Syndemics, or synergistic epidemics, were first described in the literature in the early 1990s, specifically highlighting the convergence of substance use disorders, violence, and AIDS (
1). Syndemic theory helps to provide a framework for how diseases and social conditions form, interact, and cluster to produce worse outcomes for certain populations (
2,
3). The 2019 coronavirus disease (COVID-19) pandemic, racial injustice, and health inequities have recently been posited as a new syndemic, globally and particularly in the United States (
3,
4). Here, we consider the syndemic of COVID-19, mental health inequities, and structural racism.
Although COVID-19 has led to significant morbidity and mortality, it is particularly important to consider its impact on people with mental illnesses and substance use disorders (
5). COVID-19 has been associated with increased mental health problems, including depression, suicide, anxiety disorders, and substance use disorders (
6). Furthermore, because of a confluence of social determinants of mental health and structural vulnerabilities, people with serious mental illnesses and substance use disorders are at greater risk of contracting COVID-19 (
5). Additionally, other oppressed and marginalized communities, including Black, Latinx, and Indigenous people, have higher rates of infection, hospitalization, and mortality, compared with White people (
7).
Similarly, although it is well known that racial and ethnic inequities are pervasive in the behavioral health system, recent highly publicized killings of unarmed Black people (at a critical time when the United States was economically and socially slowed enough to take closer notice) have served to sharpen the focus on structural racism and social injustice as a driver of poor health and health inequities. Thus the deadly manifestations of structural racism in the context of COVID-19 have shone a light on inequities in mental and substance use disorders for oppressed and marginalized populations, revealing a second pandemic of social injustice in the United States (
8). Taken together, the concentration and interaction between racial injustice, COVID-19, and mental health inequities have led to devastating health consequences (
3,
4). The intersection of these three conditions, and the resulting syndemic, presents numerous policy challenges—and opportunities. Addressing these issues in a unified manner, using a syndemic theory approach, can lead to significant progress and effective solutions for otherwise intransigent problems in society.
To date, the federal response to the COVID-19 pandemic has not adopted a syndemic theory approach. Initial legislation provided emergency funding for federal agencies and expansion of telehealth services (
9) and covered paid sick leave, free COVID-19 testing and cost-sharing, unemployment assistance, nutrition assistance, and Medicaid funding support (
10). A third bill addressed economic growth and public health responses, supports for state and local government, and financial supports for individuals and businesses (
11). These legislative agenda items, all signed into law in March 2020, preceded national alarm about COVID-19’s disproportionate impact on oppressed and marginalized communities.
In May 2020, companion bills were introduced that would establish a racial and ethnic disparities task force within the Department of Health and Human Services (HHS) to report outcomes data and federal spending (
12,
13). In July 2020, the Senate introduced a companion bill focused on mental health equity in suicide prevention and mental health services for youths from minority groups (
14,
15). With the current lack of congressional consensus and ongoing negotiations on a Biden-led coronavirus relief plan, communities of color continue to suffer as they await a federal plan, although the recently passed Consolidated Appropriations Act of 2021 has provided additional individual benefits in the form of direct payments, extended unemployment benefits, and rental and nutrition assistance (
16).
For a more effective response, syndemic theory can help guide policy recommendations (at local, state, and federal levels) to effectively tackle all three synergistic conditions—COVID-19, structural racism, and mental health inequities. Several critical policy recommendations that account for syndemic theory are presented below.
Protect “Essential Workers” and Other “Vulnerable” Populations
The spotlight on “essential workers” during the COVID-19 pandemic has exposed risks of exploitation of U.S. workers. Workers deemed “essential” have responsibility for maintaining the infrastructure and functioning of the U.S. economy during the pandemic. These essential, frontline workers are more likely to have lower educational attainment, identify as members of racial and ethnic minority groups, be socioeconomically disadvantaged, and identify as immigrants (
17). Essential workers, who are often in jobs with “low decision latitude” and “high job demands” are also more likely to be granted fewer labor protections and, on the basis of the seminal Whitehall II study (
18), are more likely to have associated psychiatric disorders.
Because this vital community is at high risk, policy interventions must provide protections for these workers. These interventions may seem obvious, but organizing appropriate protections has been difficult without a coordinated strategy. Because some essential workers staff behavioral health care settings, if they become infected, they might affect not only other employees but also patients receiving services in these behavioral health institutions. Thus essential workers in these institutional settings must be prioritized for personal protective equipment (PPE), should be given generous leave for recovery from illness, and should have appropriate insurance coverage to receive treatment for COVID-19–related illnesses and any sequelae, including depression, anxiety, and posttraumatic stress disorder, as well as being given priority for COVID-19 vaccines.
