Established under Section 2703 of the Affordable Care Act, the Medicaid health home program represents a significant innovation in service delivery for Medicaid enrollees with behavioral health conditions, including addiction disorders. The program enables states to contract with designated health care providers to provide comprehensive health care with the goal of improving the cost-effectiveness and quality of care for enrollees with chronic health conditions. Although states have great flexibility in the design of their health home programs, all are required to target their services to enrollees with chronic health conditions and to provide five core services: care management, service coordination, transitional care, individual and family support, and referral to community services. Currently, there are 37 active health home plans in 21 states, with a total enrollment of more than half a million enrollees (
1).
Medicaid health homes are well positioned to identify and address addiction among some of the nation’s most vulnerable low-income residents. The prevalence of addiction is 50% higher among Medicaid enrollees than among the general population, and nearly 40% of all individuals with an addiction are covered by Medicaid (
2,
3). Moreover, many Medicaid health homes explicitly target enrollees with an addiction. Of the 37 Medicaid health home plans in operation, 15 specify addiction as a qualifying chronic condition for health home entry. Three of these plans, operating in Maine, Rhode Island, and Vermont, serve enrollees with an addiction exclusively, and the health home plan in Maryland serves enrollees with addiction or psychiatric disorders. An additional 14 state plans have established health homes specifically focused on enrollees with psychiatric disorders, and several primary care–based health home plans include psychiatric disorders as qualifying conditions for health home participation.
Health homes have the potential to play a critical role in addressing the complex needs of individuals with an addiction by resolving comorbid health conditions and reducing barriers to recovery. Chronic health conditions have a high rate of co-occurrence among individuals with an addiction, and the prevalence of addiction increases with an individual’s number of chronic conditions (
4).
Research has demonstrated the importance of health care delivery models that coordinate care for treating addiction. Care coordination models have proven effective in management of other chronic health conditions, such as diabetes and depression, and have shown promising results in the management of alcohol and other substance use disorders (
5,
6). For example, Morgenstern and colleagues (
6) found that coordinated care management increased substance abstinence and service utilization by individuals with an addiction compared with those who received usual care. Studies (
7) have also shown that care coordination models improve rates of addiction treatment initiation and treatment engagement after diagnosis and reduce addiction-related readmissions to acute care.
Despite the promise of Medicaid health homes to serve low-income individuals who have addictions, little is known about the strategies Medicaid health home plans use to identify and treat such individuals. To address this gap in the literature, we conducted a content analysis of all 35 Medicaid health home plans active in the United States in 2019 to identify which plans require health home providers to routinely screen, treat, prevent, and monitor addiction among their patients. Specifically, we report on differences in state requirements across health homes based on their focus on either primary care, psychiatric care, or addiction services.
Methods
Data on state health home plans were collected from the Medicaid State Plan Amendments (SPAs) publicly available on the Medicaid.gov website. We studied all amendments approved by the Centers for Medicare and Medicaid Services (CMS) to establish health homes since the option went into effect in 2010. An initial master list of all approved health home amendments as of November 2019 was taken from the CMS website. In states where multiple revisions had been made to a single plan, we created an indicator for the most up-to-date version of the SPA to ensure plans were not double-counted in our analyses. All states were required to provide the following information within their amendment applications: geographic limitations, population criteria, provider infrastructure, service definitions, and goal- and service-based quality measures.
Variables for coding were selected with the intent of encompassing the full range of organizational and service delivery characteristics represented in the list of approved health home amendments. We used the draft Health Home SPA template provided by CMS as a framework to guide our creation of an initial set of study variables. Next, we conducted a pilot assessment of eight SPAs and developed measures where appropriate to create a final data collection instrument and codebook. The final variable list included measures of the following characteristics of SPAs: primary focus of the health home service provision (primary, psychiatric, or addiction care), qualifying conditions for eligibility (with a specific indicator for the inclusion of substance use disorder as a qualifying condition for enrollment in a health home), authorized provider types and any certification or licensure requirements (with a specific indicator for the inclusion of a behavioral health, addiction, and/or peer support specialist in the health home), inclusion of addiction prevention services, and inclusion of addiction-related service delivery and outcome reporting measures.
