensus definition of “psychiatric bed” would make answering any of these questions easier, but it does not exist. Meanwhile, determining causality between deinstitutionalization and social trends that developed around the same time frame (e.g., increased incarceration and homelessness) is complicated by so many confounding factors that causality is never beyond debate. Unsurprisingly, under these circumstances, questions still far outnumber answers.
As crucial as these questions and their answers are, what is too often lost in the clamor surrounding them is the reality that 24/7 inpatient care represents only a single component of a well-functioning continuum of care for any life-threatening health condition. We readily acknowledge that patients with cancer, stroke, congestive heart failure, and many other medical conditions may require hospitalization at some point, but we do not expect hospitals to provide all the care required for those patients to survive and recover. Indeed, the U.S. health care system generally has moved to a model wherein the swiftest possible return to the patient’s natural environment is prioritized. Yet, although the total number of hospital stays for all causes in the United States fell by 6.6% from 2005 to 2014, hospital admissions for mental health and substance use conditions rose by 12.2%—the only category of hospitalization that increased in the time period (
3).
Prior to the late 20th century, the U.S. mental health system consisted largely of psychiatric hospitals operated by the individual states. However, the era of giving state mental health authorities the keys to the system is over. Today, multiple entities influence, fund, oversee, provide, or participate in mental health service delivery and recovery, including private providers; public agencies serving specific subpopulations; managed care organizations and other insurers; courts and other justice stakeholders; corrections systems; community partners, such as faith-based organizations; policy makers and budgeters at every government level; special interest advocacy groups; and, of course, individuals living with serious mental illness themselves.
The opportunities and options for improving mental health care have perhaps never been greater. The Mental Health Parity and Addiction Equity Act, Comprehensive Addiction Recovery Act, 21st Century Cures Act, and other federal and state initiatives have been enacted, largely in response to growing recognition by the public and policy makers that inefficient and ineffective mental health care delivery is costly and that discriminatory practices produce poor outcomes for a large and vulnerable population. Nonetheless, consensus on priorities, strategies, and steps to improve mental health care has proven elusive. In this debate, few subjects have been as fraught as the issue of psychiatric beds.
Issues of Terminology
Despite cries for more psychiatric beds, the term has no commonly recognized definition. In the most basic sense, a bed is a place where an individual sleeps at night, but that definition is related more to housing than to treatment. After all, jails report bed numbers, too. In the behavioral health world, beds were once defined principally by their location inside state hospitals. The term “psychiatric bed” frequently continues to be used interchangeably with “state hospital bed,” and it is also used generically, as if all beds serve the same purpose. Yet most mental health beds in the United States today are located outside state hospitals, and they serve a variety of purposes for distinct subpopulations—critical distinctions that are often lost in the larger narrative about beds (
4).
Beds that provide round-the-clock psychiatric care to populations once served almost exclusively in state hospitals also now exist in university and community hospitals, charity and for-profit hospitals, private facilities dedicated entirely to mental health care, and other configurations. Older persons with dementia who once were housed almost exclusively in state hospitals now are accommodated in a variety of community settings, such as nursing homes; similar shifts are seen in the child and adolescent behavioral health and welfare systems. A community might also be served by specialized inpatient beds that focus on populations such as persons with substance use or co-occurring conditions, traumatic brain injuries, eating disorders, obsessive-compulsive disorder, or other neuropsychiatric challenges. To further complicate matters, some settings have the dual purpose of providing treatment services and a place to sleep for those needing both, such as short-term residential treatment settings and supportive housing, a point that is often missed in the conversation about beds.
Beds where psychiatric care is delivered also exist completely outside psychiatric settings. For example, some psychiatric patients are treated in “scatter beds” located in hospital medical-surgical and pediatric units (
5), and a growing number of corrections systems operate beds designated for incarcerated individuals with mental illness, including youths in the delinquency system. Beyond inpatient beds altogether, step-down options, such as intensive outpatient treatment or day programming, may exist to provide additional supports to individuals with mental illness who reside and sleep at home.
