When the first case of COVID-19 was confirmed in New York City (NYC) on March 1, 2020, medical directors of not-for-profit behavioral health agencies across the city confronted the urgent need to protect people with serious mental illnesses (schizophrenia, bipolar disorder, and major depressive disorder) and people with intellectual/developmental disabilities. In particular, people in congregate residences and homeless shelters were at high risk because of crowded living conditions that could increase viral transmission (
1).
People with serious mental illnesses die on average 25 years earlier than the general population because of high rates of comorbid medical conditions, including obesity, type 2 diabetes, hypertension, and nicotine dependence, all of which have been associated with COVID-19 morbidity and mortality (
2,
3). People with intellectual/developmental disabilities likewise experience greater morbidity and earlier mortality (
4). The vulnerabilities of these populations are compounded by the physiological sequelae of psychological trauma and multiple social determinants of health, including poverty, inadequate housing, food insecurity, discrimination, and structural racism (
5,
6). Despite the high risks and health costs of this population, these individuals have poor access to care, a finding that has prompted efforts to integrate primary care and behavioral health services (
7).
In NYC, about 20,000 people with serious mental illnesses or intellectual/developmental disabilities live in congregate residences with shared living spaces and staff supervision. Another 60,000 people live in the city’s homeless shelters, in some cases with 100 people in one room. An outbreak in this population could have a severe impact on the ability of the hospital system to respond. To better understand mitigation needs, this investigation sought to characterize the incidence of presumed and confirmed COVID-19 illness, hospitalization, and death in congregate and noncongregate cohorts composed of more than 8,000 people served by a NYC not-for-profit behavioral health system.
Methods
We collected data on COVID-19 symptoms, testing, hospitalization, and mortality, prospectively and in real time, for the total population of individuals served by one citywide not-for-profit behavioral health agency. This sample included individuals living in 29 congregate settings (13 residences for people with serious mental illness, 12 residences for people with intellectual/developmental disabilities, three shelters for homeless people with mental illness, and one shelter for homeless veterans) and those served by 41 noncongregate programs (scattered-site housing and outpatient treatment programs), as well as the staff working with these populations.
Screening for COVID-19 symptoms was implemented across the agency during the first week of March 2020, with additional daily temperature screening implemented at residences for people with intellectual/developmental disabilities. From March 9, 2020, to May 3, 2020, staff were asked to use a template to report, within an hour of notification or discovery, data on “sick clients” or “sick staff.” The template asked for the sick person’s symptoms; date of symptom onset; results of COVID-19 testing, if done; nature of exposure, if known; and whether the sick person had any prolonged (>10 minutes), close (<6 feet) contact with other staff or clients in the 3 days before or after symptom onset. During the time of the study, COVID-19 testing was generally limited to hospital settings. Information on presumed or confirmed COVID-19 illness, hospitalization, and death was aggregated in a database.
Criteria for presumed COVID-19 illness included one or more of the following symptoms: fever, cough, shortness of breath, sore throat, nasal congestion, body aches, diarrhea, or loss of sense of taste or smell. Cough without other symptoms was included only if the cough was new or if there was a subjective change in the quality or frequency of the cough. Individuals with a negative COVID-19 test result within 7 days of symptom onset were not counted as having COVID-19 illness.
Individuals with presumed or confirmed COVID-19 illness were asked to isolate for at least 7 days and until afebrile for at least 72 hours without the use of antipyretics and with resolving symptoms. People with exposure to presumed or confirmed COVID-19 were asked to isolate for 14 days. Symptomatic individuals in residences were provided with single rooms for isolation; isolation facilities became available to shelter clients a few weeks into the crisis. Some individuals (e.g., people with behavioral disorganization, lack of insight, severe substance use disorders, or exposed persons in shelters) were unable to be isolated; in these instances, staff informed all others in the residences to keep 6 feet away from the sick person to the extent possible and sought to enforce masking for all persons in the residence. However, masks were not widely available during the first month of the pandemic. Available personal protective equipment was prioritized for residences for people with intellectual/developmental disabilities.
We collected data in Excel, which was used to calculate population incidence. Chi-square tests were performed with an online calculator (
www.socscistatistics.com) to determine whether risk factors, including program type, congregate housing, gender, race-ethnicity, age, or psychiatric diagnosis, were associated with COVID-19–related hospitalization and death. These data were collected in the course of the behavioral health agency’s effort to screen for, track, and mitigate the spread of COVID-19 illness among its clients and staff. Institutional review was not required.
