In recent years, diversity, equity, and inclusion (DEI) have become increasingly recognized as essential to the practice of high-quality health care in all aspects of medicine, including the direct delivery of patient care and the support of clinicians and other members of the clinical environment (
1). Diversity reflects the physical, social, and psychological differences among individuals, not limited to race, ethnicity, religion, socioeconomic status, education, age, sexual orientation, disability, and gender identity (
2). Equity means guaranteeing access, opportunity, and fair treatment to all individuals in addition to identifying and eliminating barriers that have stymied the full participation of certain groups (
3). Inclusion requires an environment in which all individuals are respected, welcomed, and empowered to fully partake in or contribute to that environment.
Bolstering DEI initiatives can powerfully affect health care disparities. Despite great advances in science, technology, and medicine, health care disparities persist in unacceptable ways. Individuals from underserved and minority groups in the United States struggle with lack of insurance and access to high-quality health care, ultimately contributing to worse clinical outcomes (
1). Psychiatric health disparities are even more stark than those of other medical specialties (
4), and efforts to enhance DEI are long overdue. In addition to inadequate mental health care services for racial-ethnic minority groups, the mental health challenges and needs of these groups require intentional effort, and stigma is a more prominent barrier compared with other populations in the United States. Overall, individuals from minority groups are more likely to initiate treatment later or discontinue mental health treatment compared with individuals from majority groups (
5). A good understanding of DEI contributes to a more profound grasp of what drives mental health care disparities and yields improved clinical outcomes for minority populations.
Recent advances to promote DEI in medicine have targeted specific areas, such as increasing workforce diversity (
1) and training institutional leadership to have a nuanced understanding of DEI, in order to foster these principles in their organizations. Although most of these efforts have targeted potential organizational and high-level system efforts, which are crucial, efforts to empower individuals to champion these efforts in their microenvironments (e.g., academic departments, divisions, teams) have been less emphasized. To our knowledge, best practices of how individuals can practically promote DEI in their health care organizations have not been reported in the medical literature. Accordingly, we aim to describe the design and implementation of our initiative as an example to others planning such changes and to highlight the potentially powerful role of department-level DEI initiatives in establishing best practices pertaining to DEI in an academic medical environment.
Designing a Department of Psychiatry DEI Committee
When the idea to create a DEI committee was conceived by our department chair, a small task force consisting of the department chair and two faculty leaders assembled to brainstorm how to engage the psychiatry department of a large urban academic medical center in the northeastern United States with over 200 academic, clinical, and research staff. The task force then consulted key department stakeholders (including clinicians, administrative staff, and researchers) about the role the DEI committee could play and the initiatives the committee should focus on. To assess staff interest in committee participation, the task force developed a brief needs assessment (see
online supplement) to facilitate conversations with department stakeholders.
Integrating information gathered from conversations with stakeholders, and after discussions with department leadership, the task force developed and proposed a mission and vision statement. These were reviewed with department leadership and staff volunteers on the inaugural committee. The mission and vision statements were disseminated to department faculty and staff before being published on the department website. These statements served as a reference for the entire department about what the DEI committee set out to accomplish. Additionally, they were incorporated with other promotional materials about the department for recruitment purposes across multiple training programs.
The inaugural DEI committee evolved into a multidisciplinary group of junior and midcareer physicians, social workers, nurses, psychologists, research staff, and trainees across these diverse disciplines and roles. Although the committee members and leaders do not self-identify as DEI experts, most have had a longstanding commitment to advocating for DEI in their work or academic medical environments. Notably, a majority of the committee members are not from underrepresented minority groups within medicine.
Sample vision statement.
The Brigham and Women’s Hospital (BWH) Department of Psychiatry will serve as an innovative and national leader in culturally competent practice, education, and research.
Sample mission statement.
The BWH Department of Psychiatry faculty, staff, and students are committed to supporting a culturally responsive community of clinicians, educators, and researchers who follow diversity and inclusion value-based practices, including recognizing and celebrating the diversity of our departmental community; provision of mentorship for diverse faculty, staff, and students; integration of diversity frameworks within educational curricula across training programs; attention to and adoption of culturally responsive clinical care practices; openness to lifelong learning practices within the departmental community on diversity topics; prioritizing the recruitment and retention of diverse faculty, staff, and students within the departmental community; and development of outreach activities within the greater Boston community.