Similarly, institutionalized populations are also at higher risk—structural racism dictates that “vulnerable” populations (often “vulnerable” as the result of chronic oppression) are also commonly marginalized—isolated from other populations in nursing homes, long-term care facilities, and jails and prisons. For example, a higher proportion of Black, Latinx, and Indigenous populations are held in jails and prisons, compared with White populations in the United States (
19,
20). Because many people with serious mental illnesses and substance use disorders are incarcerated or held in long-term care facilities, it is imperative that these vulnerable populations be given appropriate protections, including PPE, adequate space to practice social and physical distancing, access to appropriate testing and treatment protocols for tracing COVID-19 infections, and prioritized access to COVID-19 vaccines.
Engage and Empower Communities
Often, marginalized and oppressed communities lack power and agency in their local county and municipal governing bodies, as well as at the state or federal level. This is the result of numerous structurally racist policies of exclusion that have prevented these communities from holding or sharing power. Often, disinvestment in these communities leads to higher rates of violence and trauma, creating an increased risk of mental health inequities, compared with wealthier communities with greater political power and agency. These marginalized communities are often less likely to have safety nets in place for morbidity, mortality, job loss, and financial insecurity brought on by COVID-19. Policy initiatives that serve to build a sense of community and encourage greater civic engagement within these communities are key (
21). This work is often led by community organizers.
Engagement at the community level also includes bolstering community health interventions. Counties have community health centers and community mental health centers that utilize a model in which people with lived experience and community members are asked to provide representative leadership. Often, the members with lived experience are not fully representative of the community in a real way—local policy interventions to restructure board composition may ensure that the most marginalized citizens have a true voice in creating policy on these community health boards. Traditionally oppressed and marginalized populations must have a role in decision making, not only when COVID-19 contact tracing and testing are being considered but also when ensuring that vaccine dissemination includes all members of the community to most effectively promote equity. Similarly, state and federal policy interventions must invest in these often-overlooked communities by infusing supports for small-business owners and implementing effective aid packages that help support people in the face of food insecurity, financial hardship, and unemployment.
However, communities are often unable to advocate for needed policy interventions because of oppression in the form of voter suppression (
22). Populations that are most likely to be oppressed, including Black, Latinx, and Indigenous people, as well as people with substance use disorders and mental health problems, often encounter systems-level barriers to adequate representation. Ultimately, the downstream effects of lack of representation are inequitable resource allocation, which can be manifest by blatant voter suppression or by more covert tactics, including long voting lines in oppressed and marginalized communities (
23). With regard to the COVID-19 pandemic, lack of equitable resource allocation exacerbates the morbidity and mortality associated with the disease. Local policies must protect and support individuals in voting, including loosening voter restrictions (particularly those restrictions for formerly incarcerated individuals) and adequately staffing polling sites (especially in minority communities). Amid the COVID-19 pandemic, additional voting precautions must be taken, including ensuring that poll workers have access to PPE and that voting stations are arranged to observe social distancing guidelines to most effectively support voter participation while protecting the health of voters who are from marginalized communities. Also, voting by mail should be encouraged, and community health and behavioral health centers can assist with voter registration for patients. At the federal level, legislation to strengthen the Voting Rights Act can help to end voter suppression and other structurally racist policies that prevent effective representation for marginalized communities.
State lawmakers should seek to stabilize Black, Latinx, and Indigenous families and communities through income and housing supports. When the social determinants of mental health are addressed, these families are not destined to fall into the safety net, worsening health outcomes and increasing overall societal costs. Additionally, the intersection of racial injustice and mental health inequities means that many state-level policies disproportionately penalize minority communities. For example, even though rates of substance use disorders are similar among all populations, Black, Latinx, and Indigenous people (especially men) are more likely to be incarcerated for substance use (
24). Because fines and incarceration destabilize family units, contribute to adverse childhood experiences, and place employment and economic barriers on individuals with drug-related offenses, reforming policies to reclassify drug possession penalties from felonies to misdemeanors and supporting a public health approach to treating substance use disorders can promote equity (
25).
Optimize Community-Led Crisis Response Interventions
As a result of the COVID-19 pandemic, mental health crisis services (including the use of suicide hotlines and rapid response to substance overdoses) are on the rise (
26). These crisis services are disproportionately accessed by minority communities. In considering racial injustice as it relates to policing, there is a new emphasis on examining the response to mental health crises—because crisis response is often closely associated with law enforcement. Crisis intervention training (CIT), which aims to educate officers to effectively interact with people experiencing mental health crises, operates under the assumption that the structural inequities within the system are static, but policy interventions can shift the response to people experiencing mental health and substance use disorder crises (
27). Several examples of community-driven mobile crisis response teams (e.g., the Eugene, Oregon, Crisis Assistance Helping Out On The Streets [CAHOOTS] model) exist because local community members have organized and launched such programs. Data on mobile crisis response services demonstrate that people in mental health crises have fewer interactions with law enforcement and greater utilization of mental health care services, and cost savings can be achieved (
28). Financial support is needed at the local, state, and federal levels to effectively execute community-driven crisis response. Ultimately, a coordinated, national policy plan to increase access to mental health care services in the United States is necessary.