Psychiatric beds and patients may also be differentiated by duration of stay. Crisis stabilization beds are typically designed for a level of care short of hospitalization and utilized for very brief stays (several hours to a few days). Transitional or respite beds in residential or other settings provide 24-hour nonmedical monitoring and significant supports and are typically utilized for a fixed or limited period following hospitalization. Long-term beds in group living environments, adult foster care settings, board-and-care facilities, nursing homes, and a variety of other settings are typically utilized for individuals with chronic mental illness who are not ready or able to reenter the community.
In addition to these differences, funding differentiates and complicates examination of psychiatric beds. When virtually all psychiatric beds were in state hospitals, they were often called “public” beds because they were funded by state budgets. In today’s world of managed care contracts and expanded Medicaid coverage, where psychiatric care in private settings may be provided through public insurance, the phrase “public bed” is antiquated, and even the notion of “publicly funded” can be problematic. For example, when a child-adolescent or adult bed in the psychiatric unit of a for-profit private hospital is occupied by a patient whose treatment is publicly insured by Medicaid or Medicare, is that a private or public bed? The lack of a shared language for discussing all these psychiatric bed models and the historic scarcity of comprehensive data about them have immeasurably complicated and obscured our understanding of the beds, their numbers, and their role in the continuum of psychiatric care.
Beyond terminology, philosophical differences also bedevil the beds conversation. More than 50 years after deinstitutionalization began, critics fear that bed expansion on any scale could precipitate a return to the 19th-century model of institutional care that peaked in 1955. At the same time, after 50 years of watching state hospital bed numbers inexorably shrink, proponents of more beds fear that beds numbers are already insufficient and will eventually disappear.
It is time to retire the extremes of both viewpoints. Three generations of pharmacological treatment development (
6) and federal laws and programs, such as Social Security Disability Insurance, the Americans With Disabilities Act, the Children’s Health Insurance Program and its 2009 reauthorization, the Individuals with Disabilities Education Act , and others, now ensure that individuals with chronic conditions and disabilities, regardless of income, will be integrated into society and are entitled to lives of inclusion. At the same time, a recognition that hospital beds continue to play a vital role in providing acute and chronic care for a segment of the population with serious mental illness at times of need is widespread (
7). This recognition has prompted some states and providers to reexamine bed numbers and has generated unprecedented support for repealing federal limits on Medicaid reimbursement to adult psychiatric facilities of more than 16 beds (the Institutions for Mental Diseases [IMD] exclusion). Halting bed closures has been another approach (
4).
Bed Types and Functions
Criminal Justice System Beds
Mental illness is global, but mental illness response is local, and whether a 911 call is made during a first psychotic break or a relapse, it triggers one of several response types reflective of the circumstances and local conditions. Circumstances that influence outcomes can include the individual’s behavior at the time; the state where the person lives and its laws, policies, and practices related to who can be held for psychiatric evaluation and where the person might go for evaluation; and the robustness of the community’s mental health services and their accessibility. In addition, factors such as the existence of emergency, crisis stabilization, inpatient, and recovery beds and personnel—even the training of local law enforcement in de-escalation tactics—can change the trajectory for the person involved in the crisis. Access to crisis stabilization centers and police drop-off sites, the availability of jail diversion programs for individuals with mental illness, and insurance status also can influence how the individual is routed after a 911 call is made.
Family caregivers of individuals with acute psychiatric symptoms and others in the community often call police under the assumption that law enforcement involvement will result in treatment for the crisis. This assumption has effectively led to law enforcement’s becoming the nation’s mental health first responders.
The response to such calls, however, is far from certain.