Results
Data were collected for 8,256 clients, including 1,543 clients in congregate programs (587 living in 13 residences for those with mental illness, 98 living in 12 residences for those with intellectual/developmental disabilities, 858 living in four homeless shelters), and 6,713 clients in noncongregate programs (1,705 in scattered-site housing and 5,008 in outpatient programs). There was significant turnover among the shelter population, with 648 clients present at the beginning of data collection and an additional 210 clients admitted during the study. (Data collected for 1,086 staff are available in the online supplement, along with available data on the demographic, diagnostic, and health risk characteristics of the client and staff populations.) For the total client population for whom demographic data were available, 51% (N=3,271/6,375) identified as female, 57% (N=2,779/4,848) identified as Black, 57% (N=3,458/6,104) were age 45 or older, 75% (N=3,628/4,840) had a serious mental illness (39% [N=1,902/4,840] had a primary diagnosis of schizophrenia or schizoaffective disorder), 57% (N=1,063/1,878) were obese, 50% (N=886/1,757) were hypertensive, and 49% (N=1,028/2,089) were smokers.
A total of 218 (2.6%) clients developed COVID-19–like illness; 84 (39%) were able to obtain testing, and 77 (92%) tested positive. Daily incidence peaked around March 31, 2020 (see online supplement). Among clients with confirmed COVID-19 (positive test), 49 (64%) were hospitalized and 19 (25%) died. Among the 134 clients with presumed COVID-19 (symptoms but no test results), five (4%) were hospitalized, and three (2%) died. Among the 211 clients with presumed or confirmed COVID-19, the most prevalent reported symptoms were fever (N=94, 43%), cough (N=83, 38%), and shortness of breath (N=39, 18%).
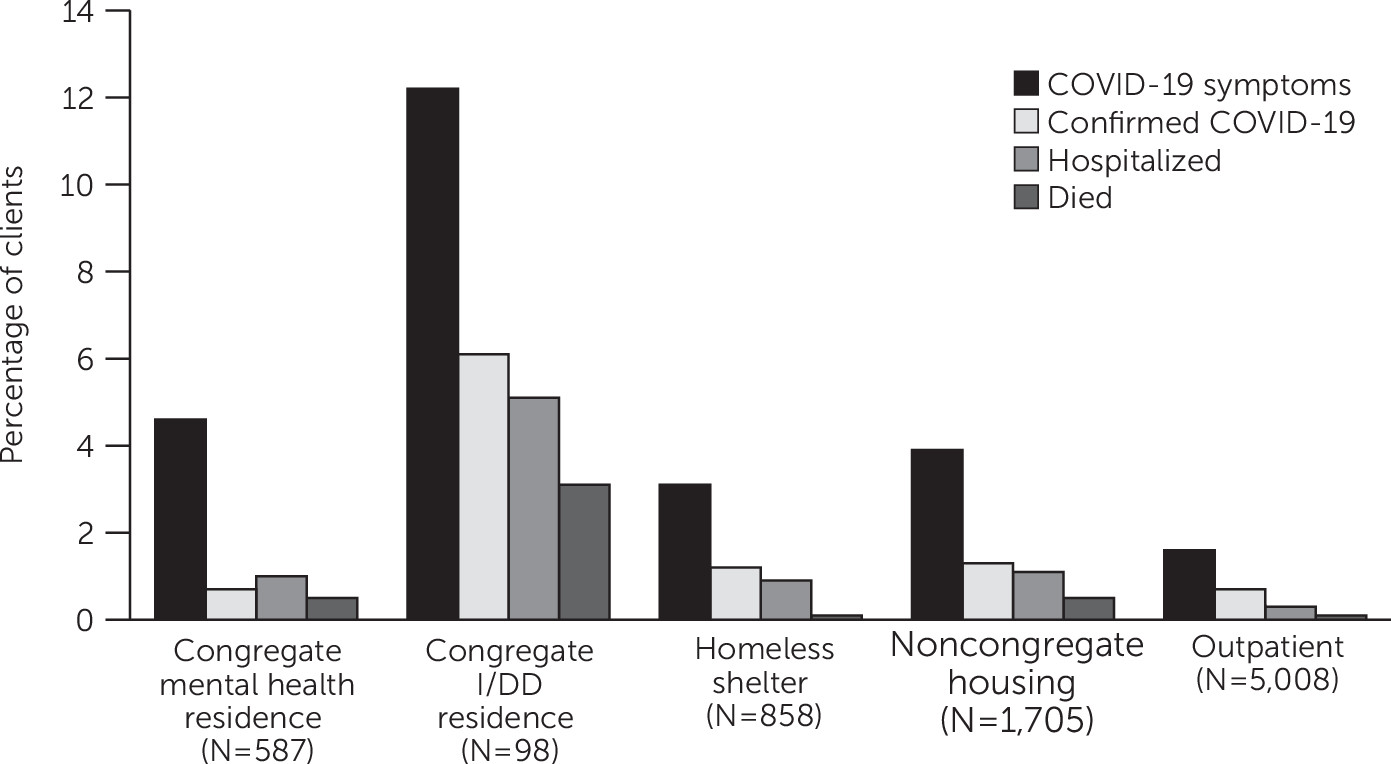
Presumed and confirmed COVID-19 illness, hospitalization, and death by program type are presented in
Figure 1. In congregate programs, 66 (4%) clients developed COVID-19–like illness (35% tested, 80% tested positive), 19 (29% of cases) clients were hospitalized, and seven (11% of cases) clients died. In noncongregate programs, 145 (2.2%) clients developed COVID-19–like illness (40% tested, 97% tested positive), 35 (24% of cases) clients were hospitalized, and 15 (10% of cases) clients died. The highest incidences of symptoms (N=12, 12% of cases), hospitalizations (N=5, 42% of cases), and deaths (N=3, 25% of cases) were found for clients in the congregate residences for individuals with intellectual/developmental disabilities.
