According to a WHO definition, the social determinants of health are the conditions in which people “are born, grow, live, work, and age.” They include adverse early life experiences; discrimination in its varied forms; exposure to conflict, violence, and other politically motivated harm; criminal justice system involvement; low educational attainment, poor-quality education, and educational inequalities; unemployment, underemployment, and job insecurity; individual and area-level poverty; homelessness, housing instability, and poor-quality housing; food insecurity; poor access to transportation; poor access to health care; adverse features of the built environment and neighborhood disorder; and exposure to pollution and the impacts of climate change (
3).
These social determinants are among the reasons postulated to explain the disproportionately high prevalence of COVID-19 cases and deaths among racial-ethnic minority groups in the United States. Such populations are less likely to be insured and therefore less likely to have access to COVID-19 testing and treatment; more likely to live in housing that makes it difficult to practice social distancing or self-isolate; more likely to work in jobs that they cannot afford to miss, that are not amenable to teleworking, and that require them to use public transportation (placing them at additional risk for exposure); and more likely to have underlying health conditions that increase risk, morbidity, and mortality—conditions that are themselves driven by social inequities (
2,
3).
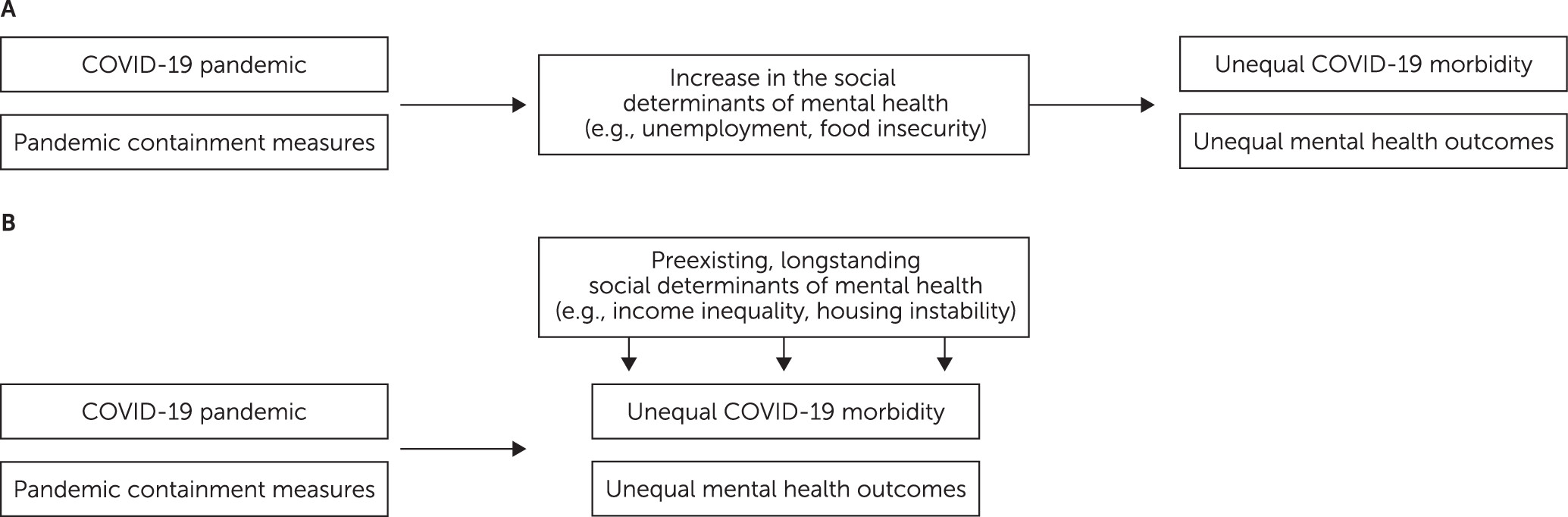
Mental health effects of the pandemic mediated by social determinants.
