The COVID-19 public health crisis forced the addiction treatment system to pivot from delivering most addiction treatment in person to delivering treatment via telehealth (
1–
3). Prior to the pandemic, only 27% of specialty addiction treatment facilities in the United States reported having telehealth capabilities (
4). Among individuals with private insurance and Medicare, telehealth was used in 0.1% of addiction treatment visits (
5). Telehealth adoption was constrained by federal and state laws and health plan policies. For example, the federal Ryan Haight Online Pharmacy Consumer Protection Act requires practitioners to conduct an in-person medical evaluation before prescribing controlled substances, such as methadone and buprenorphine. Prior to the pandemic, Medicaid programs often limited the types of technology that could be used for telehealth (e.g., not telephones), the provider types who could deliver telehealth (e.g., not nurses), and the locations where patients could receive telehealth (e.g., not in their homes) (
6). Concerns about patient safety, fraud, quality, and cost underlie these restrictions (
5,
7). Of special relevance to addiction treatment are requirements for in-person visits to prescribe buprenorphine and for in-person intake and physical exam to initiate methadone treatment (
8). To maintain access to treatment during COVID-19, federal and state agencies temporarily eased many telehealth restrictions (
9). Policy makers and payers are now considering which of these flexibilities should be maintained.
To address these questions, we collected qualitative and quantitative data from California specialty addiction treatment providers and policy leaders about their experiences and their perceptions of the benefits and challenges of using telehealth. Prior to the pandemic, California Medicaid had few restrictions on addiction treatment via telehealth (
10). However, because California’s addiction treatment system is county based, county governments also had to give permission for telehealth-delivered addiction treatment, and prior to the pandemic few counties had done so. In 2019, only 25% of California specialty addiction treatment providers reported using telehealth (
11). When the governor issued the first stay-at-home order in March 2020, California counties quickly shifted to allow substance use disorder services to be delivered via telehealth.
This study aimed to clarify whether the research evidence on the efficacy of telehealth-delivered addiction treatment and the experience of providers using telehealth during the COVID-19 pandemic support continued use of telehealth after the pandemic and, if so, under what circumstances. It also aimed to identify substance use disorder treatment services and populations to target for additional research.
Methods
We collected information on telehealth efficacy and effectiveness through a review of published studies on the comparative efficacy of telehealth addiction treatment, a survey of addiction treatment organizations in California, and interviews with treatment providers and other stakeholders.
Literature Review
We conducted a search of MEDLINE’s PubMed database and Web of Science to identify studies published in English from 2010 to 2020 and identified additional articles through a snowball approach. We defined telehealth as synchronous communication between patients and providers via telephone or videoconferencing for assessment, diagnostic, or treatment purposes. We limited the review to studies that compared the efficacy of telehealth with in-person treatment for substance use disorders and that undertook a randomized controlled trial (RCT) or used another controlled comparative design.
Provider Survey
We conducted a survey of California addiction treatment organizations to understand their use and perceptions of telehealth. We identified organizations using the Substance Abuse and Mental Health Services Administration (SAMHSA) Behavioral Health Treatment Services Locator and information provided by the California Department of Health Care Services. We surveyed only organizations that accepted Medicaid or other county funding and asked organizations to respond to questions for their whole organization, not for specific facilities. The survey was sent to the organization’s leadership, who could also have been clinicians. We collected data from September to November 2020 by using the Voxco online survey platform and analyzed the results with Stata, version 16.1.
Of the 412 eligible providers, 100 responded—a 24% response rate. More than half of the 100 responding organizations (55%) had multiple facilities in California. At least one organization in each of California’s 58 counties responded. Among the 100 responding organizations, 64% provided outpatient treatment, 37% provided residential treatment, 8% provided methadone, and 25% offered buprenorphine treatment. All respondents reported that they accepted Medicaid or county funding, 69% accepted Medicaid, 40% accepted state or county funding, and 42% accepted private insurance. Analysis of the SAMHSA Behavioral Health Treatment Services Locator data revealed that in contrast to the responding providers, 38% (N=117 facilities) of the nonresponding providers accepted Medicaid, 26% (N=80 facilities) accepted state or county funding, and 70% (N=219 facilities) accepted private insurance. Nonresponding facilities were more likely to be residential providers (55% [N=173 facilities] versus 37% of respondents), less likely to provide methadone (6% [N=18] versus 8%), and more likely to provide buprenorphine treatment (49% [N=152] versus 25%).
