Although individuals with mental illness are overall more likely than the general population to be victims of violence (
1), meta-analysis data show that nearly 20% of patients with mental illness may commit an act of violence while admitted to a psychiatric hospital (
2). Two-thirds of staff in one psychiatric hospital reported experiencing at least one physical assault in the past year (
3), and 50% of psychiatric nurses have reported experiencing physical violence at work (
4). These acts of violence detract from the therapeutic nature of the clinical milieu and increase rates of staff burnout and turnover (
1,
5). In some instances, when psychiatric providers are the target of violence, they may choose to file a complaint with law enforcement, which can lead to criminal charges against the patient.
The first case of a therapist filing criminal charges against a patient was published in 1978 (
6). Since that time, further efforts have been made to examine the ethical considerations of filing police reports on psychiatric patients for behaviors that occur on inpatient units (
7–
11). Acts of violence are not limited to psychiatric units (
12); however, the potential impact of mental illness on behavior may amplify the complexity of these legal decisions.
Advocates for filing charges against patients suggest that police involvement may be appropriate for willful criminal acts unrelated to an individual’s mental health. Legal repercussions may also deter future violence by imposing carceral and noncarceral consequences. Yet, in practice, clinicians may be hesitant to contact law enforcement because legal authorities may decide not to press charges or prosecute the person, rendering the police report both ineffective and potentially damaging to the patient-clinician relationship. Beyond that, providers may find themselves torn between a duty to act in the best interest of the patient and a duty to their employer or the legal system.
Because of these complexities, some scholars have suggested limiting the criminal prosecution of psychiatric inpatients to specific circumstances (
8,
9), including deliberate criminal behavior unrelated to psychiatric illness, instances of severe violence, and instances in which concrete consequences may motivate behavior change. Previous policies have suggested that when determining whether to file charges with law enforcement, the clinical team should consult a third party not directly involved in treatment to provide objectivity (
7).
Few studies have quantitatively examined the impact of current policies or practices surrounding legal charges for psychiatric inpatients. Kumar et al. (
13) reported on 31 assaults, of which three resulted in police involvement. Hoge and Gutheil (
14) reported nine cases in which patients received legal charges after an assault. The latter authors concluded that prosecution could positively influence some patients through deterrence and negatively affect others by alienating them from the mental health system.
In this study, we examined a sample of psychiatric inpatients who assaulted staff. We sought to determine whether patients whose assault resulted in the filing of a police report differed in certain characteristics from those whose assault did not result in a report.
Methods
Study Population
This retrospective cohort study was conducted at a 119-bed inpatient psychiatric hospital located in an urban academic medical center in the northeastern United States. The study population included patients from five specialized psychiatric units serving adolescents (ages 14–17 years), transition-age youths (ages 18–26), patients with a mood disorder (ages ≥26), general adults (ages ≥26), and geriatric patients (ages ≥56). Data were collected between November 1, 2016, and July 1, 2019. There were 9,654 admissions, and the average length of stay was 11.9 days. Of the primary psychiatric diagnoses, 58.0% (N=5,597) were mood disorders, 25.6% (N=2,470) schizophrenia or psychotic disorders, 7.0% (N=680) anxiety or adjustment disorders, 4.2% (N=409) substance use disorders, and 3.4% (N=331) other mental disorders.
As of December 2020, no written guidelines existed about when and how staff should file charges with law enforcement after an assault by a patient. In practice, individual staff members informed hospital security of their desire to file a police report immediately after an assault, and security then notified local law enforcement. This was only the first step in the legal process and was followed by the decision made by law enforcement to formally file charges, the state’s decision to prosecute a particular crime, and, ultimately, a judicial determination regarding sentencing in the event of a conviction. This study protocol was approved by the institutional review board of Yale University.
Data Collection
Data were gathered through an electronic event-reporting system used to monitor self-reported safety events across the institution (RL Solutions). Nursing staff were trained to report incidents of physical and sexual assault according to the National Database of Nursing Quality Indicators (
15). Incidents were reviewed and linked with hospital encounters in the electronic medical record. Demographic and operational data were collected, including gender, age, race-ethnicity, and hospital unit. Clinical data were extracted and included primary psychiatric diagnoses, secondary psychiatric problems, admission urine toxicology results, as-needed intramuscular antipsychotic use, as-needed oral medication use (antipsychotic, anxiolytic, or antihistamine), and criminal history. Additional details were collected during routine follow-up, including assault victim type (patient, staff, or other) and assault level of injury (no, minor, moderate, or major injury) (
15). To collect data on criminal charges, a chart review was performed on each instance of assault by using five key phrases: “charge,” “NHPD” (for New Haven Police Department), “police,” “criminal charge,” and “assault.”
