Humpty Dumpty sat on a wall,
Humpty Dumpty had a great fall.
All the king's horses and all the king's men
Couldn't put Humpty together again.
The Humpty Dumpty nursery rhyme is relevant to the work that state policy makers will face while rebuilding public mental health systems after COVID-19. A pithy response to why Humpty could not be put back together is that “he wasn’t all he was cracked up to be.” This may be relevant to many pre–COVID-19 public mental health systems that were siloed and fragmented, but a more apt interpretation is that when something precious that is complex and fragile suffers a blow that threatens its very existence, do not waste time trying to put it back together as it was. Be creative and innovative to build something stronger and more resilient.
This column presents the perspective of leaders of the New York State (NYS) public mental health system while the COVID-19 pandemic unfolded and as we prepare for the future. During the pandemic, individuals with mental illness followed the same rules as everyone else, maintaining social distance and staying at home. Hospital psychiatric services dropped dramatically, in part because of lockdowns to prevent the spread of infection, but mainly because hospitals needed to use all available beds to treat COVID-19 patients. Community mental health providers ramped up telehealth services, but the pace and extent of change has been so dramatic that many provider agencies with already razor-thin financial margins became anxious about sustainability.
State policy makers reacted: regulations were relaxed, emergency orders were issued, and interim guidelines including expanded payment for telehealth enabled providers to continue treating patients. When the pandemic wanes, the crisis will evolve into an opportunity for redesigning public mental health systems. Large budget deficits due to the pandemic will create further impetus for system redesign.
Two of us (T.E.S., A.-M.T.S.) hold positions in the NYS Office of Mental Health and participated in efforts to sustain the public mental health system throughout 2020. NYS-operated psychiatric services include 2,300 civil beds, 2,200 forensic beds, and 20,000 ambulatory patients. Community-based services that are funded and regulated by NYS include 10,000 community inpatient beds, 650 ambulatory programs serving over 700,000 individuals each year, and >43,000 residential beds.
Despite the pandemic’s resurgence in fall 2020, we see some silver linings and lessons learned that can guide the hard work ahead. Below, we highlight key focus areas and guiding principles that policy makers may consider as they redesign their systems, organized into the following domains: emphasizing a population health approach, leveraging public-private provider relationships, broadening service delivery platforms, and redefining best practices. We emphasize the need for data-driven policy making in which new or revised regulations are routinely coupled with specific, measurable standards of care that enable tracking of both implementation outcomes and unintended consequences. We also recognize that some of these innovations are too new to evaluate or critically assess at this point.
Emphasize a Population Health Approach
Community mental health clinics across NYS rapidly redirected services to virtual platforms in March and April 2020 when COVID-19 cases first became widespread. Immediate concerns involved access to care for patients with high needs: Who is likely to decompensate because of lack of medications or other support? Who may be having thoughts of harming themselves or others? Who needs immediate outreach versus who has the supports and wherewithal to get through the lockdown on their own?
Population health approaches will be key to redesign efforts. Policy makers should ensure that providers and systems use algorithms that identify and help prioritize patients having high needs for interventions. Information should be available via health exchanges, qualified entities, or registries and should be shared across public health agencies, for example, to flag individuals with serious mental illness who are homeless or have criminal justice involvement. During the pandemic, the NYS mental health authority has made available to NYS providers an information system called PSYCKES (Psychiatric Services and Clinical Knowledge Enhancement System;
https://omh.ny.gov/omhweb/psyckes_medicaid/about) that is free of charge and uses Medicaid and other administrative data to display individual-level patterns of service use and flags for clinical high-need characteristics, including gaps in receiving services and repeated use of acute services. Although some services may have a data lag of 3–4 months, the online portal was invaluable in helping providers triage patients’ needs during the pandemic.
Large payer and provider networks have the resources to access technological supports such as PSYCKES or to implement their own algorithms to flag patients with high needs, maintain registries, and participate in information exchanges. Small- and medium-size community mental health providers do not have these capabilities, however, and need support from state oversight agencies. In 2018, NYS funded behavioral health care collaboratives that allow community mental health providers to create independent practice associations that share digital platforms and interface with larger health care systems to support performance and quality measurement.
Efforts to monitor and support patients with high needs represent critical tertiary preventive care. State policy leaders should also promote primary and secondary prevention strategies to address the mental health sequelae of the COVID-19 pandemic. Many people, especially hospital workers and those who lost a loved one to the pandemic, will experience anxiety, depression, posttraumatic stress disorder, or complex grief. NYS implemented an Emotional Support Helpline in March 2020 to provide free and confidential support to callers. The helpline was staffed by 400 licensed mental health professionals and senior psychology students who were supervised by volunteers. Over a 12-week period, from March to June 2020, the helpline handled nearly 18,000 calls from individuals seeking emotional support, with 10% of the calls coming from health care workers.
