Working in the field of mental health can be emotionally taxing, particularly in community mental health service settings, which are often underresourced, with high demands and few support services to assist staff and clients (
1). People working in mental health are susceptible to client-related burnout (i.e., physical and psychological exhaustion when working with clients) (
2). Although numerous factors are associated with client-related burnout, such as inadequate supervision (
3) and severity of clients’ mental illness (
4), recent evidence demonstrates that perceptions that clients are not improving also contribute to client-related burnout (
5). Given the emotional labor involved in the provision of mental health services, particularly in an underresourced environment, it is no surprise that mental health workers can experience burnout if they perceive that their counseling is not improving their clients’ lives.
Client-related burnout is associated with negative job attitudes, lower job engagement, poorer workplace well-being, and increased intentions to resign (
6,
7). Burnout among health care workers may also result in poorer outcomes for clients, including decreased satisfaction with treatment and lower reported quality of care (
8,
9), and may be more common in settings where client progress is slow and uneven (
10). Because the recovery trajectories for clients dealing with mental health issues is variable and can depend on the severity of their mental health issue and the support available to them (
6), it is important to consider factors that might buffer mental health staff from client-related burnout associated with perceptions of limited client progress.
Lived experience with mental illness, which refers to people who have personal experience of mental health challenges and who have used mental health services themselves (
11), may play a role in this process. Research has increasingly recognized the importance of peer workers in mental health and drug and alcohol treatment settings (
12–
14), but few studies have focused specifically on the benefits of lived experience among health care staff in relation to workplace outcomes. Although the literature does not always make clear distinctions, individuals who identify as peer support workers are generally employed in a role that specifically incorporates their work as peers, whereas staff with lived experience are employed first and foremost as health care providers, who may or may not choose to share their history of mental health issues or use it to inform their work with clients (
15). This unofficial, yet valuable, source of expertise among those with lived experience is not always acknowledged in clinical services or research (
16). Yet staff with lived experience of mental health issues have first-hand experience with their own recovery challenges, as well as with the difficulties in navigating the mental health care environment as consumers. As a consequence, staff with lived experience may be less susceptible to client-related burnout caused by feelings that their help has resulted in little client progress, because they understand that recovery can be slow and uneven.
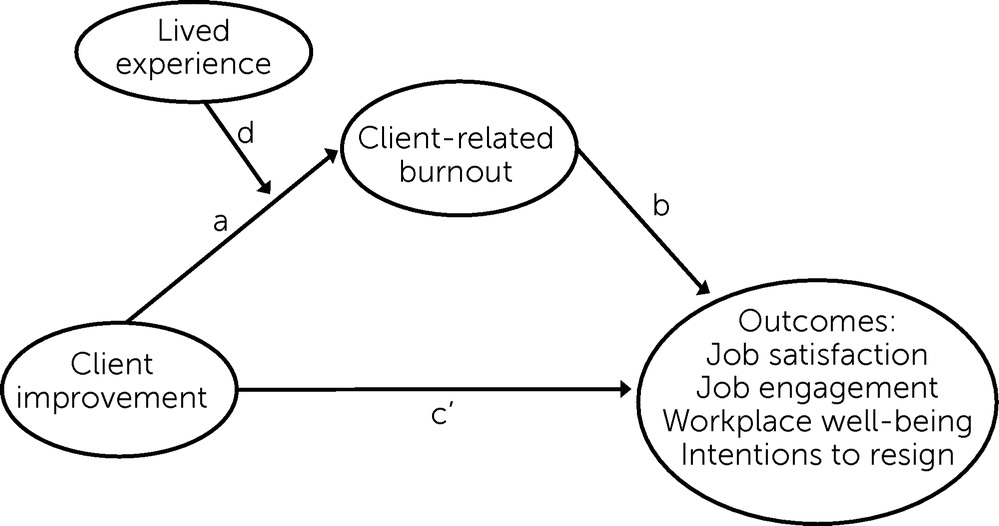
Therefore, we hypothesized that perceptions that clients are not improving should lead to client-related burnout but that this relationship should be weaker or nonexistent among mental health workers with lived experience. Consistent with previous research (
5), client-related burnout should play a mediating role between mental health workers’ perceptions that their clients are not improving and their subsequent job satisfaction, engagement, workplace well-being, and intentions to resign. This mediated relationship, in turn, should be moderated by lived experience (
Figure 1).