Stakeholder Interviews
We conducted semistructured telephone interviews from September to November 2020 with leaders (managerial and clinical) in addiction treatment organizations (referred to as “providers”) (N=12), government officials who oversee California Medicaid and public-sector addiction treatment (N=9), behavioral health telephone helpline staff (N=4), emergency department providers (N=3), and emergency medical technicians (N=2). Interviewees were identified by using networks developed by members of the study team through prior research activities. Experienced qualitative interviewers (K.T., H.P., K.H.) conducted the 30- to 45-minute telephone interviews, which were audio recorded (with consent) and transcribed. We developed an analysis matrix to abstract and organize the interview findings. Two qualitative researchers (K.T., J.T.) reviewed the abstracted data to identify common themes. Where there were discrepancies in interpretation, additional team members were consulted to achieve consensus. The study was approved by the New England Institutional Review Board.
Results
Literature Review
We identified eight studies that compared the efficacy of telehealth addiction treatment with in-person treatment (
Table 1) (
12–
19). Five studies were RCTs, and three were retrospective observational studies with a matched comparison group. Five studies involved patients with opioid use disorder, and three studies involved patients with problematic alcohol use.
Individual and group counseling.
Four studies that compared individual counseling delivered via telehealth with in-person delivery found no significant differences in treatment adherence and retention (
15,
16), excessive alcohol consumption (
16,
17,
19), drug-positive tests (
15), treatment satisfaction (
15), or therapeutic alliance (
15). Three of these studies focused on counseling of persons with problematic alcohol use (
16,
17,
19). The other study examined individual counseling for persons receiving methadone maintenance (
15). One study compared telehealth addiction group counseling with in-person group counseling for patients with partial response to methadone treatment (
14). All patients in that study received daily in-person methadone and were required to have weekly in-person individual counseling and to submit one random urine drug test per week. A higher percentage of individuals attended the telehealth group counseling, compared with in-person group counseling, although the differences did not reach statistical significance (92% versus 76%, p=0.07). No difference in drug-positive tests was noted.
Medication management.
Three studies found that telehealth can be used effectively for medication management for opioid use disorder (
12,
13,
18). In these studies, patients who received medication management via telehealth from a physician also received routine in-person treatment for drug testing and counseling and other general medical and mental health services when needed. The largest study (N=3,733) was an observational comparative study that used data from Canada (
12). Patients receiving methadone were either connected to a physician remotely from a videoconference site, usually at a clinic and under the supervision of a registered nurse, or visited the prescribing physician in person. Retention was higher among patients who had predominantly telemedicine physician visits, compared with those who had predominantly in-person physician visits.
Assessments.
We did not find any studies comparing telehealth intake assessments with in-person intake assessments.
Provider Survey and Stakeholder Interview Findings
Use of telehealth to improve access.
As an indication of telehealth’s ability to facilitate access, we asked the online survey respondents (N=100) the following question: “To what extent has telemedicine been able to mitigate the access barriers created by the stay-at-home order?” Most providers reported that telehealth mitigated access barriers almost completely (28%) or moderately (36%), whereas fewer responded “a little bit” (13%) or “not at all” (10%), and 12% responded that the question was not applicable because their patient attendance had not been affected by the pandemic. In general, the interviewed participants were enthusiastic about telehealth as a mechanism for improving access to addiction treatment. One provider said, “The unseen bonus in this [shift to telehealth] is the access to get people into treatment. That has been amazing. It just eliminated so many barriers.” Another interview participant said that because of telehealth, providers are “able to reach more people and do it more quickly and effectively.”
Use and perceived effectiveness of telehealth for various treatment services.