Leverage Public-Private Provider Partnerships
Flexible and appropriate use of inpatient psychiatric beds has become an urgent national issue (
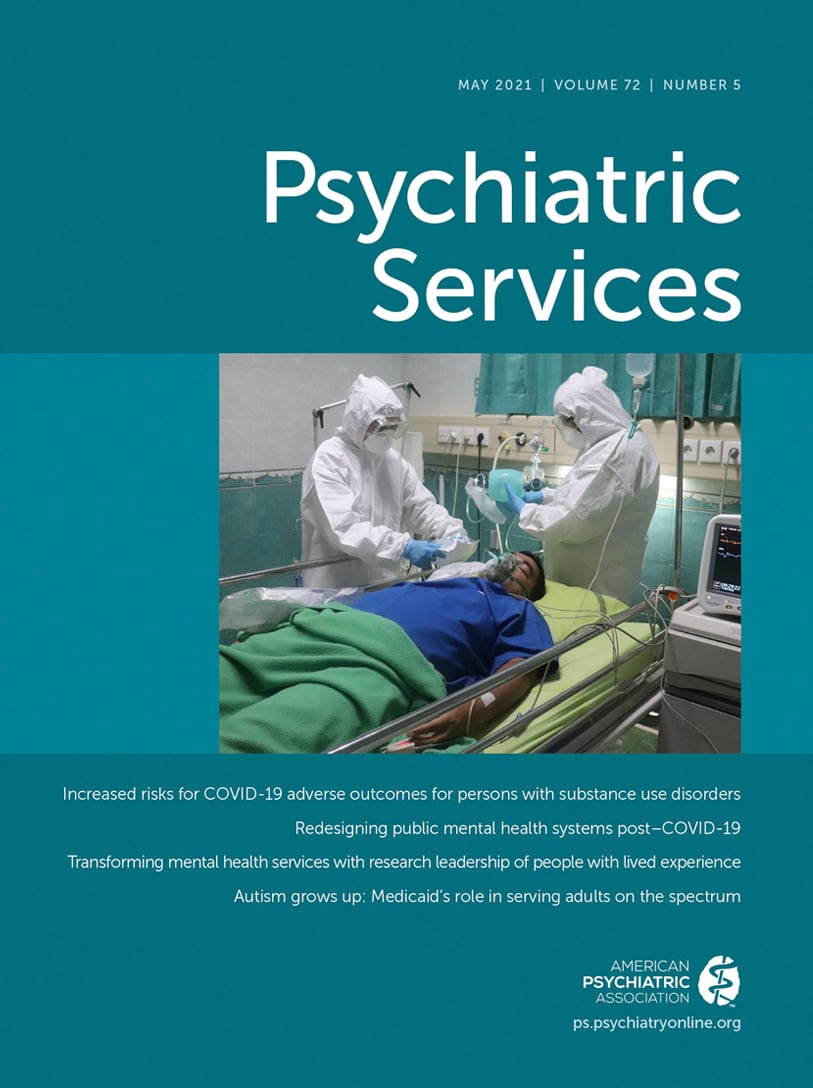
1). Hospital inpatient psychiatric care in New York City was rapidly and dramatically reorganized in the initial few weeks of the COVID-19 pandemic. When the NYS governor ordered hospitals to increase their bed capacity by 50% to manage the surge of COVID-19 cases, New York City’s public hospital system, which comprises about 40% of the city’s psychiatric bed capacity, converted approximately 30% of its adult beds, 40% of its child/adolescent beds, and 100% of its substance use detoxification beds to COVID-19–related services. The New York City community hospital system similarly converted 20% of its psychiatric beds to COVID-19–related services. Seven state-operated psychiatric hospitals assisted this rapid downsizing by accepting 165 patient transfers from community hospital psychiatric units. Additionally, a newly built, state-operated psychiatric inpatient building, which was due to open in May, was repurposed for COVID-19 patients and staffed by a large New York City hospital system.
To support this rapid collaboration of systems, NYS passed emergency regulations for public and commercial insurers, including easing regulations for admission, discharge, and transfer of patients and easing credentialing of out-of-state clinicians. New York City’s private, public, and state-operated psychiatry programs worked as a single system of care during the pandemic with daily communications and data sharing among hospitals to triage and move patients within the system in order to ensure availability of hospital beds for COVID-19 patients. Such cooperation, if continued, could ensure that more patients receive the appropriate level of intensive services when needed. Public policy leaders need to leverage such system-wide collaborative relationships to allow ongoing flexibility and responsiveness to system needs.
