The COVID-19 pandemic has resulted in more than half a million deaths in the United States. The virus continues to cause substantial personal, social, economic, and political discord, despite ongoing efforts to slow its spread (e.g., wearing masks, maintaining social distance, staying home, limiting business operations) and the recent rollout of vaccines. COVID-19 has disproportionately affected communities of color (
1). Furthermore, the broad impacts of COVID-19 are cumulative and compounded by existing issues of substance use and social inequalities. The opioid epidemic in the United States has resulted in more than 450,000 overdose-related deaths. The three waves of the opioid epidemic have been driven by prescription opioids in the 1990s, a resurgence of heroin and synthetic opioids (e.g., fentanyl) in the mid-2000s, and the COVID-19 pandemic in the current wave.
Underlying these health crises, systemic racism (i.e., policies and practices that favor some racial-ethnic groups over others) has precipitated and maintained social, health, and economic disparities among many communities with many individuals who identify as Black, Indigenous, and people of color (BIPOC). However, institutions and policy makers have often taken the stance that racism does not play a role in the lived experiences of minority communities (i.e., color-blind racism) (
2). This view disregards the idea that highly racialized issues (e.g., food insecurity) affected minority groups before the pandemic. In reality, these issues were caused by systemic racism and have been exacerbated by the COVID-19 pandemic and opioid epidemic.
A syndemic is the compounding of two or more health conditions that exacerbates poor outcomes for a population or within a given time frame. A COVID-19, opioid use, and racism (COR) syndemic framework is needed that considers these three crises as jointly occurring and related, with overlapping social determinants. This framework is critical to developing meaningful interventions that view the drivers of illness from a synergistic perspective. This concept is particularly important in addressing health inequities where multiple comorbid illnesses unduly affect certain disadvantaged populations, causing cumulative and/or cascading health burdens and needs that may be reciprocally reinforcing. Failure to consider each issue as part of a syndemic leads to inefficiencies in a systemic approach to addressing the root causes and harms of each crisis.
Impact of Systemic Racism on Opioid Use Outcomes
For years, the perception prevailed that opioid abuse was a crisis among predominately White populations, largely excluding many BIPOC communities from the focus of prevention and treatment. However, disparities based on intersections of gender, race-ethnicity, and age have been documented. Racial-ethnic disparities, including greater increases in overdose deaths from 1999 to 2017 among Black/African American communities compared with White communities, have been particularly persistent (
3). Furthermore, substance use treatment is less accessible to BIPOC populations than to White populations. This deficit in accessibility is due to extensive systemic factors that limit access to treatment facilities and impede treatment completion, including housing instability, socioeconomic hardship (e.g., unemployment), availability and cost of treatment, and physician bias.
It is important for researchers and clinicians to recognize and understand the considerable distinctions between perceptions about the opioid epidemic, compared with previous national concerns about substance use (e.g., crack and cocaine), which have criminalized members of racial-ethnic minority groups and led to greater rates of policing, arrests, and incarceration among BIPOC communities. Although our understanding of effective substance use prevention and treatment has grown over the past five decades, BIPOC communities continue to receive unequal and inadequate care for substance use disorders. Despite engaging in substance use at similar rates compared with White populations, members of racial-ethnic minority groups (particularly Black/African American people) continue to be more likely to be incarcerated for drug-related offenses, rather than referred to needed treatment facilities (
3). Furthermore, nearly 50 years of discordant incarceration rates between White and BIPOC populations continue to exacerbate persistent social and economic adversity among BIPOC communities (e.g., limited employment opportunities, more restricted access to resources, inability to vote). Thus, there is a need to understand and address the bidirectional pathways between systemic racism and substance abuse, particularly given the strain of the COVID-19 pandemic, and to address these issues with institutional and policy-level change.
Pathways Between Opioid Abuse and COVID-19
In addition to considering the racial underpinnings of the opioid epidemic, the compounding effect of COVID-19 on opioid use must be better understood to inform any significant progress in public health and policy. According to data from the Overdose Detection and Mapping Application Program (ODMAP) (
4), 16% more overdoses occurred in February 2020, at the onset of the COVID-19 pandemic, than in February 2019, and 42% more occurred in May 2020 compared with May 2019. Early research has begun to shed light on several biological factors in overdose deaths, with the increased rate of fatalities suggesting a bidirectional relationship (
5). For individuals using opioids, the compromising impact of COVID-19 on lung function increases risk of fatal drug overdose. Simultaneously, individuals with heavy opioid use are prone to hypoxemia (low blood-oxygen levels), which has been shown to increase the risk of COVID-19’s adverse consequences.
