Mental Health Staffing at HRSA-Funded Health Centers May Improve Access to Care
Abstract
Abstract
Objective:
Methods:
Results:
Conclusions:
Highlights
Methods
Data and Sample
Independent Variables
Dependent Variables
Statistical Analysis
Results
| Licensed mental health FTE | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| per 2,000 patientsb | |||||||||||||
| Total | No mental health FTE | Fewer than one | At least one | ||||||||||
| (N=4,575) | (N=547, 19%) | (N=3,543, 71%) | (N=485, 10%) | ||||||||||
| Characteristic | N | % | SE | N | % | SE | N | % | SE | N | % | SE | pc |
| Patient mental health utilization (in past 12 months) | <.01 | ||||||||||||
| No mental health visits | 3,419 | 73 | 2 | 459 | 81 | 3 | 2,695 | 74 | 2 | 291 | 50 | 11 | |
| All mental health visits off site | 506 | 11 | 1 | 66 | 13 | 2 | 395 | 11 | 1 | 45 | 12 | 4 | |
| At least some mental health visits on site | 650 | 16 | 2 | 22 | 6 | 2 | 453 | 15 | 2 | 149 | 37 | 8 | |
| Health center | |||||||||||||
| Organizational capacity | |||||||||||||
| PCP panel sized | .94 | ||||||||||||
| <1,200 patients (reference) | 866 | 17 | 4 | 144 | 21 | 11 | 602 | 15 | 5 | 120 | 23 | 12 | |
| 1,200–1,999 patients | 2,565 | 58 | 6 | 221 | 60 | 15 | 1,990 | 58 | 7 | 354 | 50 | 19 | |
| ≥2,000 patients | 1,144 | 25 | 5 | 182 | 19 | 11 | 951 | 27 | 6 | 11 | 27 | 21 | |
| Ratio of clinic support staff to PCP FTE | .67 | ||||||||||||
| ≤2 (reference) | 1,306 | 34 | 6 | 170 | 43 | 15 | 971 | 33 | 7 | 165 | 26 | 13 | |
| >2–≤4 | 2,710 | 54 | 6 | 262 | 47 | 16 | 2,128 | 53 | 7 | 320 | 74 | 13 | |
| >4 | 559 | 12 | 4 | 115 | 10 | 8 | 444 | 14 | 5 | 0 | — | — | |
| Rural location | 1,506 | 47 | 6 | 304 | 72 | 16 | 1,001 | 43 | 7 | 201 | 28 | 14 | .13 |
| N of center’s clinic sites | .15 | ||||||||||||
| ≤10 (reference) | 2,298 | 60 | 6 | 407 | 80 | 12 | 1,756 | 57 | 7 | 135 | 49 | 19 | |
| 11–19 | 1,173 | 23 | 5 | 140 | 20 | 12 | 975 | 25 | 6 | 58 | 10 | 8 | |
| ≥20 | 1,104 | 17 | 4 | 0 | — | — | 812 | 18 | 5 | 292 | 41 | 18 | |
| Demand for mental health services: % of patients at center with a diagnosis of depression | .05 | ||||||||||||
| ≤5% (reference) | 1,244 | 30 | 5 | 304 | 52 | 15 | 930 | 28 | 6 | 10 | 1 | 1 | |
| >5%–<15% | 2,915 | 59 | 6 | 226 | 34 | 14 | 2,362 | 64 | 6 | 327 | 70 | 15 | |
| ≥15% | 416 | 11 | 4 | 17 | 14 | 13 | 251 | 8 | 3 | 148 | 30 | 15 | |
| Funding incentives for integrated care: % of total revenue from Medicaid managed care | .58 | ||||||||||||