Improve Data Collection and Dissemination
The COVID-19 pandemic has shown the importance of data in quantifying inequities and in directing resources to defined populations. As has been done with the COVID-19 Racial Data Tracker, counties and states should develop public health strategies for their mental health data and surveillance programs to monitor COVID-19 risks by race and ethnicity for people with mental health conditions (
29). State departments of health should utilize offices and task forces aimed at eliminating health disparities and inequities to develop action plans for the pandemic-associated mental health response. Local, state, and national COVID-19 case and hospital data should inform targeted mental health awareness campaigns and screening initiatives, with special emphasis on health care workers, who have experienced excess trauma and burnout in their work.
Support School-Based Interventions
It is not yet clear how distance learning is affecting the mental health of students, although some preliminary data indicate that it has slowed the school-to-prison pipeline that exists in the United States, whereas other data suggest a widening of educational inequities (
30,
31). Trauma and adverse childhood experiences lead to worse mental health outcomes for adults, and COVID-19 and interpersonal racism are two main sources of trauma, although not all adverse childhood experience questionnaires have previously incorporated the experience of discrimination as an adverse childhood experience (
32). Thus schools must be redesigned with supports in place for students experiencing racism and trauma and to promote mental health in the face of loss associated with inequitable outcomes resulting from COVID-19. Prioritizing these efforts with policy interventions at the local and state levels could lead to better outcomes and prevention of more serious mental illness.
Expand Financial Supports for Mental Health Service Delivery
Although local and state governments may be financially constrained with economic downturns, increased unemployment rates, increased numbers of uninsured individuals, revenue declines, and budget shortfalls, the COVID-19 pandemic underscores the urgency to maintain progress delivered by state mental health authorities. Programs, services, and supports available through traditional means of service delivery in hospital and community-based settings should be realigned with innovation and technology to increase access through telehealth and home-based solutions. Reducing payment rates for Medicaid providers who offer mental health and substance use disorder treatments or removing behavioral health services and benefits from state plans would worsen inequities and outcomes for Black, Latinx, and Indigenous populations.
As a result of structural racism, poor access to health and mental health care—including lack of parity and insurance coverage—is a primary driver of mental health inequities. The ultimate fix will be universal access to health care for all U.S. residents; however, in the meantime, expanding access to services can be an important first step toward reducing inequities. As a result of the relaxation of state and federal restrictions, telepsychiatry services have expanded significantly during the COVID-19 pandemic (
33). This increased access enables those who are unable to get transportation to appointments to connect for the first time. Telepsychiatry services, paid at a reasonable rate, need to be continued throughout the pandemic and afterward to address access problems for populations affected by service disparities.
Expand Insurance Coverage and Increase Access
A critical component to ensuring health equity is access to health insurance. In states that did not opt to expand Medicaid under the Affordable Care Act, many families remain in the coverage gap, and several areas within these states are densely populated with Black, Indigenous, and Latinx communities. Additionally, many of these states have high per capita rates of COVID-19 cases (
34). For these states, Medicaid expansion still offers a path to reducing mental health inequities in a manner that creates cost savings for states and protects oppressed and marginalized communities (
35).
Although the immediate federal response considered prevention and treatment for the physical manifestations of COVID-19, it is critical to develop policies that address the emotional distress inequitably experienced by oppressed and marginalized communities. The federal government can eliminate cost-sharing (out-of-pocket costs) for mental health and substance use disorders services in the private health insurance market, in government health care programs, and for uninsured individuals who are survivors of COVID-19 or who are spouses or children of COVID-19 decedents.
Federal funding should support the broader range of community behavioral health organizations with prospective payment models and expand behavioral health integration services within Federally Qualified Health Centers and Rural Health Centers (which overwhelmingly provide care to communities of color). Given the expansion of telehealth services, the federal government should support the development of broadband infrastructure to close the technology and digital divide that currently exists, which can improve access to mental health and substance use disorder treatment for older adults, children, and adolescents.