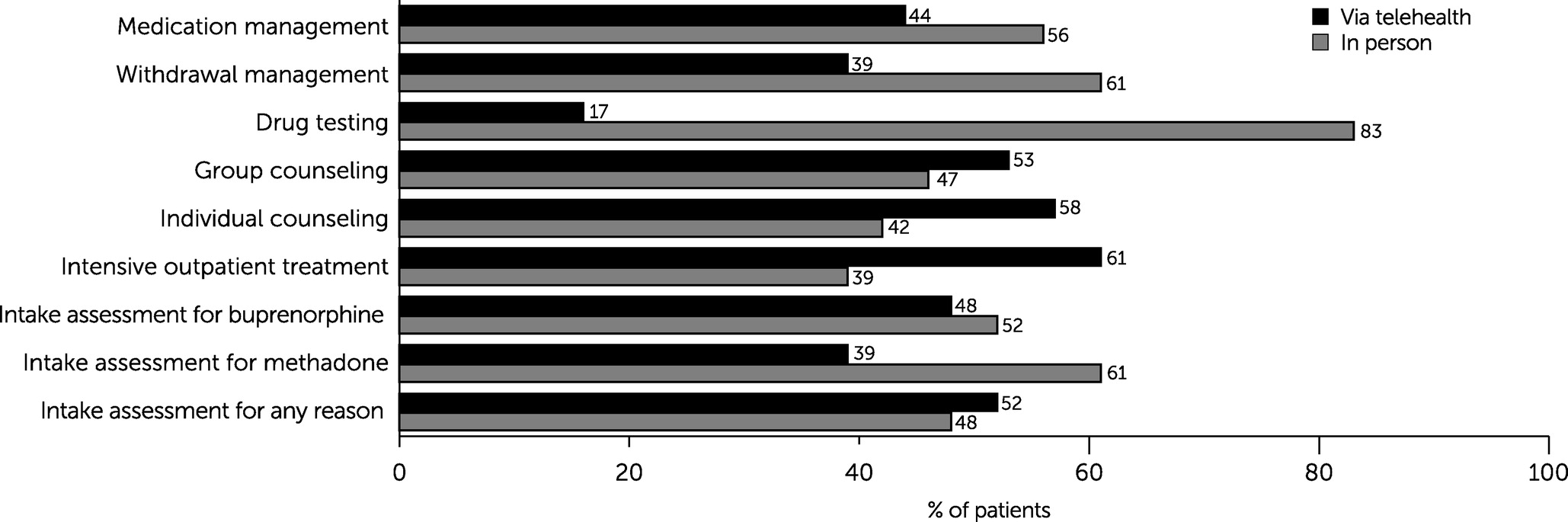
To gauge the usability of telehealth for various types of substance use disorders services, we asked the online survey respondents, “About what percentage of patients are being treated via telemedicine versus in-person?” The question was asked in regard to various addiction treatment services. The services with the largest percentage of patients being treated via telehealth were intensive outpatient (61% of patients treated via telehealth), individual counseling (58% telehealth), group counseling (52% telehealth), and intake assessment (52% telehealth) (
Figure 1). The least likely services to be delivered via telehealth were withdrawal management (39% of patients treated via telehealth), intake assessments for methadone (39% telehealth), and drug testing (17% telehealth).
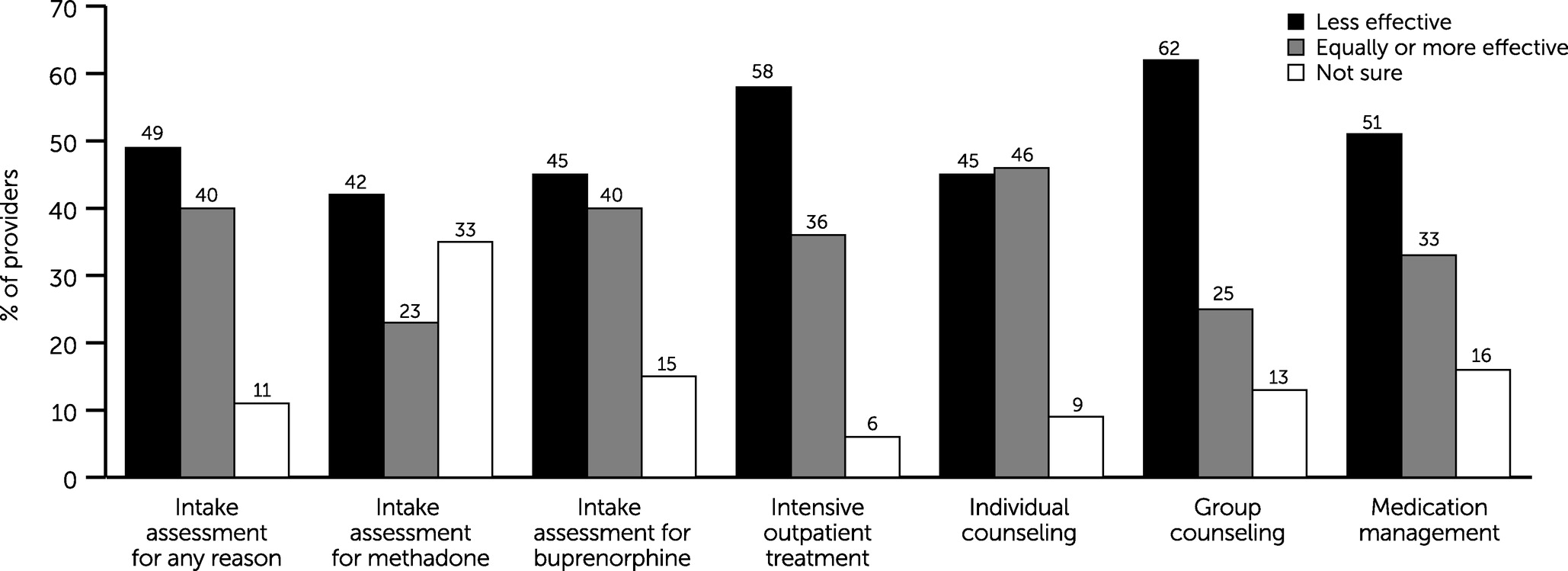
We also asked survey respondents, “How effective do you think telemedicine is relative to in-person treatment for most patients?” The question was asked in regard to various addiction treatment services (
Figure 2). For all services, except individual counseling, a larger proportion of respondents thought that in-person treatment was more effective than telehealth treatment.