Individuals in recovery from addiction have also faced a host of novel disruptions and barriers to treatment as a result of the pandemic. Attempts to limit the spread of COVID-19 through social isolation resulted in the closing of treatment facilities and decreased access to support systems. With fewer harm reduction services, such as needle exchange programs and naltrexone administration and dispensation, and decreased bystander intervention because of social distancing and stay-at-home orders, rates of overdose have skyrocketed since the beginning of the COVID-19 pandemic. ODMAP data (
4) have shown that more people are dying more rapidly as a result of opioids than before the pandemic because of insufficient intervention and a halt in preventative care.
In addition to the biochemical interaction of concurrent COVID-19 and opioid use in an individual’s body, the combined impact of these two crises is seen in the various psychosocial factors predisposing individuals to opioid use and greater rates of relapse. COVID-19 restrictions, increasing unemployment, and loss of housing have left communities that were already affected by substance use further ravaged by stress and financial hardship and with little-to-no structural support. Social distancing measures and loss of loved ones to COVID-19 have exacerbated feelings of fear, anxiety, grief, and isolation. These factors, including limited access to caregivers and support systems, have coalesced in a devastating emotional toll and a potential nationwide trigger for relapse.
Systemic Racism and COVID-19
As the COVID-19 pandemic persisted throughout 2020 and into 2021, the pathways between systemic racism and COVID-19 became more distinct. A large proportion of BIPOC individuals work in settings that were deemed essential during the pandemic (e.g., grocery stores, warehouse delivery services, and food processing facilities). Despite the importance of these roles in providing fundamental services, these occupations often have limited health care access and insurance coverage and increased risk for exposure to COVID-19. Systemic racism also affects the frontline health care workers from BIPOC communities, who may be the most affected by COVID-19 (
2). Yet the media has often portrayed frontline workers as White medical personnel who are single-handedly fighting off the virus. The “heroes” narrative takes responsibility from the state and national handling of the pandemic and places it on individuals, who are shamed for protesting inadequate or unsafe work conditions, and minimizes the crucial role of BIPOC health care workers.
Chronic exposure to racism and discrimination, along with preexisting health conditions (e.g., obesity, diabetes, and hypertension) that are exacerbated by systemic racism and that disproportionately affect members of racial-ethnic minority groups, may heighten risk for morbidity and mortality after COVID-19 infection (
6). Incarcerated individuals are at even greater risk for contracting COVID-19, further reinforcing the need to address the persistent systemic injustice that maintains ongoing disparities in outcomes related to COVID-19 and other illnesses.
Preexisting inequalities in health care have also persisted into the pandemic era. Members of racial-ethnic minority groups, particularly Black/African American people, may have limited access to testing sites because of distance or site requirements. For example, drive-through testing sites may be difficult to navigate for individuals without a car or driver’s license (
6). Black/African American people are also more likely to be turned away for treatment or to have their symptoms minimized by providers across medical systems (
6), leading to inadequate or lower-quality care for COVID-19 and other illnesses. When members of racial-ethnic minority groups contract COVID-19, they are often treated by medical staff who lack racial training. This situation puts these individuals with COVID-19 in the position of being stereotyped, with their assumed preferences for care driven by provider bias that can be potentially life threatening (
7). Furthermore, vaccines were substantially less likely to be distributed in BIPOC communities during initial rollout efforts. All of these factors, combined with historical mistreatment of minority groups by the fields of medicine and research, contribute to mistrust among BIPOC communities, which drove initial vaccine hesitancy and may maintain disparities related to COVID-19.