Clients in congregate programs were more likely than those in noncongregate programs to develop COVID-19–like illness (χ2=22.6, df=1, N=8,256, p<0.01) and to be hospitalized but not to have died. (The results of chi-square tests for risk factors of COVID-19–related hospitalizations and deaths are presented in the online supplement.) People living in congregate residences for those with intellectual/developmental disabilities and people age 45 or older were significantly more likely to be hospitalized or to have died. Hospitalizations and deaths did not differ by race-ethnicity or gender. People with serious mental illnesses were not more likely to be hospitalized and were less likely to have died compared with people with other diagnoses.
Discussion
The disproportionate impact of the COVID-19 pandemic on individuals served by a behavioral health housing and treatment system is in keeping with recent reports (
8–
10) from shelters for people experiencing homelessness and from residences for people with intellectual/developmental disabilities, where crowding and high staff contact are of greatest concern. To our knowledge, this was the first cohort study that included primarily people with serious mental illness, who, regardless of incidence of infection, may have worse health outcomes (
11). In this study, the highest morbidity and mortality occurred among people with intellectual/developmental disabilities, drawing attention to the needs of this group.
A quarter of clients with confirmed COVID-19 died during this 2-month period, a case fatality rate exceeding that seen in a hospitalized population (
3). Along with the high rates of positive tests, resulting in part from the dearth of testing available, this finding exposes limitations in the health care system’s ability to respond to the needs of people with mental health issues and those experiencing homelessness. It is unclear what proportion of presumed COVID-19 cases were true cases, but the otherwise unexplained deaths in this group underline the importance of care, including isolation and monitoring, for people with COVID-19 symptoms who are unable to obtain testing.
Reliance on self-report data and the inability to confirm COVID-19 were limitations of this study. Underreporting was likely, and many asymptomatic individuals, representing an estimated 40% of COVID-19 cases, may have been missed (
12). Copies of test results were not available, because tests were generally done only in hospitals that were in crisis during this period, and the reliability of the tests performed is not known. Symptoms may have been more easily discovered among clients who had closer monitoring by staff, possibly inflating the difference between congregate and noncongregate settings. In turn, the shelter incidence rate was affected by the high client turnover rate and diversion to isolation beds, likely underestimating the risk in this population. By the time testing became more widely available, incidence of new cases was already low across the city (see the online supplement for results of shelter testing drives, where all tests were negative). Insufficient client-level demographic and cardiometabolic risk factor data were available to test for associations with COVID-19 illness, although analyses for hospitalizations and deaths for noncardiometabolic risk variables were done. Another limitation of this study was that comparisons were made between cohorts of people receiving behavioral health services but not with the general population.
The incidence curve of new (including presumed) cases across the agency roughly corresponded with the confirmed case curve (
13) for NYC, with incidence beginning to decline for the agency a week earlier than for the city at large (March 31 versus April 8). Although the earlier decline in incidence cannot be clearly attributed to the interventions put into place, early implementation of cleaning, screening, isolation protocols, contact tracing, and masking may have mitigated risk. Ultimately, increasing availability of affordable, supportive noncongregate housing will be needed to reduce risk in the long term, particularly for shelter residents.
The tendency of people with serious mental illnesses to self-isolate may be protective in the setting of a pandemic, as suggested by the lack of association of these diagnoses with COVID-19 morbidity and mortality in this study. For this population, home visits from behavioral health workers may paradoxically present a risk of viral transmission. Conversion to increased use of telehealth may reduce infection risk, but it is not yet clear how telehealth will affect psychiatric risk in this high-risk population. Anecdotally, however, the rapid advent of telehealth spurred by this pandemic has addressed a longstanding barrier to care in this population: people who have been unable to attend health care appointments because of negative symptoms, behavioral disorganization, or depression have been able to connect with psychiatric and medical providers by telephone. Facilitating access to care must, however, be balanced with the importance of helping people to engage with community life.
In behavioral health agencies, the responsibility for infection control may lie with psychiatrists, who are usually at the medical helm of these organizations. Access to virtual primary care consultation and to guidelines developed by major hospitals supported this agency’s ability to respond to the crisis. The pandemic only puts more focus on the need for integration of behavioral and general medical care across the system.
Conclusions
People with behavioral health disorders are highly vulnerable to the risk posed by the COVID-19 pandemic. Screening, personal protective equipment, and isolation capacity are needed to address the high risk of COVID-19 morbidity and mortality among this population, particularly in congregate housing, and for people with intellectual/developmental disabilities. Further research on risk and preventive factors is needed to mitigate future waves of the pandemic.