Individual and group counseling.
Survey respondents were almost equally split about the relative effectiveness of in-person individual counseling (telehealth equally or more effective, 46%), compared with telehealth individual counseling (telehealth less effective, 45%) (
Figure 2). Interview participants highlighted that telehealth eliminates the transportation challenges that can prevent patients from attending counseling sessions. One county official observed that telehealth “allows access to be a little easier when people don’t have to ride a bus for two hours roundtrip to get to their appointments.” Some providers also noticed that patients were missing fewer appointments because of the convenience of telehealth. Providers also highlighted that counseling via telehealth gave them an opportunity to observe the patient’s home environment and to engage family members. One interview participant observed, “There is an intimacy of video visits that is almost like doing a home visit.”
However, providers said that it could be more difficult to sense how patients are doing in the absence of face-to-face contact. One interview participant commented, “Seeing somebody face to face, being able to see how they look, gauge their affect, and see the expressions on their face” is critical because “half of counseling and therapy is body language and visual.” Using a video format was preferable to the telephone in this respect, “If you’ve got dark circles under your eyes or you haven’t showered in a week, I’m going to be able to see that [on video], but I’m not going to be able to tell on the phone.” It can also be challenging to keep patients focused during virtual counseling sessions, especially teens and patients with attention deficit issues. To address this challenge, some providers scheduled more and shorter telehealth counseling sessions. Another concern was patient privacy. Depending on patients’ living situations, patients may not have had a place to talk where they would not be disturbed or overheard.
Of the 100 survey respondents, most (62%) reported that telehealth group counseling was less effective than in-person group counseling; only 25% reported that telehealth was equally or more effective in this context (
Figure 2). The providers said it could be challenging to keep groups engaged in a video group session. One provider noted that this challenge was especially problematic for patients with attention issues and for patients misusing methamphetamine and that sometimes patients displayed inappropriate behaviors while in groups. Some group counselors were better able than other counselors to adapt to the telehealth format and to keep group members engaged. One provider described the range of counselors’ comfort with running groups virtually: “We’ve had staff who are very good on Zoom. . . . [It is] almost like watching a game show when they go on Zoom because they’re so energetic and so on, and then some staff are just not that.”
Providers noted that telehealth may work better for some patients than for others. For example, some individuals with social anxiety may feel more comfortable participating virtually. In one provider’s experience, some patients “are a lot more open to talk about their issues” in telehealth group sessions because of “that feeling of anonymity.” However, other patients preferred in-person contact with both counselors and peers and may “feel a little more isolated.”
Many of the providers felt strongly that patients need “personal relationships and connectedness,” which are hard to establish virtually. One provider explained, “The population needs contact, they need the support of that peer group. It is one of the most effective elements of substance use disorders treatment.” Providers expressed particular concern about the appropriateness of telehealth groups for new patients. Without the initial interpersonal contact with providers and other patients, one provider noted that “they can feel a little lost in the process.” Although providers tried to recreate this support through telehealth group counseling, as one noted, “It is hard to develop a sober support network through Zoom meetings.”
Intake assessments.
Addiction treatment begins with an “intake assessment” or “history taking and evaluation” that is used to develop a treatment plan. We asked providers how effective they thought telehealth is relative to an in-person visit for intake assessment for buprenorphine, intake assessment for methadone, and intake assessment for any reason. Of the 100 survey respondents, 49% reported that telehealth intake assessment for any reason was less effective than in-person intake assessment, compared with 40% who reported that telehealth was equally or more effective in this context (
Figure 2). Interviewees noted that one advantage of telehealth intake assessments is that they can shorten the waiting time for treatment initiation. Some interview participants said that in-person intake is important because, as one noted, “an assessment is developing rapport, it’s not just data gathering.”
Medication prescribing and medication management.