Methods
Participants and Procedure
Participants were employees of a community mental health service organization in Australia who provide direct support to the people accessing their services. Although a diagnosis is not necessary to access support from this organization, its stated mission is to provide services to people who are experiencing severe and persistent mental illness. The participating community mental health organization sent its employees an e-mail containing a weblink to the survey. Employees who clicked on the link were provided information about the study before deciding to continue. Employees were eligible for participation if they indicated that they were over age 18 and provided direct support to the people who access their services. The survey was launched on October 28, 2020, and was open for 3 weeks.
The scales in the survey were presented in a randomized order, with the exception of the demographic questions, which were always at the end of the survey. At the completion of the survey, participants could provide their e-mail address to be included in a prize draw. E-mail addresses were collected in a separate spreadsheet file so that they could not be linked to survey responses. Six respondents were randomly selected to receive a $50AUD gift voucher. The study was approved by the University of New South Wales Ethics Committee (HC200473) and conformed to the ethical standards set out in the 1964 Declaration of Helsinki.
Measures
Client-related burnout was assessed with the six-item subscale from the Copenhagen Burnout Inventory (Cronbach’s α=0.82) (
2). The items are designed to tap feelings of physical and psychological exhaustion from working with clients. A sample item is “Does it drain your energy to work with the people who access your services?” Responses are provided on a 5-point scale ranging from never to always, with higher numbers indicating greater client-related burnout.
Job satisfaction was assessed with Brayfield and Rothe’s (
17) job satisfaction scale (Cronbach’s α=0.82). A sample item is “Most days I am enthusiastic about my work.” Responses are provided on a 5-point scale (1, strongly disagree, to 5, strongly agree), with higher numbers indicating greater job satisfaction.
Job engagement was assessed with nine items from Rich and colleagues’ (
18) Job Engagement Scale (Cronbach’s α=0.90). Sample items include the following: “I devote a lot of energy to my job”; “At work, I am absorbed by my job.” Responses are provided on a 5-point scale ranging from strongly disagree to strongly agree, with higher numbers indicating greater job engagement.
Intentions to resign from the organization and from the profession were assessed with Boroff and Lewin’s (
19) two-item scale. Samples from each scale are “I am seriously considering quitting this job for an alternative employer,” and “I am seriously considering quitting the mental health profession.” Both scales showed good reliability (for intentions to quit the organization, r=0.89; for intentions to quit the profession, r=0.80). Responses are provided on a 5-point scale ranging from strongly disagree to strongly agree, with higher numbers indicating greater intentions to resign.
Workplace well-being was assessed with Warr’s (
20) 12-item scale (Cronbach’s α=0.93). Participants read, “Thinking of the past two weeks, how much of the time has your job made you feel each of the following,” which is followed by adjectives such as tense, depressed, optimistic, and enthusiastic. Responses are provided on a 6-point scale ranging from 1, never, to 6, all of the time. Items are reverse-coded as necessary, such that higher numbers indicate better workplace well-being.
Employees responded to two items designed to tap the degree to which they perceive their clients to be improving from treatment (“The support I provide enables the people who access our services to live better lives,” and “The support I provide improves the lives of the people who access our services”; r=0.91). Participants responded by using a 5-point scale (1, strongly disagree, to 5, strongly agree), with higher numbers indicating greater perceived improvement among their clients.
At the completion of the survey, participants indicated their age, gender, tenure working in the mental health sector and in the organization, and their role in the workplace. Finally, participants were asked, “Do you identify as someone who has lived experience with mental health issues?” (yes or no). Participants who responded yes received a follow-up question asking, “Over the course of your life, how much has your personal experience of mental health issues affected your life?” Respondents answered on a scale ranging from 0, not at all, to 10, greatly affected.
Analysis Plan
Moderated mediated regression analyses were conducted using SPSS, version 26, and model 7 of the PROCESS macro (
21). The basic goal of moderated mediation is to test the influence of a moderator variable (i.e., lived experience) on a proposed mediated relationship (i.e., beliefs that clients are not improving leads to burnout, and greater burnout leads to more negative workplace outcomes). This causal chain (lack of client improvement to burnout to workplace outcomes) was predicted to differ between staff with and without lived experience: moderated mediation. Our moderated mediation analyses tested whether lived experience buffers staff from the burnout experienced when they perceive that their clients are not improving from treatment and also tested whether client-related burnout plays a mediating role between mental health workers’ perceptions that their clients are not improving and their subsequent job satisfaction, engagement, workplace well-being, and intentions to resign (
Figure 1).