Assault instances targeting nonstaff members were excluded (N=105, 46% of all assaults). This exclusion enabled us to focus on elucidating when mental health providers pursue legal recourse for violence against staff on the inpatient unit. Diagnostically, we identified a group of patients who were diagnosed as having schizophrenia, schizoaffective disorder, or a mood disorder with psychotic features and labeled this group as having chronic mental illness with psychosis. A different diagnostic group was used to capture psychosis that was not clearly due to a chronic mental illness, such as psychosis unspecified. This distinction helped to create a group of individuals who had a cross-sectional, inpatient presentation of psychosis that was linked to a known chronic condition and separated these individuals from those who may have had psychotic symptoms with a less defined illness. Those who were diagnosed as having any substance use disorder (excluding nicotine use disorder) were grouped as patients with substance use disorders. Patients who had a diagnosis of antisocial, borderline, and unspecified personality disorder were grouped as having personality disorder. These diagnoses were grouped according to the first four chart diagnoses so that patients could be part of multiple diagnostic groups.
Data Analysis
Data management and statistical analysis were performed with Stata/IC v16. Continuous variables are presented as mean±SD. Categorical variables are presented as the number (proportion or percentage) of participants. We estimated p values for continuous variables with two-sample t tests (for comparison of means between groups). For categorical variables, p values were calculated with Pearson's chi-square tests. Multivariate logistic regression models were used to factor in demographic characteristics, comorbid conditions, and injury data to estimate the odds of the outcome of receiving criminal charges from assault to staff members. Effect-modification analysis was used to examine the relationship between patients’ age and the hospital unit where patients were admitted because units were organized largely by age.
Results
In total, 124 instances of assaults of patients on staff were included in this study, 27 (22%) of which resulted in staff filing charges with law enforcement.
Table 1 shows the characteristics of the patients involved in the assaults, stratified into two groups by whether staff wished to file charges with the police after an assault. The mean age±SD in the total sample was 32.9± 21.1 years, and 48% were female. Overall, 42% identified as non-Hispanic White, 33% as non-Hispanic Black, 10% as Hispanic, and 14% as “other.”
Table 2 shows multivariate logistic regression results, where the outcome for this analysis was the odds of staff members pursuing charges for assault. Compared with patients without criminal history, those with criminal history had 2.2 times higher odds of staff filing charges (95% CI=1.26–3.78, p=0.006). Patients diagnosed as having a chronic mental illness with psychosis had higher odds of staff filing charges compared with patients without these diagnoses (OR=7.23, 95% CI=1.49–35.04, p=0.01). Last, younger patients were more likely to have a police report filed than older patients (OR=0.92, 95% CI=0.91–0.94, p<0.001). The odds of staff pursuing charges based on patient race or sex were not statistically significant.
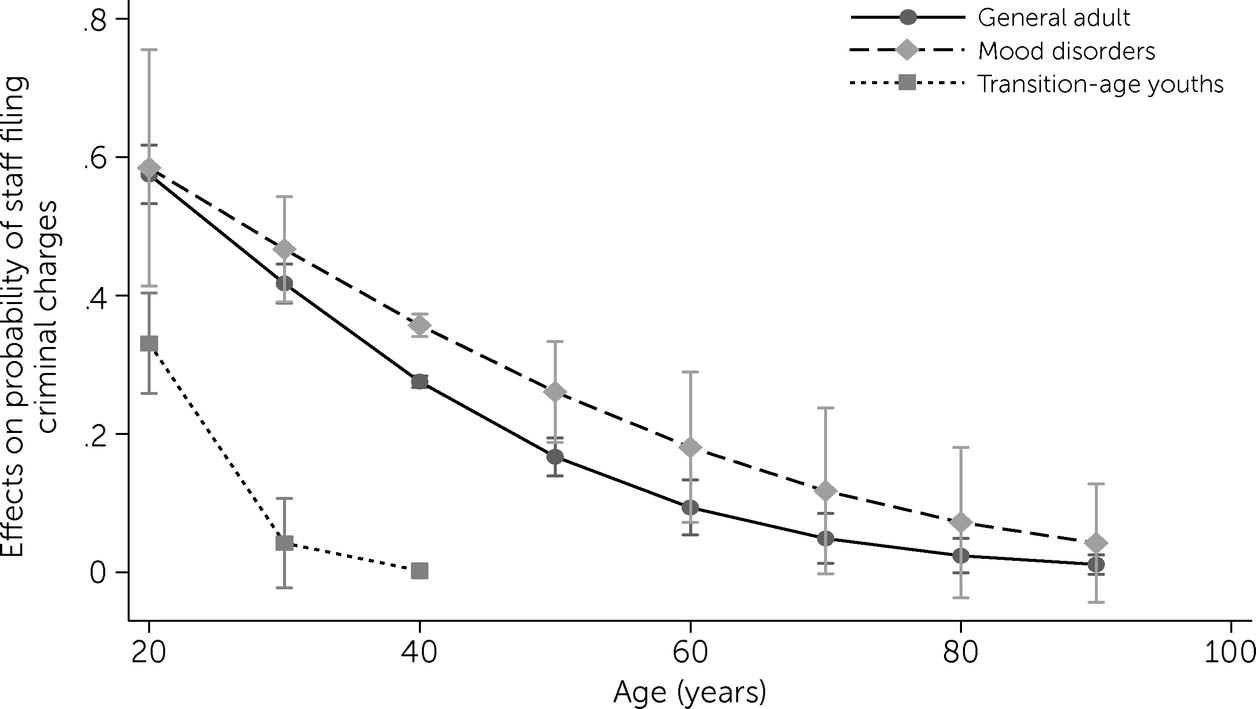
Effect-modification analysis revealed an interaction between age and the hospital unit where patients were admitted. A statistically significant interaction was found that modified the odds ratio for age on the mood disorders unit. Older patient age was related to a reduced probability of staff wishing to file charges; however, this effect was significantly weaker for patients admitted to the mood disorder unit, as shown in
Figure 1.
