In 2011, the National Institute of Medicine released a report highlighting the finding that U.S. adults identifying as lesbian, gay, bisexual, or transgender/gender nonconforming (LGBT) experience higher rates of general medical and mental health problems compared with their cisgender and heterosexual peers (
1). Similar findings have been identified in subsequent studies that used a nationally representative sample, underscoring the extent of these discrepancies (
2,
3). These disparities, including increased risk for depression and suicide, are also apparent among LGBT youths (ages <18 years) (
4,
5). However, few studies have reported representative mental health data from individuals of all ages to provide insight into the degree of these disparities during different life stages.
To identify age-related differences in mental health problems, it is necessary to examine outcomes across developmental stages and identify whether and when changes in mental health occur. The mental health of older sexual and gender minority (SGM) adults is especially understudied, and it is therefore difficult to make comparisons by age. Data on the well-being and needs of this population are lacking because of inconsistent collection of information on sexual orientation and gender identity in many national health surveys (
6). Moreover, bisexual, transgender, gender-nonconforming, and gender-diverse individuals are rarely examined as distinct subgroups, separate from gay or lesbian respondents, thereby hindering comparison across studies.
The current evidence base on older SGM adults is derived primarily from community-based convenience samples, with few probability or nationally representative samples (
7). The findings of these studies are often mixed. Data from the California Health Survey (conducted in 2005 and 2007) found that, compared with their heterosexual counterparts, gay men and lesbians ages 50–70 had 45% and 35% higher odds of psychological distress, respectively (
8). The 2015 iteration of the survey, however, found no differences in psychological distress between older heterosexual and lesbian, gay, or bisexual adults (
9). The Caring and Aging With Pride study, a 2014 cross-sectional survey in Washington State, reported that 29% of older gay and lesbian adults experienced depressive symptomatology, and rates of depression were similar across minority sexual orientation subgroups (
10). In the same study, compared with cisgender SGM peers, older gender-diverse adults reported higher rates of distress, depression, and suicidal ideation (
11). Findings from other studies, however, have indicated that older SGM adults display more qualities consistent with healthy aging (
12,
13), including lower rates of psychological distress and suicidal behavior, than do younger SGM individuals (
14). This finding is also consistent with studies in the general population that have found higher rates of psychological distress among younger age cohorts compared with older age cohorts (
15).
Numerous psychosocial and health disparities have been described as risk factors for mental distress among older SGM adults. High rates of smoking and excessive alcohol use have been noted, in comparison with the non-SGM population (
16,
17). Indicators of poor general medical health, such as obesity, lack of exercise, disability, and barriers to accessing medical care due to financial limitations or fear of discrimination, have also frequently been noted (
10,
16,
18–
23). Factors of “minority stress,” including past and present experiences of prejudice and victimization, can also continue to influence mental health across the life span. For instance, older lesbian, gay, and bisexual adults reported an average of six instances of discrimination or victimization throughout their lives, which was highly correlated with depression and disability (
10,
24).
In this study, we aimed to clarify these mixed findings for older SGM adults in the limited literature on the topic and to use data from a national sample to determine differences across age groups in the SGM population. Our study offers quantitative data on trends of mental distress across the full range of adult developmental stages, which may advance our understanding of age-related differences in mental distress. We hypothesized that older SGM adults would report better mental health outcomes than younger SGM adults, following the trend of findings from recent health surveys. Our findings may help inform the provision of psychiatric services to improve mental health outcomes among SGM adults.
Methods
Study Population
The current study used data from the 2014–2018 Behavioral Risk Factor Surveillance System (BRFSS), the largest continuously conducted national health surveillance survey (
https://www.cdc.gov/brfss). Eligible respondents were adults ≥18 years old. Data from 37 states that completed the sexual orientation and gender identity module from 2014 to 2018 were included (see Table S1 in an
online supplement to this article). This sample represented approximately 43.7% of the U.S. population (weighted, N=143,289,672 of 328,000,000). The study was determined to be exempt from institutional review because BRFSS data are publicly available and deidentified.
Measures
Dependent variables.
Mental distress was assessed with the following question: “For how many days during the past 30 days was your mental health not good?” Responses ranged from 0 to 30 days. For this study, two measures of mental distress were used: mean days of mental distress and prevalence of frequent mental distress (≥14 days of distress in the past month). The construct validity of this definition of frequent mental distress has been previously established, including its association with diagnosable depressive symptomatology and serious mental illness (
25,
26).