Promote Workforce Diversity
Policies should promote workforce leadership initiatives to ensure that culturally and linguistically appropriate mental health services are provided to oppressed and marginalized communities, those hit hardest by the COVID-19 pandemic. Federal workforce development programs should seek to eliminate the structural racism that persists in research institutions, education and training programs, and clinical mental health and substance use disorder settings that receive federal funding. Disparity impact statements are required for federal grant awards, and, similarly, grantees receiving grants for federal workforce development should be expected to report human resource management data or other plans on antiracism training, diversity and inclusion efforts, and implementation strategies. Organizations that receive federal workforce development grant awards should be required to report racial and ethnic demographic data and should be held accountable for ensuring Black, Latinx, and Indigenous representation at all levels of the organization, including leadership and executive staff. To further enhance the pipeline for mental health professionals, a federal student grant program should be developed to improve access to higher education for students from racial and ethnic backgrounds traditionally underrepresented in mental health care who are interested in mental health professions.
Federal agencies should receive specific funding and resources (beyond the funding traditionally earmarked for this work) to address inequities in mental health that have been exacerbated by COVID-19 and structural racism. The Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity, the HHS Office of Minority Health, the National Institute of Mental Health Office for Disparities Research and Workforce Diversity, the National Institute on Minority Health and Health Disparities, and other analogous federal agency offices should address the social determinants of mental health through direct action plans and policies that prioritize educating, training, and hiring a diverse workforce.
Conclusions
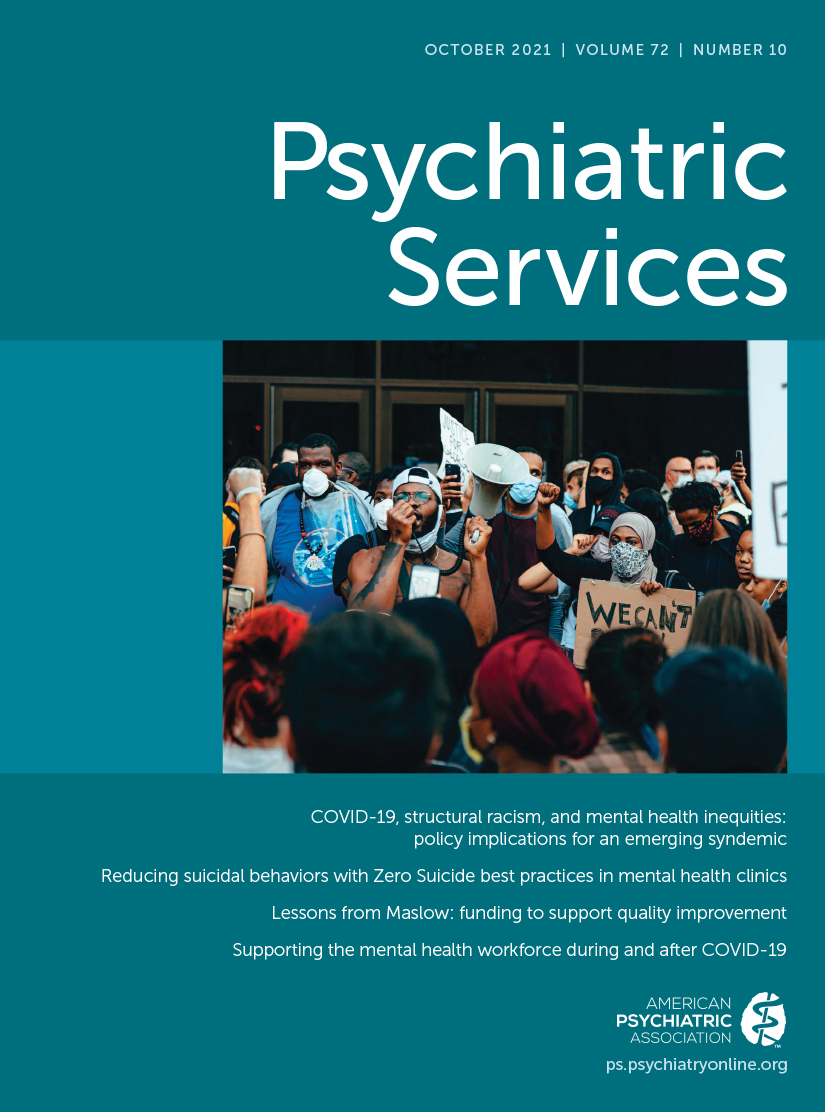
The syndemic of COVID-19, mental health inequities, and structural racism has led to widespread protests and calls for change—in our public health system and in the structures that perpetuate racism. Social injustice has exposed certain weaknesses in the United States in terms of response to COVID-19, structural racism, and access to mental health services. However, it also presents a unique opportunity to correct course and set forth on a new path, one in which solutions take the synergistic effects of these social and health conditions into account.
For all policies, implementing racial equity action plans and impact assessments for policy decisions ensures that laws do not promote structural racism or inadvertently cause harm to Black, Latinx, and Indigenous populations (
36). Emphasis on policy interventions that prioritize equity and justice and that focus on collective health and well-being will ultimately lead us on a more sustainable and equitable path.