Structure of a DEI Committee
Based on feedback from the inaugural committee members and department leadership, the committee would have two cochairs with 2- to 3-year term limits, and the group would meet monthly. To foster the participation of the entire department, every member of the department was sent a calendar invitation and an announcement (from the department chair’s office), which was repeated periodically as a reminder of the group’s existence, especially for newer department members and trainees. In addition, the first meeting of the committee was celebrated with a luncheon to officially establish its existence.
Because the department at our academic medical center is spread out in different locations, the initial meetings were held onsite at the two primary locations, with a teleconference option. The number of people who met onsite was about the same as the number who used the teleconference option. The teleconference format facilitated a smooth transition to an all-virtual format during the COVID-19 pandemic. Eventually, as the pandemic progressed, we saw an increase in group membership, and meetings were transitioned to Zoom (
6).
The cochairs developed and disseminated an agenda to all members 3 to 7 days before each meeting. The meeting agenda allowed a safe forum to discuss diversity dilemmas within clinical or work-related interactions, an opportunity for different diversity leaders in the hospital community to share their work, and an opportunity for anyone in the department to receive feedback on DEI-related educational material. One of the two cochairs facilitates the discussion, and each meeting provides an open forum for department members to consult on critical incidents pertaining to DEI. To emphasize the importance of creating a safe space for dialogue, we do not record the sessions. However, after each meeting, a summary of the topics discussed and actions assigned to individuals is e-mailed to members of the committee.
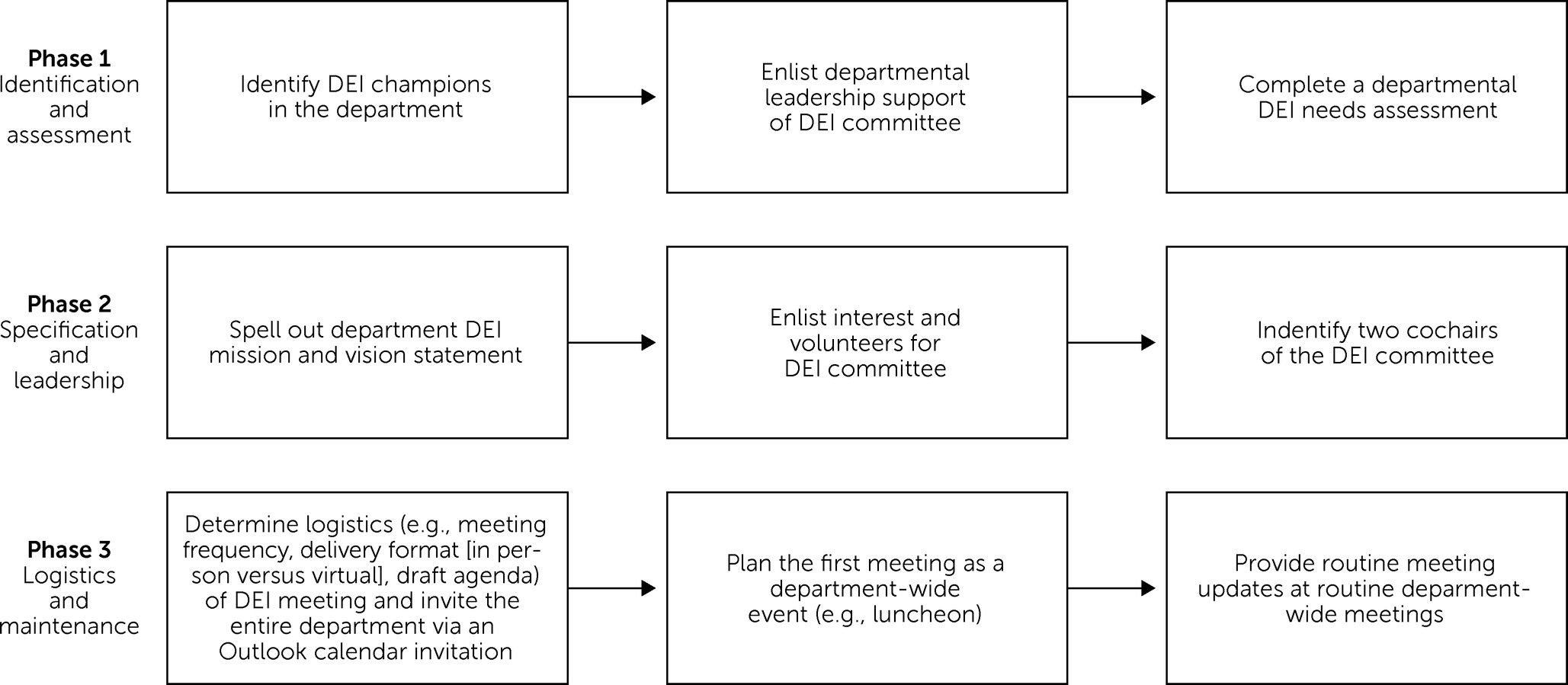
Figure 1 shows a schema of the structure of the DEI committee.