Independent variables.
The age of respondents was categorized into six groups (18–24, 25–34, 35–44, 45–54, 55–64, and ≥65 years). Sexual orientation and gender identity were determined from responses to the sexual orientation and gender identity module questions. These questions asked, “Do you consider yourself to be [straight, lesbian or gay, or bisexual]?” and “Do you consider yourself to be transgender (if yes, male-to-female, female-to-male, or gender nonconforming)?” Respondents who identified as cisgender were classified as gay or lesbian, bisexual, or heterosexual. Transgender and gender-nonconforming respondents were classified as a single gender-diverse group because of the study’s limited sample size. All participants who responded that they considered themselves to be transgender were classified as gender diverse, regardless of their response to the question about sexual orientation.
Control variables.
Sociodemographic measures included sex, race-ethnicity, education level, relationship status, employment status, and annual income. Health care access and disability measures included health care coverage and presence of multiple chronic medical conditions. For this study, sex was meant to denote natal sex. Recorded sex has been shown to primarily follow natal sex for gender-diverse respondents, although the potential for misclassification has been acknowledged, particularly before 2016, when interviewers were permitted to assume sex on the basis of vocal timbre (
27).
Statistical Analyses
Analyses were performed with STATA/MP, version 17.0, and accounted for the complex survey design, with sample weights recalculated to account for pooling of multiple years. Only respondents with complete data were included (see Figure S1 in the
online supplement for missing measures and sample selection). Descriptive statistics and chi-square tests were used to assess differences in measures across sexual orientation and gender identity subgroups. Zero-inflated negative binomial regression (
28) and logistic regression models were fit to evaluate trends in mental distress or frequent mental distress, respectively, across age categories. Estimates were calculated from the predictive margins of the interaction term between age and sexual orientation/gender identity, controlling for the main effects of age, sexual orientation, and gender identity as well as sex, race-ethnicity, education level, employment status, annual income, health care coverage, presence of multiple chronic medical conditions, state of residence, and year of survey participation. Post hoc Bonferroni-adjusted significance tests were conducted to determine pairwise differences between different strata.
Results
The study sample included 734,670 (95.6%) heterosexual, 12,166 (1.8%) lesbian or gay, 12,609 (2.1%) bisexual, and 3,096 (0.5%) gender-diverse respondents (total N=762,541). The weighted characteristics of the sample, stratified by sexual orientation and gender identity, are shown in