Two coders were trained to review and code amendments. Issues were addressed twice per month during team phone calls, and any modifications to the coding scheme, measures, or other protocols were amended in the codebook. Discrepancies in results between the two coders were highlighted after each of the two coding sessions and were sent to a supervising team member (M.A.W.) for resolution. After reviewing the discrepancies and relevant amendment materials, the research team leader (C.M.A.), who developed the measures and coding scheme, issued final decisions on all remaining codes.
We identified 35 active Medicaid health home plans among 24 unique states. The average number of plans per state was 1.7, with one active plan in 15 states, two active plans in seven states, and three active plans in two states. By census region, the greatest percentage of plans were in the Northeast (N=13, 37%), followed by the Midwest (N=10, 29%), the South (N=8, 23%), and the West (N=4, 11%).
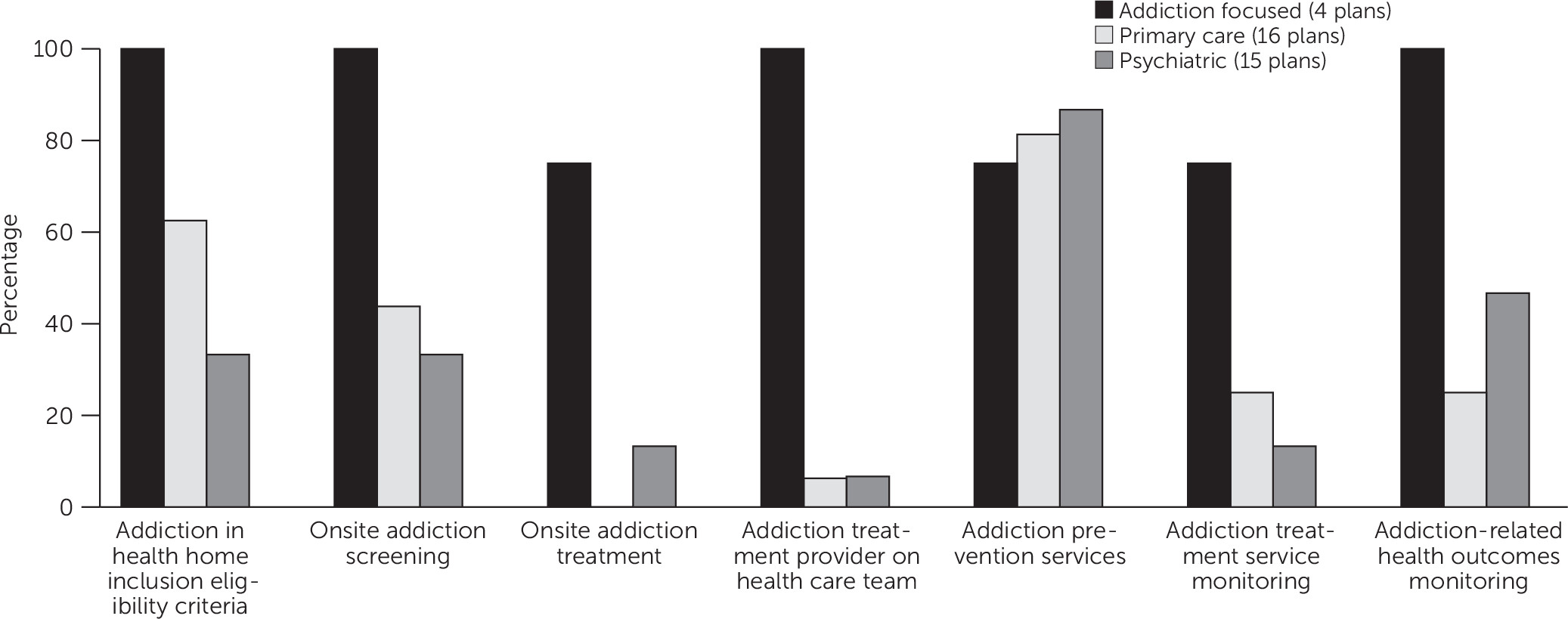
We calculated descriptive statistics for each SPA requirement (addiction as a qualifying condition in health home eligibility criteria, onsite addiction screening, onsite addiction treatment, addiction provider required on health home care team, addiction prevention services, addiction service monitoring, and addiction-related health outcomes monitoring). Descriptive statistics were stratified by programmatic focus: addiction (N=4), primary care (N=16), and psychiatric care (N=15). These programmatic foci were determined from the health homes population criteria and enrollment section of the SPAs. The final study data included all active health home SPAs, which obviated the need for inferential tests. This study was deemed exempt from institutional review board approval because no human subjects data were used.