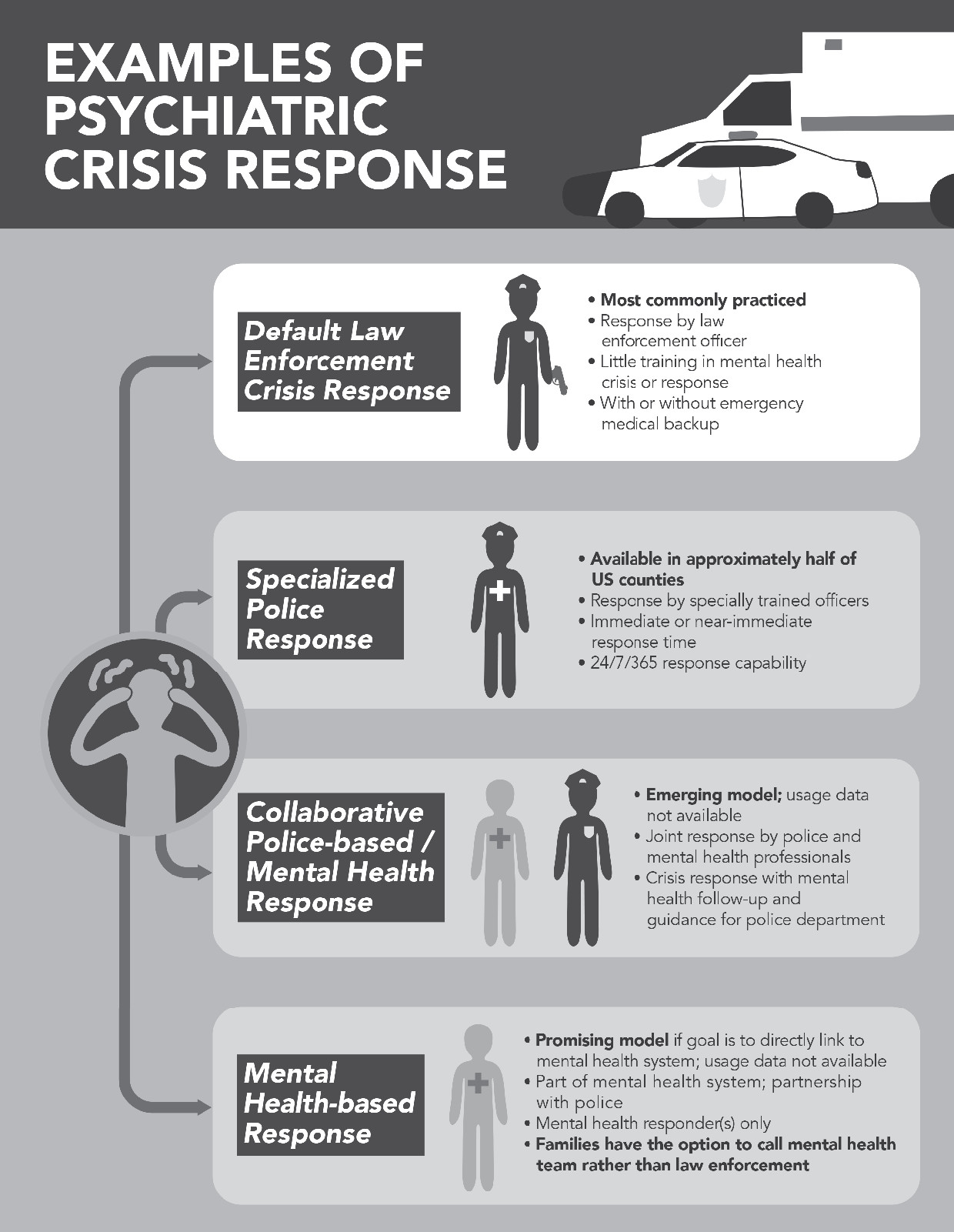
Figure 1 presents a graphic representation of examples of psychiatric crisis response. During the encounter, the individual’s risk of injury or death is 16 times greater than it is for a member of the public without serious mental illness (
8), and the risk of arrest is six times greater (
9). If the individual is taken into criminal custody, new uncertainties arise, including whether the defendant is released or jailed, given appropriate psychiatric treatment during incarceration, evaluated for criminal competency and where, referred for restoration of competency, and others. Any of these contingencies may invoke the need for some type of treatment bed.