DEI Initiatives
Over 3 years, the DEI committee has pioneered several initiatives in the department to promote diversity, inclusion, and equity. On the basis of informal feedback provided by various department members, the two initiatives that have had the greatest impact are diversity dilemmas and colloquia.
At the beginning of every meeting, participants are invited to share incidents, or diversity dilemmas, they have encountered either directly or indirectly in the preceding month. The group offers suggestions for remediation, and the committee uses its departmental authority to engage individuals involved in the problem to work toward a solution. Thus, committee members and cochairs deliver recommendations on behalf of the DEI committee.
Table 1 provides examples of diversity dilemmas that the group has addressed. Additionally, the committee has created formal presentations, or colloquia, on DEI topics for use as training materials in their various divisions (e.g., a cross-cultural training module to engage social workers regarding care of patients with values, beliefs, and patterns that can cause tension in the clinician-patient relationship).
In addition to the initiatives described above, the committee has provided opportunities for faculty in different clinical settings to collaborate on scholarly projects, including presentations and writing projects. One such collaboration resulted in a recent peer-reviewed publication describing diversity issues in the context of COVID-19 (
7).
Challenges
The DEI committee has experienced several notable challenges. First, it was difficult to share the ongoing progress of the group with the entire department; occasionally, department members reported that they were unaware of the group. Committee members were given the responsibility to remind members of their divisions or clinical teams about the group. However, it was challenging to identify avenues for routine and integrated updates about the DEI committee’s ongoing meetings and activities.
Although there was a robust level of commitment from multidisciplinary clinicians, it was difficult to engage trainees from psychiatry training programs to participate in the group. Trainees are essential members of any academic department because they are on the front lines of patient care, so it would be beneficial to get their input on various problems that arise in the clinical settings. When engaged, trainees can also help disseminate DEI initiatives and can serve as department champions to implementing the mission and vision of the DEI.
Lessons Learned and Recommendations
Over the past 3 years of work with the DEI committee, it has become clear that department leadership is essential for the group to thrive. The committee cochairs have provided detailed updates of the committee’s activities to the department chair, who in turn has reaffirmed that DEI is a priority. Accordingly, the committee has been encouraged to bring clinical and operational issues to department leadership and has been empowered by the department chair to develop action items based on issues raised. A multidisciplinary membership of the DEI committee has encouraged a more holistic view of problems that have arisen in different facets of the department. A DEI report has become part of the biannual department staff meetings, an opportunity to share the work of the committee more broadly within the department and to motivate participation.
Moving forward, increasing trainee participation will require targeted messaging and coordination with all training programs (including residency and fellowship). It will also be useful to explore potential barriers to trainee participation (e.g., time constraints and scheduling conflicts with clinical and other training and DEI activities). One incentive might be to offer a leadership role for trainees who are specifically interested in DEI to foster ownership and encourage other trainees to promote attention to DEI issues in their clinical work. It may also be helpful to institute routine data collection via surveys of the department to more formally assess the impact of the DEI committee.
Conclusions
Cultivating a culture of diversity, equity, and inclusion is critical in health care organizations as we learn more about the negative effects (e.g., increased morbidity and mortality for individuals from underserved populations) of systemic racism on health care disparities (
1). Based on our experience, we believe deliberate efforts to promote DEI initiatives in psychiatry departments are imperative and should involve all department members, not just leaders in the academic medical institution. We have found that a DEI committee is a powerful vehicle to drive a cultural shift toward engaging all individuals in a department to promote DEI. We hope that the information shared here will inspire academic psychiatrists to take initiative in their own academic departments.