Results
We found that all of the health homes that focused on addiction specifically included addiction in health home eligibility criteria, whereas only 63% (N=10) of health homes focused on primary care and 33% (N=5) of those focused on psychiatric care included addiction as an eligibility requirement (
Figure 1). Additionally, all addiction-focused health homes specifically required onsite addiction screening (compared with 44% [N=7] of primary care and 33% [N=5] of psychiatric health homes), included an addiction treatment provider on the health care team (compared with 6% [N=1] and 7% [N=1], respectively), and included addiction-related health outcomes in their monitoring plans (compared with 25% [N=4] and 47% [N=7], respectively). Although not all addiction-focused health homes provided onsite addiction treatment or addiction treatment service monitoring (75% [N=3] for both categories), these services were performed at much higher rates at addiction-focused health homes than at primary care (0% [N=0] and 25% [N=4], respectively) and psychiatric health homes (13% [N=2] for both categories). Addiction-focused health homes were less likely to provide a service in only one required area, with 75% providing addiction prevention services, compared with 81% (N=13) of primary care and 87% (N=13) of psychiatric health homes.
Discussion and Conclusions
Among the most important findings from this study is that most health home plans do not require providers to routinely screen patients for addiction. Aside from the few health home plans specifically focused on addiction, fewer than half of health homes required screening for addiction. Given that fewer than 20% of people with an addiction ever receive treatment for their condition (
3), it is possible that many health homes have individuals with undiagnosed addiction who are not receiving addiction care. Such untreated addiction can complicate health care delivery and coordination (
8,
9), impede the effectiveness of health care for other conditions, and lead to a host of other health conditions, such as cancer, heart disease, cirrhosis, and infectious diseases (
9).
Our findings also revealed that few states required Medicaid health homes to establish strong programmatic infrastructure for treating addiction. Requirements to include an addiction treatment specialist on the care team were limited. Although it is possible that some addiction treatment services could be delivered by primary care or other behavioral health care providers, these services may not be as comprehensive and tailored as those delivered by an addiction specialist. Moreover, our findings indicate that most states did not require Medicaid health home plans to provide truly integrated care for addiction treatment. This situation is likely a consequence of well-documented structural and financial challenges faced by health care providers in incorporating behavioral health into primary care and vice versa (
10). However, because many states identify addiction as a qualifying condition but do not require onsite staff or provide the necessary infrastructure to treat addiction, it will be difficult for health homes to make substantial improvements in their population health outcomes without adequately treating addiction and tracking addiction treatment outcomes. This circumstance is particularly important in psychiatric health homes, because addiction is highly comorbid with depression, anxiety disorder, and a host of other mental health conditions (
11). Given the high rate of the co-occurrence of psychiatric disorders and addiction, it is important for states to ensure that health homes that focus on these areas provide addiction screening and treatment.
The study findings should be understood within the context of several limitations. First, SPAs provide information only about what each state plan requires health home providers to do. It is possible that some health home providers may not fully adhere to the requirements laid out in the SPA. Second, it is possible that some health homes offer services as part of routine care that are not required or reported by their state program. The combination of these factors could result in either an over- or underestimation of actual service availability in some health home programs.
Addiction care must be a central component of any effective system of care for patients with complex chronic conditions. Although Medicaid health homes have made great strides toward improving the coordination and comprehensiveness of health care for enrollees with complex chronic conditions, the findings of this study indicate that greater attention to these areas is needed. For example, many primary care–based health homes could be missing important opportunities to identify and address addiction, which could in turn limit their success in improving other health outcomes. States should consider reviewing current policies and incorporating new requirements to ensure that Medicaid health homes are adequately identifying and treating addiction. There is also a need for further research to understand the impact of diverse Medicaid health home design choices on patient treatment receipt and outcomes for addiction as well as for other chronic conditions targeted by state health home models.