Results
Preliminary Analyses
The sample comprised 179 employees (45 men, 131 women, one nonbinary individual, and two who preferred not to say) who completed the online survey, a response rate of approximately 23%. With regard to age, 39 participants were under age 30, 50 were ages 30 to 39, 33 were ages 40 to 49, 45 were ages 50 to 59, and 12 were age 60 or older. The mean±SD number of years that respondents had worked in the mental health field was 5.92±5.99 (range 1 month to 37 years). Respondents’ average tenure working for their current employer was 3.65±3.51 years (range 1 month to 18 years).
Among the 179 respondents, 112 identified as having lived experience with mental health issues, and 67 did not. Lived experience did not differ as a function of education level. On average, participants with lived experience indicated that their mental health issues had affected their lives in meaningful ways (mean±SD score=7.13±1.99, on a scale ranging from 0, not at all, to 10, greatly affected).
On average, respondents felt that their clients were improving from treatment (
Table 1), although there was considerable variability in this belief, with responses ranging across the full scale. Perceptions of client improvement were unrelated to the demographic variables. Specifically, no differences were noted in ratings of client improvement between staff with and without lived experience (mean±SD=4.40±0.77 versus 4.32±0.70). The relationship between tenure and perceptions of client improvement was not significant, suggesting that beliefs about client improvement were not affected by how long someone had worked at the organization (r=0.09, p=0.234) or in the mental health field (r=0.071, p=0.344). Degree of burnout also did not vary as a function of lived experience (r=–0.11, p=0.153).
Table 1 presents the means, standard deviations, and intercorrelations between the study variables. To the degree that staff perceived their clients were not improving from treatment, they reported lower job satisfaction, poorer workplace well-being, greater intentions to quit the organization and profession, and higher client-related burnout.
Moderated Mediation Analyses
Model 7 of the PROCESS macro (
21) with 5,000 bootstrapped resamples was used to test the model presented in
Figure 1. The results of this model are presented in
Table 2. Perceptions that clients were not improving were associated with more burnout (
Table 2, column a). Importantly, as can be seen in column d, the relationship between client improvement and burnout (
Figure 1, path a) was moderated by lived experience (
Figure 1, path d). This interaction was decomposed by examining the relationship between client improvement and burnout separately for staff with and without lived experience. These follow-up analyses revealed that the relationship between client improvement and client-related burnout was significantly weaker among staff with lived experience (b=0.175, p=0.017), suggesting that they were less susceptible to the burnout caused by perceptions that clients were not improving, compared with those without lived experience (b=0.591, p<0.001). In summary, when staff believed that their clients were not improving, staff with lived experience reported lower burnout, compared with staff without lived experience.
We also examined whether beliefs that clients are not improving influenced workplace outcomes directly (path c′) and indirectly through burnout (column a*b). That is, does client-related burnout mediate the relationship between perceived lack of client improvement and workplace outcomes, and, importantly, does this mediated relationship differ as a function of lived experience? Results indicated that the mediated relationship between client improvement and the outcome variables via client-related burnout differed significantly as a function of lived experience for all the outcome variables (
Table 2, column d). Nonetheless, the pattern of these moderated mediated relationships was not uniform across the outcome variables. Among staff with lived experience, burnout was associated with poorer workplace well-being and increased intentions to quit the job and profession. As can be seen in
Table 2, burnout was not associated with these workplace outcomes among staff without lived experience. In contrast, burnout was associated with lower job satisfaction and job engagement for both groups of staff.
Finally, we compared the hypothesized model depicted in
Figure 1 to all other viable competing models to assess whether the causal direction we propose better fits the data than do alternative causal models. For example, we examined whether more negative organizational outcomes (i.e., job satisfaction, job engagement, workplace well-being, and intentions to quit) might lead employees to experience client-related burnout, which in turn affects perceptions of client improvement. Across the 12 alternative models, only job engagement showed significant moderated mediation (further details are provided in an
online supplement to this article). Thus these additional analyses suggest that none of the alternative models fit the data as well as did the hypothesized model.