Discussion
Over approximately 3 years, our large hospital system had 124 admissions that resulted in assaults on staff on inpatient psychiatric units. In 22% of these instances, staff filed a police report and pursued criminal charges. When we examined differences in demographic and clinical characteristics between the group of patients whose assault led to a police report and those whose assault did not, we observed significant effects of criminal history, age, and diagnosis of a chronic mental illness with psychosis on the likelihood of charges being filed against assaultive patients. A variety of other variables did not show a significant effect on the filing of criminal charges, including race, gender, number of instances of restraint use, and number of as-needed medications. On the basis of the differences we examined in these groups, we used predictive models, finding that assaults that resulted in minor injury, which was the most commonly identified level of injury, were predictive of staff pursuing charges. In addition, the model identified three patient-level variables, discussed below, that predicted which patients were more likely to have charges filed against them.
Criminal History
The presence of a criminal history increased the likelihood that staff would pursue charges. One possible explanation for this finding is that previous legal involvement may signal to staff that a patient is predisposed to volitional antisocial behaviors. Previous legal involvement may bias staff toward believing that a patient’s behavior should be managed by the judicial system rather than a hospital. They may also be less hesitant to file charges against someone who already has experience in the legal system.
It is notable that in one-third (N=9) of cases where staff pursued filing criminal charges, the patients had no known criminal history. This observation suggests that although the absence of a criminal history may mitigate the risk for staff filing criminal charges, it does not eliminate it. Assaultive behavior on inpatient units is one potential, albeit small, entry point through which individuals with mental illness may enter the criminal justice system.
Chronic Mental Illness With Psychosis
Patients experiencing psychosis are at times detached from reality and may be perceived as having less volitional control over their actions (
16). It may be expected that patients charged for their violent behavior would be more likely to be diagnosed as having character pathology rather than chronic mental illness with psychosis as reported in the study by Hoge and Gutheil (
14).
However, in our sample, individuals diagnosed as having chronic mental illness with psychosis were more likely to experience legal charges for assaultive behavior. This observation suggests that a detachment from reality did not protect against staff filing charges. This finding was true even for a group that excluded patients with unspecified psychosis and focused on those with known chronic illnesses. The presence of a co-occurring substance use disorder or personality disorder did not contribute to the difference in likelihood of filing charges. Notably, only two patients in this study had a chart diagnosis of a personality disorder, which limited our ability to evaluate the impact of this comorbid condition on the filing of charges.
Further, victims, particularly nonclinical staff, may not always be privy to patients’ diagnoses, and staff’s desire to contact law enforcement may be in response to their affective arousal in the immediate aftermath of an assault. Thus, the victim may not consider the impact of the illness on an assaultive patient’s behavior. Victims have a right to pursue charges as independent citizens, and the severity of certain crimes (e.g., rape and severe injury) may outweigh other considerations. However, given the unique medical-ethical considerations for a member of the health care system filing charges against a patient, it may be beneficial to provide third-party consultation to victimized staff. This third party can provide a more objective perspective, create an opportunity for staff to consider the impact of illness on a patient’s behavior, and allow some time to pass to prevent staff from reflexively pressing charges in the heat of the moment. This is only one possible mitigating strategy because ultimate prosecutorial authority lies outside the hospital, and staff are not ultimately responsible for determining whether a criminal act is caused by a mental illness. Legal processes exist to investigate a defendant’s state of mind at the time of the assault and subsequent culpability should prosecution proceed.