Broaden Service Delivery Platforms
Policy makers have been dipping their toes into the telehealth waters for several years, but the pandemic threw providers into the deep end of the pool. Widespread availability of telehealth services for individuals with behavioral health conditions is one of the silver linings arising from the COVID-19 pandemic. Within 4 weeks of the lockdown, NYS mental health clinics were providing 80%–90% of their services via online video telehealth or telephonic platforms. Anecdotal reports indicate that access to care improved and patient “no-shows” for telehealth appointments were markedly lower. Many patients prefer telehealth, noting that they do not have to spend time in waiting rooms, that their provider seems more attentive, and that the communication feels more personal. How will policy makers know which specific telehealth practices offer real advantages and should be continued beyond the pandemic? Providers have suggested billing for the time spent texting patients—if regulations are permanently relaxed, what would the potential “uberization” of mental health (
2) look like?
Policy makers should define measurable standards of care that will accompany new telehealth regulations and address anticipated obstacles such as availability and cost of equipment. Standards could encourage shared access to electronic mental health records, digital-based supervision of clinical staff, and measurement-based care. Telehealth could also support the care of patients with serious mental illness, including requirements such as providers committing to telehealth meetings with hospitalized patients before discharge when patients are referred for aftercare, or use of telehealth for emergency room consultations and evaluations. Linking new regulations with specific standards of care allows state policy makers to limit unintended consequences, maintain providers’ focus on quality of care, and adequately measure the impact of regulatory changes.
Community mental health agency directors are now facing the challenge of having to estimate future space needs and what proportion of services will continue to be provided virtually. The NYS Office of Mental Health has already received requests from licensed clinic providers to downsize clinic space by as much as 50% in anticipation of more services being offered by telehealth. How much downsizing should be allowed by oversight agencies? Approvals should include conditions that ensure that individuals with serious mental illness do not experience diminished access to care, such as requirements that clinics ensure onsite services for timely in-person evaluations of new referrals, provision of injections of long-acting antipsychotic medications, and core activities that meet standards for integrated care, including monitoring of vital signs, weight, and metabolic parameters.
Redefine Best Practices
State policy makers should look for opportunities to implement new standards for key best practices. For example, as telehealth became widespread, anecdotal reports underscored the importance of measurement-based care. Prescribers who previously were not interested in patient ratings of depression, anxiety, and other symptoms became much more willing to receive reports from therapists and care managers that included symptom ratings. Telehealth care for individuals with serious mental illness is greatly enhanced when treatment team members communicate and share information; revised regulations should encourage such communication.
State policy makers should develop clear standards related to care management for individuals with serious mental illness. When mental health providers identified patients with high needs during the NYS lockdown, the burden for outreach fell primarily on care managers, many of whom continued to work in high-risk settings such as community residences, adult homes, and nursing homes. Urgent guidance was needed for infection control. Reform initiatives over the past 10 years have identified care management as the backbone of integrated public health programs (
3), yet there is limited consensus on care manager qualifications, training and supervision, and standards of care.
Standards and best practices need to be developed for care management of individuals with serious mental illness. They need care management that is flexible, persistent, and provided by care managers who are experienced, skilled, and comfortable working with this population. Techniques such as motivational interviewing, deescalation, advocacy on behalf of patients, and mobilization of family and other key supports are critical. State policy regulations should establish such practices and techniques. NYS is developing specialized care management services in a program called Health Home Plus, which will serve the 25,000 individuals with highest needs living with serious mental illness across the state.
Another opportunity to reexamine practices involves assertive community treatment (ACT). When New York City hospital psychiatric programs rapidly discharged patients early in the pandemic, most community mental health clinics could not support care transitions because their staff were working from home. NYS policy makers responded by asking community-based mobile crisis and ACT teams to support posthospital care transitions. NYS and city oversight leaderships rapidly designed a hybrid model of ACT and brief critical time intervention. Standards were written that allowed ACT teams to admit patients directly from hospital psychiatric inpatient or emergency departments and provide time-limited (3 months) treatment as patients transitioned to community-based care. This promising model could help address the gap in critical engagement between inpatient and community care that contributes to adverse outcomes, including suicide, violence, and all-cause mortality.
Other examples likely exist of innovative providers who have modified practices to meet urgent needs during the COVID-19 pandemic. Virtual learning care collaboratives like Project ECHO (Extension for Community Healthcare Outcomes, [
4]) would be helpful in spreading these practices. State policy makers should think beyond immediate needs related to the pandemic and consider regulatory changes that address these long-standing gaps in access and standards of care.
Conclusions
Although NYS is a well-funded and experienced public mental health system, its leadership and staff still learned a great deal during the COVID-19 pandemic. Much more work remains to be done to stabilize and evolve public mental health systems nationally, and state public mental health policy makers understand perhaps more than anyone how to do more with less. Policy makers will need to rebuild public mental health systems while also dealing with marked reductions in funds for services due to the pandemic’s devastating impact on state’s economies. But such crises create real opportunities for change. To quote Victor Hugo, “The future has several names. For the weak, it is impossible; for the fainthearted, it is unknown; but for the valiant, it is ideal.” Now is the time for valiant public policy.