When local practice depends heavily on state hospital beds for pretrial competency services and the number of detainees exceeds available beds, individuals end up waiting to receive those services. These “forensic bed” waits typically take place in jails, where wait times average weeks to more than a year in different states, and these waiting times have been increasing in many places (
10). States have been attempting to reduce or eliminate their bed waits, but waitlists remain common, and many states have been sued, sometimes repeatedly, or threatened with lawsuits over the situation (
1).
The sequential intercept model is a framework based on the premise that criminal justice involvement of individuals with mental illness can be reduced by identifying and redirecting them into treatment at various intercept points along the criminal justice continuum (e.g., during police encounters, during court proceedings, at jail and prison reentry, and while on community probation or parole supervision) (
11). A full continuum of options that appropriately supports individuals with mental illness is often what is missing to prevent or reduce criminal justice involvement at these intercept points.
Emergency Department Beds
When there is an incomplete continuum of care, both law enforcement and families also commonly turn to the EDs of their local hospitals for psychiatric crisis intervention. The demand this creates contributes to ED crowding and often results in psychiatric “boarding,” a practice in which psychiatric patients whose condition merits hospital admission are held in the ED because no inpatient bed is available to admit them.
The American College of Emergency Physicians (ACEP) has reported that 90% of hospital EDs board psychiatric patients (
12), with bed wait times averaging three times those of nonpsychiatric patients (
13). Bed waits can last days or even weeks, and, as with waits in jail, can lead to lawsuits, court orders, and costly settlements (
14). Studies of boarding patterns indicate that psychiatric patients who have the most extreme symptoms or are the most suicidal often wait the longest for admission or are discharged without care because of the difficulty of matching them to beds (
15).
ACEP for two decades has been proposing strategies to reduce ED crowding, but it has reported only “minor gains” from the efforts (
16). The intractability of the problem despite efforts by ACEP and other organizations and agencies reflects its complexity. Boarding is a symptom of needs and resources that are not balanced. These needs include a variety of factors, such as patient access to preventive and supportive services in the community that reduce the likelihood of crisis (e.g., assertive community treatment teams) (
17), hospital access to real-time information about where and what kinds of beds are available (e.g., psychiatric bed registries), the availability of alternatives to intensive treatment outside hospitals (e.g., crisis stabilization units in the community), and law enforcement training and practices that influence whether law enforcement encounters are de-escalated at the scene (e.g., crisis intervention teams). Other factors that present challenges to efficiently triaging and transferring individuals to appropriate alternative levels of care include governing state laws and criteria that influence the volume of involuntary mental health evaluations and hospital admissions initiated through EDs; the absolute number of beds available within the hospital or transport distance; the licensing and distribution of available beds (e.g., by gender, age, or purpose); and staffing resources, including the availability of qualified mental health professionals willing to treat the population in either the public or private sector.
Quality of care is another critical aspect of the ED bed challenges. Studies and surveys consistently find that patients in psychiatric crisis do not receive the same quality of health care in the ED as patients presenting with other medical conditions. Provider biases and prejudices that result in inferior interventions are reported (
18,
19). In psychiatric cases, misinterpretation and overinterpretation of confidentiality provisions of HIPAA often leave caregivers out of treatment discussions that typically include family members (
20). EDs underequipped to handle mental health emergencies may be even less prepared to expeditiously evaluate and place patients with comorbid conditions, such as substance use; intellectual-developmental disabilities, including autism; sensory issues, including deafness; and others (
17). “Emergency in the emergency room” is how more than a few observers have described the situation.