Age
In this study, staff were more likely to pursue criminal charges when assaulted by younger patients. This finding is complicated by the fact that the units in this hospital system were largely divided by patient age. Our analysis suggests that regardless of the environment, staff tended to bring charges against younger patients more frequently. However, the magnitude of the impact of age was modified by the unit. Specifically, age had less impact on the filing of charges against assaultive patients treated in the mood disorders unit, which may suggest that the relationship with patient age is affected by diagnosis or other unit-specific factors. The small sample size in this study limited the drawing of further conclusions from the effect-modification analysis.
One potential contributor to this finding may be the perception that younger patients are more dangerous than older patients because younger individuals tend to be more physically fit (
17,
18). However, as seen in
Figure 1, an interaction between clinical unit type and age suggests that unit-specific factors are contributing to staffs’ decision to file charges. Further studies will be needed to explore the interaction between age and unit-specific milieu to better understand how this interaction determines assaultive patients’ treatment trajectories.
Limitations
The retrospective design of this study relied on documentation by team members to identify when criminal charges were filed. We used a wide range of key words and individual chart review to better understand the series of events that occurred after an inpatient assault. However, we may have underestimated the number of charges filed either because of an error in our search processes or because of a lack of chart documentation.
Because of limitations in the available data, the characteristics of staff members were not available. Staff members’ age, race, gender, and job title may influence their decision about filing charges. Staffs’ level of experience and perception about violence in the workplace are also important factors to consider and would benefit from future qualitative study (
19). Such further study may also shed light on the impact of informal conversations between law enforcement and hospital staff. The perception of follow-through and law enforcement attitudes may influence the victim’s behavior in a given location but was not examined in this study.
Although this report of psychiatric patients with legal involvement after assaults on staff is the largest to our knowledge, it still had a sample size that was relatively small for using multivariate statistics to explore a complex outcome. We were limited in our ability to sufficiently power analyses to explore additional variables that may influence staffs’ decision to pursue charges with law enforcement. For example, gender, race, and use of as-needed medications or restraints did not appear to be different between the two groups in this study, but this lack of a significant difference may also have been a result of the small sample size and should be explored in future studies.
The small number of patients diagnosed as having a personality disorder was also a limitation. Although the limited sample size may be explained by the lack of reimbursement incentives and the cross-sectional nature of inpatient hospitalization, it limited our ability to draw conclusions because it likely underrepresented the true number of patients with personality disorders. Future prospective studies may be able to identify personality pathology more accurately to further our understanding of their impact on law enforcement involvement after staff assault.
Implications and Future Directions
In this study, younger age, chronic mental illness with psychosis, and a known criminal history of an assaultive patient were associated with a higher likelihood of staff pursuing charges with law enforcement after the assault. Larger studies are needed to examine whether these findings are generalizable to other institutions and whether additional variables may contribute to a patient’s risk for facing legal involvement after an assault. Future studies may also benefit from qualitatively examining the perceptions and attitudes of law enforcement and staff who are victimized to better ascertain how these perceptions influence their decision about whether to pursue criminal charges.
This study examined only the first step in the legal process, health care workers’ decisions whether to pursue charges. Insufficient data were available to examine the remainder of the legal process. It is unclear how each of the 27 charges filed were adjudicated and whether they were even prosecuted. We hope that future studies can follow these processes longitudinally to better understand the impact of criminal justice involvement on patients charged for assaultive behavior during psychiatric admission.
Conclusions
To our knowledge, this study offers the largest known analysis of patient characteristics that appear to predict staffs’ decision to contact law enforcement after being assaulted by a patient at one institution—these patient characteristics included younger age, a criminal history, and presence of a chronic mental illness with psychosis. It is important to remember that all psychiatric staff have a right to pursue charges after an assault. However, criminal justice involvement can have long-lasting impacts and should be considered carefully.
We contend that institutions should create a review process for patients’ assaults on staff. Ideally, this review would include three key components. First, a third party would be made available to provide time for staff to distance themselves from the heat of the moment to gain objectivity and to educate them on the steps of the potential legal process. Second, consultation would be offered to the clinical team about ways to optimize clinical care and prevent further acts of violence. The U.S. Department of Veterans Affairs Disruptive Behavior Committee is one example of how behavioral disruptions can be managed by noncarceral interventions (such as medical record flags to increase awareness, limitations on where patients and staff can interact, specific levels of observation, and others) recommended by a committee of stakeholders (
20). Third, such a process would include systematic data collection on these types of assaults and periodic review of outcomes to monitor for potential trends, including changes in the rates of assaults or reports to law enforcement and systemic bias on the basis of race, gender, or socioeconomic status.