Mental health effects of the pandemic include serious and persistent stress, which may be associated with sleep disturbances; increased substance use; depressive symptoms, including suicidality; anxiety-related behaviors; and reductions in perceived health (
4). The pandemic’s effects on mental health are caused and compounded by the necessary containment measures, which include social and professional restrictions, physical distancing, and compulsory isolation at home. Both the pandemic and the measures for its containment increase the prevalence of certain social determinants. For example, many communities have observed increased prevalence of adverse childhood experiences, unemployment or underemployment, and food insecurity (caused by supply chain disruptions, business closures, empty store shelves, and inadequately stocked food pantries), to name just a few of the social and economic disruptions. Thus, aside from causing stress related to the virus itself, the pandemic will have substantial and long-lasting effects on mental health through pathways created by these social determinants. As such, the social determinants are mediators: the pandemic and its containment measures lead to these social conditions, which in turn lead to poor mental health and mental illness. A global economic slowdown has resulted from containment measures, accompanied by massive unemployment and fewer governmental resources to support public welfare systems. For each percentage point slowdown in the global economy, at least 14 million people are falling into poverty and food insecurity worldwide (
5,
6). The full effects of COVID-19 are yet to be seen, but given the current situation, the acute and long-term consequences on global mental health may be devastating.
Mental health effects of the pandemic moderated by social determinants.
Individuals experiencing the general medical and behavioral health inequities associated with the aforementioned social determinants have also carried a disproportionate burden of COVID-19 morbidity and mortality. Social determinants already existing in society because of longstanding injustices moderate the impact of the pandemic, and those with the greatest social challenges face the greatest impacts. Existing social and economic inequities drive the spread of infection and moderate the impact of containment measures, with foreseeable consequences on populations that are already disadvantaged. Poor populations, underdeveloped countries, conflict zones, prisons, and refugee camps appear to be more at risk to be hit the hardest (
5). Persons with serious mental illnesses may be particularly at risk because of their medical, social, psychological, and cognitive vulnerabilities (
7).
A damaging feedback loop has been created: each of the social determinants of health and mental health contribute to the disparate prevalence and severity of COVID-19 among marginalized and disenfranchised populations. In turn, the disparate prevalence of COVID-19 contributes to the worsening of the very social determinants that affect mental health. For example, housing instability makes sheltering in place more challenging and therefore increases the risk of contracting COVID-19. In turn, exposure to COVID-19 increases housing instability when at-risk individuals are excluded from housing, need to be isolated, and/or cannot pay rent because of COVID-19–related unemployment. Crowded housing and densely populated neighborhoods similarly set the stage for higher, and unequal, prevalence of infection, disease, and death.
Public policies and social norms.
Any consideration of the social determinants of health leads to the underlying public policies and social norms. The pandemic is underpinned by public policies and social norms that, by creating social injustices, ultimately increase risk for disease and behavioral disorders. Without direct policy and social action, these injustices will continue to affect the lives and health of those already suffering deprivation, discrimination, and inequality, even after the stressor has receded.
From a public policy perspective, the COVID-19 crisis has quickly disclosed the unpreparedness of public systems to face viral epidemics in even the historically richest European and North American countries, exposing widespread inadequacies, including shortages of personal protective equipment, testing reagents, ventilators, and other supplies. In some places, political debates have affected or trumped coordinated efforts to efficiently and effectively ramp up testing availability and contact tracing. Additionally, as noted above, policies that affect health care access in general directly affect vulnerability to, identification of, and treatment of the illness itself.
Social norms are the informal agreements that govern the behavior of members of a society. In contrast to official policies, laws, rules, and regulations, the social norms that underpin the social determinants of health are the conscious and unconscious biases and beliefs that maintain systemic inequality and inequity. For example, the overrepresentation of COVID-19 infection among some of the lowest-paid workers in the United States who, in the context of the pandemic, are now deemed “essential” reflects, in part, a longstanding underappreciation of their value, their socioeconomic challenges, and their health care needs. Disturbingly, the concentration of COVID-19 illness and impact on racial-ethnic minority groups, which have suffered centuries of discrimination and trauma, exposes the continuing challenges of racism, racial discrimination, race-based inequities, and structural violence.