Changes in practice at any point on the continuum of care connected to crisis services can affect ED boarding dramatically. One 2017 study based on computer modeling found that adding a single half-time clinician during the 8 a.m. to 4 p.m. shift could cut average wait time to discharge by 35% and average wait time to admission by 13% (
21). Conversely, when Sacramento, California, closed an outpatient crisis stabilization unit and eliminated 50 of 100 inpatient beds in 2009, the number of ED visits requiring psychiatric consultation at the city’s university hospital tripled, and the average time that psychiatric patients spent waiting to be seen by a psychiatric clinician in the ED increased from an average of 14 hours to nearly 22 hours (
22).
The ED visit is another crossroads. What transpires there determines the patient’s next step along the continuum of care—or off it.
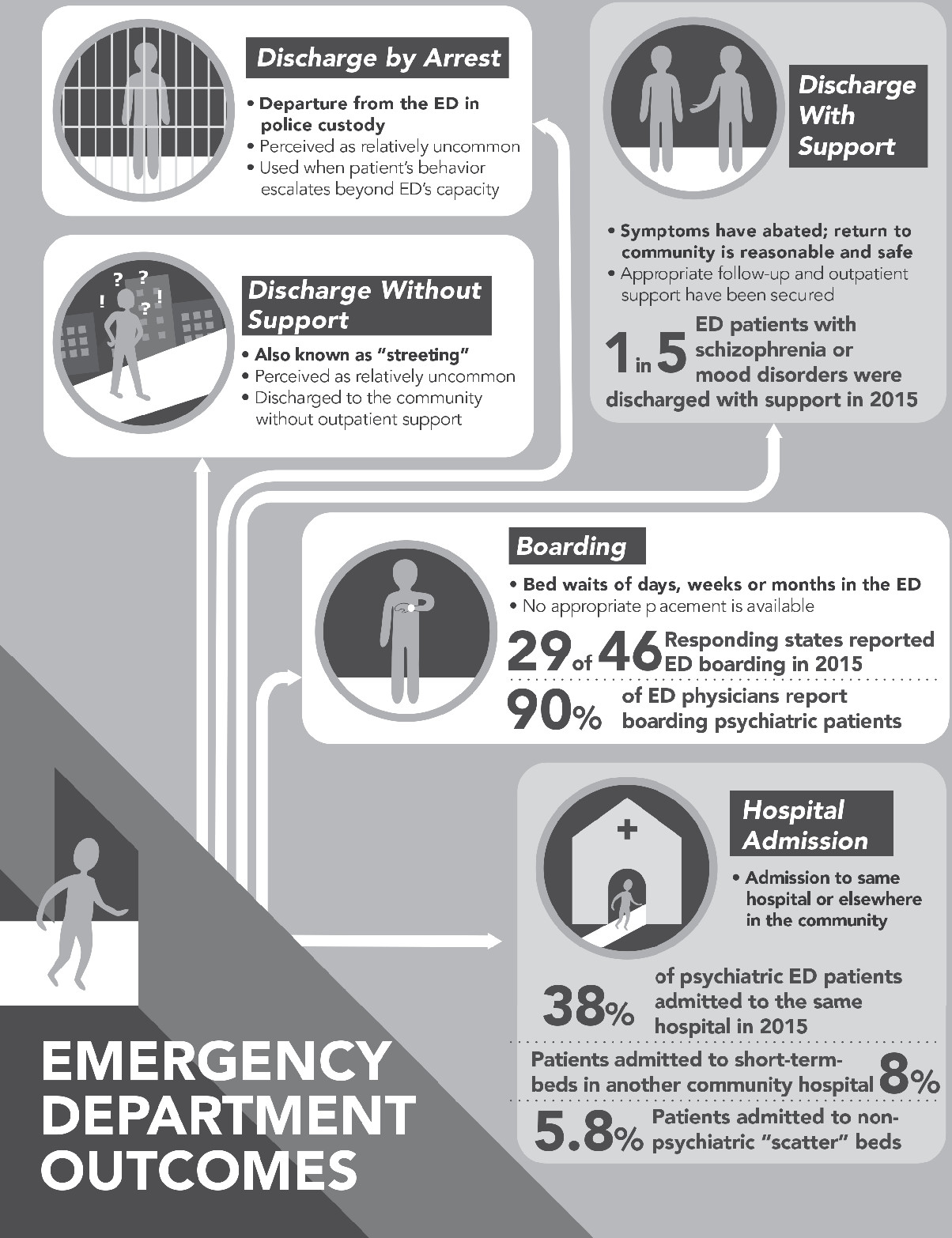
Figure 2 is a graphic representation of the most common ED pathways for psychiatric patients. As with arrival at the ED itself, the outcome that any individual patient experiences is a function of multiple factors: the gravity of the symptoms; the patient’s behavior; the availability of appropriate beds; the clinical assessment of the evaluator; the tenacity of the patient’s advocates, who may include family members, outpatient providers, and caretakers; transient factors, such as whether the hospital has a psychiatrist on staff; and many others. All other factors being equal, however, if the supply of appropriate beds does not match the demand for them at this juncture, hospital admission likely will be delayed or denied altogether.
Psychiatric Inpatient Beds
When state hospitals functioned as virtually the entire mental health system, they were the main disposition point for patients transferred from community hospital EDs, whether voluntarily or involuntarily. It is largely a result of this model that state hospitals continue to be viewed as synonymous with psychiatric hospitalization. Inpatient treatment remains a vital component of the continuum of care (
23–
26). At a minimum, emergency hospitalization allows time for stabilization of acute psychiatric symptoms, much as intensive care in a cardiac bed promotes stabilization of acute cardiac symptoms. Furthermore, inpatient psychiatric hospitalization offers an appropriate place and time for further evaluation, diagnostic study, respite, and initiation of complex treatment, just as inpatient care does for the delivery of other medical treatment.