| None (reference) | 2,259 | 56 | 6 | 293 | 48 | 16 | 1,751 | 58 | 7 | 215 | 55 | 18 | |
| <25% | 1,974 | 38 | 6 | 234 | 51 | 16 | 1,470 | 34 | 6 | 270 | 45 | 18 | |
| ≥25% | 342 | 6 | 2 | 20 | 2 | 2 | 322 | 8 | 3 | 0 | — | — | |
| Patients | |||||||||||||
| Predisposing factor | |||||||||||||
| Female | 2,946 | 66 | 2 | 369 | 74 | 4 | 2,311 | 66 | 3 | 266 | 48 | 10 | .04 |
| Age | .06 | ||||||||||||
| 18–25 | 427 | 16 | 2 | 265 | 62 | 4 | 1,691 | 50 | 2 | 247 | 51 | 4 | |
| 26–49 (reference) | 2,203 | 52 | 2 | 47 | 9 | 2 | 350 | 18 | 2 | 30 | 17 | 4 | |
| 50–64 | 1,945 | 31 | 2 | 235 | 29 | 4 | 1,502 | 32 | 3 | 208 | 32 | 5 | |
| Race-ethnicity | .24 | ||||||||||||
| Non-Hispanic White (reference) | 1,081 | 48 | 4 | 144 | 60 | 5 | 770 | 44 | 5 | 167 | 53 | 15 | |
| Hispanic, Latino | 1,616 | 25 | 3 | 183 | 19 | 6 | 1,313 | 28 | 4 | 120 | 15 | 3 | |
| Non-Hispanic Black | 1,074 | 20 | 2 | 159 | 18 | 6 | 813 | 21 | 3 | 102 | 18 | 9 | |
| Other | 804 | 6 | 1 | 61 | 3 | 2 | 647 | 6 | 1 | 96 | 14 | 6 | |
| Not married, no domestic partner (reference: married or has domestic partner) | 2,717 | 59 | 2 | 308 | 49 | 5 | 2,075 | 61 | 2 | 334 | 61 | 3 | .06 |
| Education | .28 | ||||||||||||
| Less than high school (reference) | 1,980 | 34 | 2 | 270 | 39 | 4 | 1,533 | 33 | 3 | 177 | 35 | 7 | |
| High school graduate | 1,268 | 29 | 2 | 125 | 24 | 2 | 1,001 | 32 | 2 | 142 | 21 | 7 | |
| More than high school | 1,327 | 37 | 2 | 152 | 37 | 4 | 1,009 | 35 | 2 | 166 | 44 | 6 | |
| Limited English proficiency | 1,418 | 17 | 2 | 138 | 11 | 4 | 1,203 | 19 | 3 | 77 | 13 | 3 | .13 |
| Would not or would only somewhat recommend health center to family or friends (reference: would definitely recommend) | 840 | 14 | 1 | 102 | 9 | 2 | 649 | 16 | 2 | 89 | 14 | 5 | .19 |
| Enabling factor | |||||||||||||
| Income ≤100% of the federal poverty level (reference: >100%) | 3,004 | 57 | 3 | 340 | 49 | 6 | 2,341 | 60 | 3 | 323 | 51 | 7 | .13 |
| Insurance coverage | .43 | ||||||||||||
| Uninsured (reference) | 1,241 | 30 | 3 | 197 | 25 | 5 | 942 | 31 | 4 | 102 | 27 | 7 | |
| Medicaid | 2,531 | 54 | 4 | 227 | 51 | 5 | 2,002 | 54 | 5 | 302 | 56 | 7 | |
| Other or missing response | 803 | 16 | 2 | 123 | 24 | 6 | 599 | 15 | 2 | 81 | 17 | 4 | |
| Need factor | |||||||||||||
| Level of psychological distress as measured by K6e | .08 | ||||||||||||
| Mild or none (reference) | 2,029 | 45 | 3 | 270 | 55 | 7 | 1,585 | 44 | 3 | 174 | 32 | 7 | |