Influence of the COR Syndemic on Traumatic Stress
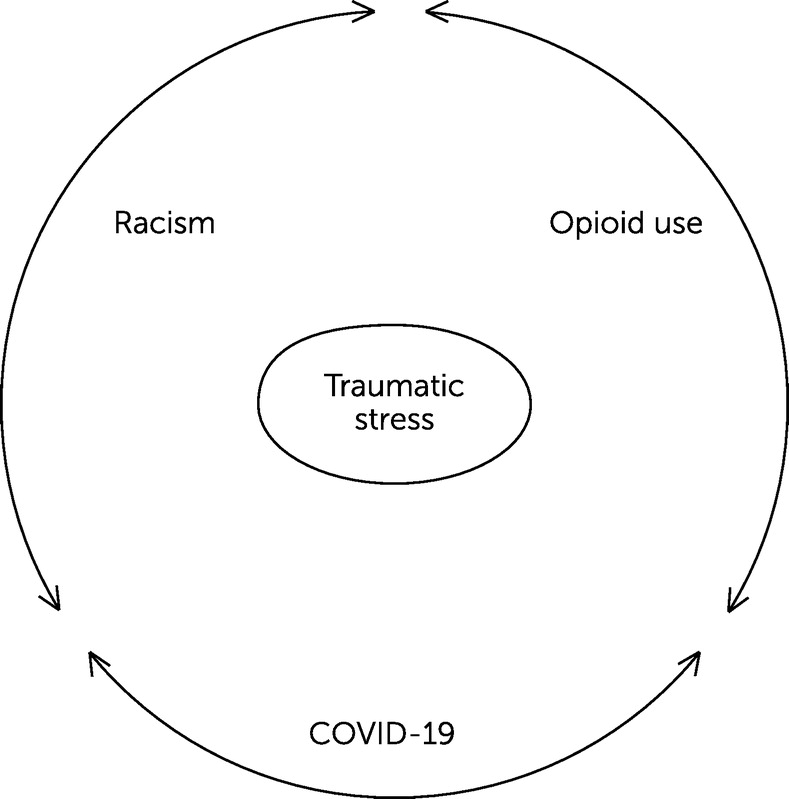
The overlapping and synergistic effects of the three epidemics—COVID-19, opioid use, and systemic racism—have led us to propose an integrative framework that allows us to consider research, practice, and policy implications. In conceptualizing these three crises as a syndemic, we are able to recognize their interconnectedness (
8). As seen in
Figure 1, we center traumatic stress as a critical underpinning that links each of the three crises in the COR syndemic.
Traumatic events may be categorized into three general types: those with intentional human causes (e.g., terrorist attacks, combat, sexual and/or physical abuse), those with unintentional human causes (e.g., industrial or motor vehicle accidents), and those with nonhuman causes (e.g., floods, earthquakes, or life-threatening illness). Each category of traumatic event has an extensive body of literature associated with each of the three crises, considered separately—for example, COVID-19 losses that are due to illnesses, deaths, and socioeconomic impacts; opioid losses due to overdose deaths and the known traumatic determinants of opioid use disorder (i.e., childhood physical and sexual abuse, childhood adversity, adult intimate partner violence), and racial pandemic-related stressors, including racial trauma (i.e., chronic microaggressions, discrimination, and inequalities).
Enhanced understanding of the larger risk environment and the inextricable links between multiple pathways (e.g., biological, behavioral, environmental, genetic, and structural determinants) on health outcomes should shape public policy making, which at present is most often fractured and siloed, leaving clients, families, and health care providers to work across systems and funding structures that do not communicate. For these reasons, it is important to embrace a perspective that views the COR syndemic through a structural competency lens (
9), which does not define social determinants as having exclusively biological or cultural origins but provides new and innovative educational paradigms (
10) that promote skepticism in race-based diagnostic differences, creation of real working relationships between systems with all involved providers, and adoption of an antiracism stance when encountering barriers to integrated care. For example, training for mental health and substance use providers in the concept of the COR syndemic and its likely overlap in diagnostic symptoms and features will enhance treatment decision making. Methods are also needed to incentivize collaboration across typically disparate systems of care through funding, administrative commitment to bridging gaps in care, and creation of positions that can serve as ambassadors across systems (i.e., peer specialists who work in integrated health and substance use community and/or hospital programs).
Finally, how does one adopt an antiracism stance when encountering barriers to care? Top-down recognition of the COR syndemic is needed. Such recognition supports an antiracist and trauma-informed position and frames considerations about inequalities at every level of treatment planning—from program administration, to hiring and retention policies and practices, to patient access to care, and to systems that promote “one-stop shopping.” All of these are examples of ways to enhance integrated and informed health care that takes into account the mental health– and substance use–related needs of disadvantaged populations when addressing multiple, complex, and intersecting problems. Finally, funding for research and practice must be broadened to include trauma-informed care across aspects of the COR syndemic.
Conclusions
We have presented a syndemic framework to show the shared, interwoven elements of the COVID-19, opioid use, and racism crises, centering traumatic stress as a key underpinning and considering the role of other social determinants. We have reviewed the ways the COVID-19 and opioid use crises have disproportionately affected BIPOC populations and suggested that the fields of social medicine and policy apply a trauma-informed framework to address the COR syndemic. We now call for action, particularly by those in social medicine, to develop new and innovative frameworks for connecting systems and integrating care.