As noted in the above examination of terminology, however, inpatient care extends far beyond state hospitals—and far beyond hospitalization in other settings as well. Psychiatric hospitalization itself has been transformed. In 2014, approximately 75% of residential psychiatric beds were located outside state and county hospitals (
23), and fewer than 2% of all public mental health care clients were treated in state hospitals (
27). Individuals 65 years or older, who made up 29% of the state and county hospital population in 1970, were being cared for largely in the community (
23).
Issues related to voluntary and involuntary civil and forensic hospitalization also have an impact on the beds landscape, including typical inpatient length of stay. Although some state hospitals continue to accept voluntary patients, most state and county beds today are reserved for civil patients deemed by a court to meet state criteria for involuntary civil commitment or, increasingly, for forensic patients committed through the criminal justice system (
10). Especially in forensic cases, involuntary hospitalization may have less to do with symptoms and clinical considerations than with public policies designed to address public safety, homelessness, or any number of other social concerns.
One study, for example, reported that patients who were found incompetent to stand trial and not restorable had a longer duration of commitment and received more involuntary medications, compared with a nonforensic patient sample, despite clinical data showing that they met fewer admission criteria and appeared less dangerous to themselves or others (
28). Patterns such as this also confound and complicate the issue of psychiatric beds.
Transitional and Community Beds
Residential treatment beds are the fastest-growing category of capacity in the United States; since 1970, the number of such beds has doubled, from 6.8 beds per 100,000 people to 13.5 per 100,000 in 2014 (
23). Terminology differs by locale. These beds may be described as “respite,” “transition,” or “step-down” services or by another name. Regardless of nomenclature, their essential characteristic is providing a place to stay that is monitored by nonmedical staff who are trained in medication administration and who provide transportation and other support and structure. They generally do not have a psychiatrist or a nurse on site but may have medical personnel on call in the case of an emergency. Residential stays are short term, such as 4 weeks or less.