Table 1. Sexual orientation and gender identity subgroups differed significantly (p<0.001) across all covariates, except for the presence of multiple chronic medical conditions (coded as zero to one vs. two or more conditions) (
29). Compared with their heterosexual counterparts, SGM respondents were generally younger, more ethnically diverse, more likely to be single, and more likely to report lower rates of health care coverage.
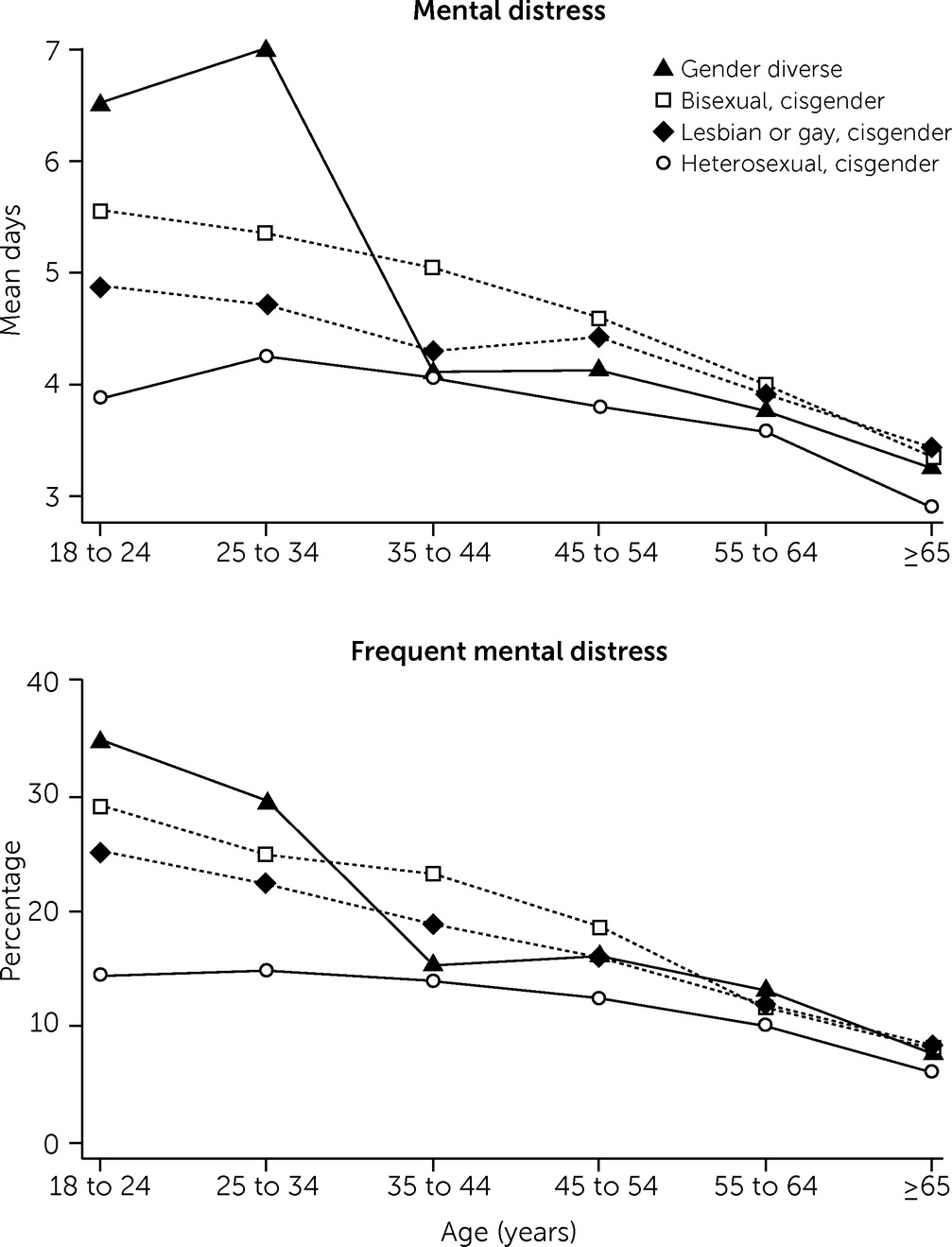
Trends in the adjusted mean days of mental distress and the rate of frequent mental distress are shown in
Figure 1 and
Table 2 (see Table S3 in the
online supplement for full regression results). Adjusted mean days of mental distress and rate of frequent mental distress decreased linearly with increasing age. Among respondents ages 18–24, gender-diverse individuals experienced the highest level of mental distress (mean=6.5 days, frequent mental distress=34.5%), followed by bisexual (mean=5.6 days, frequent mental distress=29.0%), gay or lesbian (mean=4.9 days, frequent mental distress=25.0%), and heterosexual (mean=3.9 days, frequent mental distress=14.5%) respondents. For both mental distress measures, all SGM subgroups significantly differed from cisgender individuals among those ages 18–24 (p<0.05), but not among those ages 45–54, 55–64, or ≥65. Differences between the ≥65 and 18–24 subgroups were largest for gender-diverse individuals (mean days of mental distress=−3.3, frequent mental distress=−26.8 percentage points), followed by bisexual (mean days of mental distress=−2.2 days, frequent mental distress=−20.6 percentage points), gay or lesbian (mean days of mental distress=−1.5 days, frequent mental distress=−16.7 percentage points), and heterosexual (mean days of mental distress=−1.0 days, frequent mental distress=−8.3 percentage points) respondents (p<0.05).
Discussion
In this study, we analyzed mean days of mental distress and the rate of frequent mental distress among SGM adults and their heterosexual counterparts and found a linear reduction in both measures with increasing age for all SGM subgroups examined. The largest differences were noted among gender-diverse respondents. These data suggest clear differences in SGM individuals’ mental health by age. More recent data indicate that older SGM adults are as healthy as their heterosexual counterparts (
9), an observation supported by the findings from the present study. The time frame of the data collected for this study included significant legislative changes and periods of uncertainty for SGM individuals. Mental distress among SGM adults significantly increased during this same interval (
30). How adults in different developmental stages experience such shifts in public policy is unknown.