| Moderate | 1,797 | 40 | 3 | 202 | 33 | 6 | 1,377 | 40 | 2 | 218 | 57 | 8 | |
| Severe | 749 | 15 | 1 | 75 | 13 | 3 | 581 | 16 | 2 | 93 | 11 | 5 | |
| Reported past-year want of or need for counseling or treatment for substance use | 356 | 5 | 1 | 40 | 4 | 2 | 263 | 6 | 1 | 53 | 5 | 3 | .89 |
| Excellent or very good self-reported health (reference: good, fair, or poor health) | 775 | 20 | 2 | 107 | 16 | 3 | 580 | 19 | 2 | 88 | 28 | 4 | .12 |
| Marginal | p>|z| for | |||
|---|---|---|---|---|
| Model and variableb | % | SEc | differenced | difference |
| Model 1: any licensed mental health staff (primary predictor) | ||||
| No mental health staff (reference) | 22 | 2 | ||
| Fewer than one mental health FTE per 2,000 patients | 24 | 1 | 2 | .370 |
| At least one mental health FTE per 2,000 patients | 32 | 4 | 10 | .049 |
| Model 2: type of mental health staff (primary predictor) | ||||
| No psychiatrist FTE on staff (reference) | 24 | 2 | ||
| Any psychiatrist FTE on staff | 26 | 2 | 2 | .507 |
| No clinical psychologist FTE on staff (reference) | 25 | 1 | ||
| Any clinical psychologist FTE on staff | 25 | 2 | 0 | .881 |
| No other licensed mental health provider FTE on staff (reference) | 25 | 3 | ||
| Any other licensed mental health provider FTE on staff | 25 | 1 | 0 | .909 |
| Difference | ||||
|---|---|---|---|---|
| from | p>|z| for | |||
| Model and variableb | % | SEc | base leveld | difference |
| Model 1: any licensed mental health staff (primary predictor) | ||||
| No mental health staff (reference) | 28 | 6 | ||
| Fewer than one mental health FTE per 2,000 patients | 49 | 3 | 22 | .001 |
| At least one mental health FTE per 2,000 patients | 65 | 7 | 38 | <.001 |
| Model 2: type of mental health staff (primary predictor) | ||||
| No psychiatrist FTE on staff (reference) | 40 | 4 | ||
| Any psychiatrist FTE on staff | 58 | 4 | 17 | .002 |
| No clinical psychologist FTE on staff (reference) | 50 | 3 | ||
| Any clinical psychologist FTE on staff | 50 | 3 | 0 | .935 |
| No other licensed mental health provider FTE on staff (reference) | 42 | 5 | ||
| Any other licensed mental health provider FTE on staff | 51 | 3 | 9 | .133 |
Discussion
Conclusions
Supplementary Material
- View/Download
- 416.16 KB
References
Information & Authors
Information
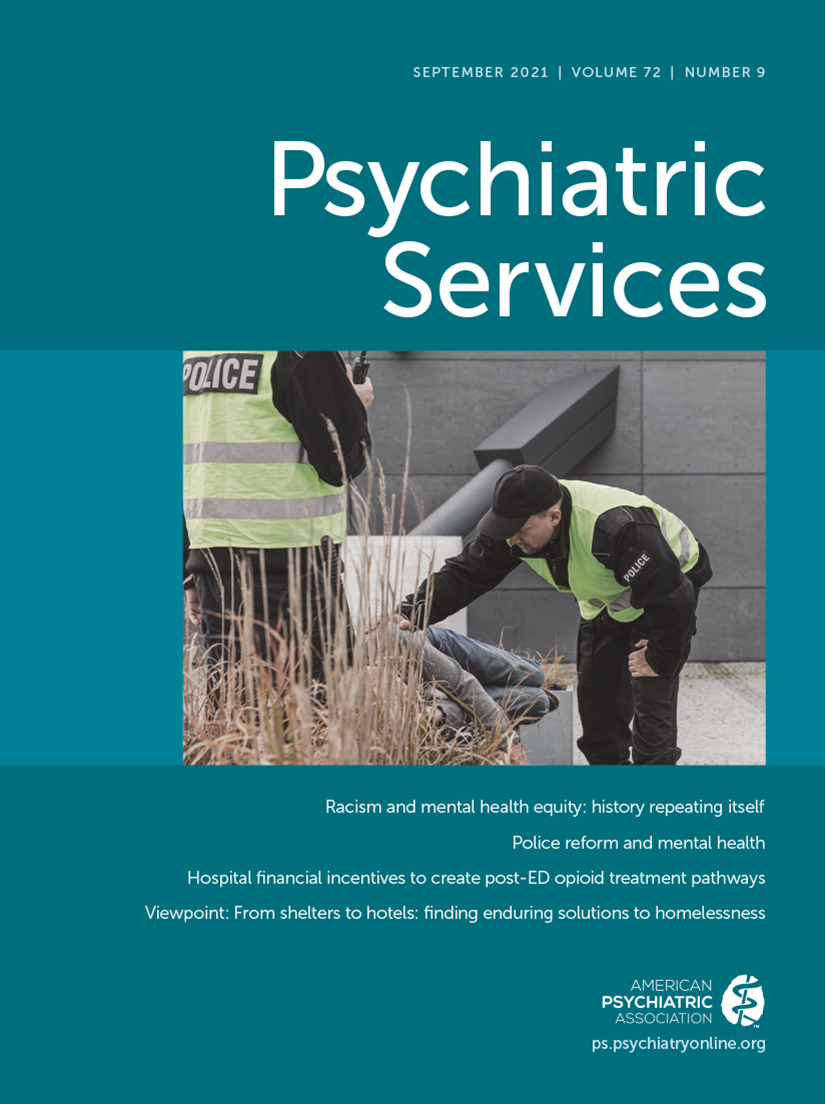
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing PsychiatryOnline@psych.org or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).