Functionally, transitional beds may operate either as a hospital diversion or a hospital step-down strategy. Residents typically are referred by the public mental health system, hospitals, or another public agency; individuals and private providers usually cannot access transitional beds. Few studies have assessed the direct impact of transitional residential programs in producing measurably improved outcomes, but their role in linking people with mental illness to evidence-based programs and other supports strongly suggests they have an indirect association with improvement.
Recommendations
It should go without saying that the bed in one’s own home is the ultimate bed for any person with mental illness, as for any other medical patient. Only with a more complete continuum of psychiatric care will more individuals be able to live life to its fullest while accessing any needed supports in their own homes. To this end, the following recommendations issued by NASMHPD remain compelling and vital for improved mental health outcomes. Some of these recommendations are related to policies and practices regarding psychiatric beds, others move beyond beds themselves to contextual and background factors (
Box 1).
Recommendation 1. Establish a Vital Continuum
Prioritize and fund the development of a comprehensive continuum of mental health care that incorporates a full spectrum of integrated, complementary services known to improve outcomes for individuals of all ages with serious mental illness.
Timely and appropriate supports are the first line of mental health care. When fully realized, they reduce the demand for inpatient beds, which in turn provide essential backup when psychiatric needs cannot be met in the community.
Recommendation 2. Standardize Terminology
Direct relevant agencies to conduct a national initiative to standardize terminology for all levels of clinical care for mental illness, including inpatient and outpatient treatment in acute, transitional, rehabilitative, and long-term settings operated by both the public and the private sectors.
Shared terminology for core components of mental health care is essential to discussing, defining, and establishing an evidence-based continuum. Standardized definitions in the level-of-care guidelines for substance use disorders of the American Society of Addiction Medicine (
29) and the Level of Care Utilization System (
30) for psychiatric and addiction services are examples that model the benefits to clinicians, patients, and research from use of a common language.
Recommendation 3. Pursue Criminal and Juvenile Justice Diversion
Fund and foster evidence-based programs to divert adults with serious mental illness and youths with serious mental illness or emotional disorders from justice settings to the treatment system. These programs should operate at all intercept points across the sequential intercept framework and be required to function in collaboration with correctional and other systems.
Although individuals with serious mental illness make up an estimated 4% of the population, “severe psychological distress” is reported to affect 26% of jail inmates and 14% of prison inmates overall and 20%−33% of women inmates (
31). Similar overrepresentation is seen in the juvenile justice system. Evidence-based practices have been developed to prevent or diminish the prevalence of serious mental illness in the criminal and juvenile justice systems, but they are not universally available and remain underused.
Recommendation 4. Enforce the Emergency Medical Treatment and Labor Act (EMTALA)
Monitor hospitals for their adherence to EMTALA and levy sanctions for its violation, including withholding of public funding. Hospitals with licensed psychiatric beds that refuse referred patients should similarly be sanctioned if monitoring shows that they have a record of refusing referred patients without legitimate cause.
EMTALA is a federal law that requires stabilization and treatment of all persons coming to an ED prior to transfer, regardless of their insurance status or ability to pay. Nonetheless, compared with other medical patients, psychiatric patients wait longer in EDs for admission and experience other disparities, including discharge without treatment or even arrest. Potential receiving hospitals are not obligated to accept patients from EDs.
Recommendation 5. Improve Supply of Psychiatric Beds
Identify policies and practices that operate as disincentives to providing acute inpatient and other beds or that act as obstacles to psychiatric patients’ accessing existing beds (e.g., Medicaid’s IMD exclusion). Hospitals benefiting from taxpayer dollar investments should be required to directly provide or ensure timely access to inpatient psychiatric beds as a condition of their continued public funding.