Possible policy and practice implications of the study’s findings include addressing the increased mental distress among SGM young adults by prioritizing service delivery and reducing barriers to accessing mental health services for individuals in this age group. Although the argument could be made that frequent mental distress may decrease without intervention over the course of the life span, the higher mental distress among SGM adults, compared with that among heterosexual age peers, does not resolve until later in life (ages ≥45 years). As such, to value quality of life for SGM adults across the life span, the results of our study support the development of additional resources and services for SGM young adults so that reduction of mental distress can begin much earlier in life.
One possible explanation of the study’s findings is that, over time, older SGM adults may have learned effective coping strategies that buffer against the health consequences of discrimination. To counteract the negative effects of discrimination, it may be effective to support the implementation of mental health services for SGM young adults, such as affirmative cognitive-behavioral therapy (
31). Programs such as Project Youth Affirm specifically target salient stressors for SGM young adults, such as minority stress, and enhance coping skills to combat maladaptive thoughts and beliefs. Acquisition of such skills early in life may lead to improved mental health outcomes earlier in life. However, we note that coping skills and experiences of discrimination were not assessed in this study. Moreover, other processes and factors, such as social and family role transitions, changes in substance use, employment, and economic stability, occur throughout adulthood and may also contribute to changes in well-being and distress over time, independent of or in conjunction with the development of coping skills. The results among older adults in the present study may also be explained by the creation of a robust social support network during the life span. This factor may be addressed by supporting programs such as gay-straight alliances in educational settings and by making local LGBT centers attractive and accessible to young adults so that an affirming social network can be created early in life.
The strength of our study was its use of a large, population-based sample that provided sufficient power in analyses to examine individual sexual orientation and gender identity subgroups. Community-derived samples, although enabling more nuanced psychological measurements, are susceptible to a multitude of biases that hinder generalizability to the overall SGM population. Limitations of this study included that sampling was done from a large selection of, but not all, U.S. states and a repeated cross-sectional, rather than longitudinal, design. The analyses in this study did not examine within-person changes or improvements in distress over time; analyses represented cross-sectional comparisons among groups. Additionally, when BRFSS response rates were especially low for states (<40%), racial-ethnic minority groups, women, and younger adults were more likely to be underrepresented (
32). Younger adults and gender-diverse adults may have been undersampled, which may have inflated variability in the measured outcomes, the ability to detect changes, or both.
The impact of a “survivor effect” in these results must also be taken into account. It is necessary to consider whether individuals with poorer mental health outcomes may have died by suicide or other causes (e.g., substance use–related morbidity) earlier in life, thereby skewing the results for the older age groups. This alternative explanation of our results would suggest that, instead of providing evidence of healthy aging, our findings indicate a regression to the mean due to premature death. As such, it is important to view these results as only preliminary evidence of healthy aging until rigorous longitudinal studies can be conducted. Although an increase in suicide attempts for SGM adults, relative to cisgender, heterosexual adults, is well documented in the literature (
14), evidence is less robust for a difference in rates of deaths by suicide between SGM and non-SGM adults, because death records typically do not document sexual orientation (
33). However, some evidence indicates that transgender adults die by suicide at twice the rate of cisgender adults (
34), and SGM women have approximately double the overall mortality rates of heterosexual women (
35). Additionally, the precipitous reduction in mental distress between ages 25–34 and 35–44 in the gender-diverse subpopulation may correspond to the benefits of gender-affirming medical and surgical treatments for gender dysphoria (
36). However, because transition status was not measured, this explanation is purely conjecture.
Conclusions
Significant disparities in mental health exist among SGM young adults relative to their heterosexual, cisgender counterparts. These differences, however, were not observed in older subpopulations in our sample, providing preliminary evidence of positive life trajectories among SGM adults. Longitudinal studies are needed to better establish the precise factors underlying this observed trend. This study adds to the established literature that SGM young adults are in great need of mental health services because of the disproportionately high levels of mental distress in this group. Initiatives to further explore this discrepancy in mental health experiences are worthwhile to close the mental health gap between SGM adults of different ages and to improve mental well-being at an earlier age.