Discussion
Given the emotional demands of working in community mental health, staff being susceptible to client-related burnout is not surprising. Building on previous research demonstrating that perceptions that clients are not improving are associated with client-related burnout (
5), we found that lived experience of mental health issues buffered health care workers against client-related burnout. Health care workers with lived experience also reported more positive job attitudes, compared with those without lived experience.
In light of the buffering role that lived experience appeared to play in reducing burnout associated with perceptions that clients were not improving, future research should uncover why lived experience is beneficial. For example, do staff with lived experience differ in their recovery beliefs, compared with staff without lived experience? Lived experience provides staff with first-hand knowledge about the path to recovery, and thus they may be more likely to recognize the nonlinear path that recovery can take (
22). If differences in recovery beliefs help explain the buffering role of lived experience, interventions outlining the nonlinearity of recovery may help reduce burnout that is caused by feeling unable to help clients. Alternatively (or additionally), having dealt with the challenges of recovery personally, staff with lived experience may be more empathic toward their clients, and this increased empathy may make them less susceptible to client-related burnout when they perceive that their clients are not improving. Uncovering the mechanisms by which lived experience buffers staff from client-related burnout can aid the development of interventions to boost resilience and ultimately workplace longevity among mental health employees.
Although not directly relevant to our findings, future research might also examine whether (and when) staff with lived experience disclose this information to their clients and if so, whether this disclosure is beneficial. Research suggests that lived experience can inform how mental health workers engage with and understand clients and can increase credibility and rapport with them (
23,
24). Having successfully navigated the challenges of their own mental health, employees with lived experience may be examples to clients that successful recovery can be achieved over time. Additionally, workers with lived experience may have a more deep-seated optimism in their clients’ long-term prognosis, which may ultimately enhance their clients’ recovery. Future research should explore whether client outcomes vary as a function of whether their mental health providers have lived experience.
As with any research, limitations should be considered when interpreting the findings. First, because of the cross-sectional design, causality is unclear. For example, health care workers who had more negative job attitudes may simply have been less likely to recognize improvement in their clients. This possibility seems unlikely, however, because mental health staff with lived experience had more positive job attitudes, yet their perceptions of client improvement did not differ from those of staff without lived experience. Nonetheless, reverse causal models were run to determine whether any models fit the data better than the proposed model. The results demonstrated that alternative models were statistically less plausible, but experimental or longitudinal research is necessary to address concerns about causality.
Second, because of our exclusive reliance on self-report measures, the results are susceptible to problems of common method variance, which can inflate interrelationships between variables. To address this concern, we followed recommendations to create methodological separation (
25). For example, predictor, moderator, and mediator variables were all assessed on different response scales. We also presented the different types of measures on separate survey pages. Finally, the amount of identifiable information collected was minimized to reduce common method variance that can arise from social desirability concerns (
25). Despite these proactive steps, future research should use a multimethod approach where possible. For example, a longitudinal design incorporating more objective measures of client improvement would eliminate concerns about the causal direction of the proposed model and common method variance.
Third, the number of health workers in this sample who reported a history of lived experience of mental health issues was almost double the number who reported no lived experience. This discrepancy may be a by-product of self-selection into the survey (particularly in the context of a 23% response rate), but a history of mental health issues appears to draw people to work in the mental health sector (
26). Thus, although it is unclear how representative these samples of individuals with and without lived experience are of the field of community mental health, the pattern of relationships appears to be robust. Finally, although not a limitation per se, the finding that client-related burnout was not consistently associated with more negative workplace outcomes among employees without lived experience was unexpected. We have no explanation for this uneven pattern of results, but we suggest that it is worth reexamining in future research.
Conclusions
This study provided evidence that long-term efforts to assist clients, coupled with feelings that only limited progress is being made, were associated with client-related burnout. Nonetheless, this relationship was weaker among staff who identified as having lived experience, demonstrating a previously undocumented benefit of lived experience. Given the high rates of burnout in the mental health profession, future research should explore why lived experience protects staff from client-related burnout. This information can aid in the development of interventions to boost worker resilience, engagement, and longevity in the field.
Acknowledgments
The authors are grateful to the community mental health organization for its participation in this research. They also thank members of the Community Research Advisory Committee for their advice on the project.