A full continuum of care includes a sufficient number of beds to meet the acute, intermediate, and long-term needs of individuals with mental illness who require more intense or specialized services than are available in the community. Currently, statutory, licensing, funding, and other policies are combining to limit bed supplies and access in most states. Hospitals receiving public funding are not required to have psychiatric beds to serve their communities, and patients are often then hospitalized at sites far away from home.
Recommendation 6. Adopt Data-Driven Solutions
Prioritize and fully fund the collection and timely publication of all relevant data on the role and intersystem impacts of severe mental illness and best practices.
Evidence-based public policy and practice require reliable, comparable, and scalable data from which to identify, quantify, and analyze individual and community outcomes and thus implement best practices. Under new federal direction, more such data are becoming available, but the value of such data to policy makers and the public continues to be limited by the lack of common definitions and methodologies, delays in publication, and barriers to public access.
Recommendation 7. Strengthen Linkages
Recognize that the mental health, community, justice, and public service systems are interconnected and adopt and refine policies to identify and close gaps between them. This should include providing “warm hand-offs” and other necessary supports to help individuals navigate between the systems in which they are engaged.
Outpatient supports could effectively increase bed capacity by reducing the number of patients in need of inpatient care. However, because such supports often are unevenly distributed and operate in silos rather than in collaboration, system inefficiencies occur that create barriers to recovery as individuals are left to themselves to navigate a complex array of interventions despite their significant mental health and other challenges.
Recommendation 8. Incentivize Use of Technology
Create and expand programs that incentivize and reward the use of technology to advance care delivery, promote appropriate information sharing, and maximize continuity of care. Policy makers should require as a condition of such incentives that outcome data be utilized to help identify the most effective technologies and actively incorporate proven technologies and computer modeling in public policy and practice.
Mental health applications for computer and other technologies are proliferating and hold promise for promoting more precise, timely, and effective treatment for individuals with serious mental illness. At the same time, computer models are emerging that equip decision makers to analyze large data sets and project the impact of small changes to systems of care to better tailor interventions toward positive outcomes. Technology-assisted medical record keeping has increasingly been constructed to preserve and make available clinical information while maximizing allowable sharing of clinical information between clinicians through health information exchanges.
Recommendation 9. Develop the Workforce
Initiate assessments to identify, establish, and implement public policies and public-private partnerships that will reduce structural obstacles to entering or remaining in the mental health workforce. This workforce includes peer support for adults and parent partners for youths and their families. These assessments should include but not be limited to educational and training opportunities, pay disparities, and workplace safety issues, and the assessments should be conducted across all positions in the workforce.
The capacity of any system to deliver services effectively and efficiently is impaired by workforce shortages. Both outpatient and inpatient mental health services and supports are being limited in many locations because there are not sufficient numbers of trained workers and certified peers to provide them. These services include psychiatric beds that cannot be used because they are unstaffed. Limiting services in turn limits opportunities for recovery and the benefits of recovery to individuals and their communities
Recommendation 10. Expand Partnerships
Recognize the vital role that families and nontraditional partners outside the mental health system can play in improving mental health outcomes and encourage and support the inclusion of a broader range of invited stakeholders in improving mental illness policy and practice.
A growing number of advocacy organizations, faith-based communities, and others outside the mental health field are emerging as able and willing to support and supplement public resources. In some venues, such as those serving children, families are being included in treatment and policy development in new and more vigorous ways.
Conclusions
At every juncture, the rush to provide more beds needs to be moderated with illumination and clarity about patient needs, the kinds of beds best suited to meet those needs, and the recognition that bed capacity today is a function of far more than sheets on a mattress. The desire to add beds and bed-per-population goals as a one-dimensional solution needs to be tempered with the development of a continuum of care that includes comprehensive and high-quality treatment and services before, during, and after acute illness episodes. With the commitment of federal, state, and local policy makers and stakeholders to system improvement and consideration of the above recommendations, a robust, interconnected, and evidence-based system of care—and one that goes beyond inpatient beds—can be built to improve the lives of individuals with serious mental illness, their families, and their communities.