For medication management, more providers surveyed (51%) thought that telehealth was less effective than in-person treatment, and 33% reported that telehealth was equally or more effective (
Figure 2). For intake assessment for methadone, 42% of respondents thought telehealth was less effective, 23% thought it was equally or more effective, and 35% were not sure. For intake assessment for buprenorphine, 45% thought it was less effective, 40% thought it was equally or more effective, and 15% were not sure. However, the interview participants highlighted that being able to start patients on buprenorphine without requiring an in-person visit “lowered the threshold to start treatment,” made it easier to “meet somebody in that moment when they are ready to start medication-assisted treatment and get them going right away,” and allowed providers to “reach people that they wouldn’t otherwise be able to reach.”
Benefits and challenges of telehealth for some patients.
Interview participants identified subsets of patients who might benefit from telehealth and those who might be more challenged by telehealth. Rural residents and patients with limited access to public transportation were identified as potentially benefiting from telehealth. Although telehealth offers potential benefits for rural patients, only about one-quarter of rural residents have broadband access (
20). Parents with young children also were identified as potentially benefiting from telehealth services, because their family responsibilities make it difficult to come to a clinic.
Telehealth was a challenge for individuals who lacked the needed technology (e.g., computers, smartphones, and Internet access) or who were not comfortable with using technology. Prior to the pandemic, most states required telehealth with videoconferencing and would not reimburse for voice-only telehealth; however, this restriction was relaxed during the public health emergency (
10). As one county official explained, “A lot of our patients don’t have reliable access either to [the] Internet or to devices with data plans that they can use to do telehealth, so telephone-based services have been really important.” Some lower-income patients obtained telephones through the federal Lifeline Assistance program, although the telephone plans came with limited monthly minutes, and some patients were reluctant to use minutes on telehealth.
Discussion
The COVID-19 pandemic caused addiction treatment providers to rapidly pivot from primarily delivering in-person addiction treatment to providing telehealth treatment. California’s experience demonstrates that it is feasible to deliver many addiction treatment services via telehealth. We were able to identify only eight studies comparing the effectiveness of addiction treatment via telehealth with that of in-person treatment. In contrast, there is a large research base on the effectiveness of telehealth for treating mental disorders. This research showed that telehealth mental health counseling is equally as effective as in-person counseling (
21–
26).
In our study, California addiction providers were most comfortable with using telehealth for one-to-one counseling. Four studies compared the effectiveness of individual counseling as part of opioid use disorder treatment or counseling for alcohol misuse (
15–
17,
19).
Providers in our study highlighted more challenges with telehealth group counseling than with telehealth individual counseling. One small study compared the effectiveness of in-person counseling with telehealth group counseling (
14).
A greater proportion of providers in our study reported that they thought medication management via telehealth was less effective than in-person medication management. The three comparative effectiveness studies that we reviewed found that medication management for opioid use disorder provided via telehealth was as effective as in-person medication management, but it should be noted that patients in these studies also received in-person services, such as visits with a clinician and drug testing (
12,
13,
18).
Although providers thought telehealth helped reduce access barriers, five studies did not find that telehealth resulted in improved treatment retention, but they may have been underpowered (
13–
16,
18). One large Canadian observational study found improved retention with telehealth-delivered methadone medication management (
12).
Providers in our study noted that the relative benefit of telehealth depended on a client’s circumstances and stage of treatment. New patients, patients who are homeless, patients who are isolated, patients who are not comfortable using technology, patients with attention challenges, and patients without private spaces to talk may be better suited to in-person treatment. Conversely, patients with young children, patients who find it difficult to take time off and travel to appointments, and patients who prefer meeting online may benefit from telehealth treatment. There also may be times during treatment when the ability to observe the patient in person to better monitor symptoms and build rapport outweighs the convenience of remote treatment. These factors point to the benefits of a hybrid approach comprising both telehealth and in-person addiction treatment.
This study had some limitations. We collected data only in California, and the stakeholder interviews involved a convenience sample. Although we believe that the findings are generalizable to other states, this should be confirmed. We did not examine the benefits and limitations of telehealth by speaking with patients or payers. For example, payers have justified telehealth restrictions as necessary to prevent fraud, and we did not examine this issue. In terms of the literature review, we did not conduct a formal meta-analysis that accounted for the quality of the research. Some of the studies had small samples and may have been underpowered to detect a difference between telehealth and in-person treatment.
Conclusions
The widespread and rapid adoption of telehealth for substance use disorder treatment services under the COVID-19 pandemic emergency order invigorated a reassessment of telehealth’s role in addiction treatment. More research is needed on the effectiveness of telehealth-delivered addiction treatment. Telehealth may serve to improve addiction treatment access, initiation, and retention. However, to date, only one study of telehealth-delivered addiction treatment has shown that benefit.