Differences Between VHA-Delivered and VHA-Purchased Behavioral Health Care in Service and Patient Characteristics
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Methods
Study Design
Data Sources
Measures
Outcome variables.
Inpatient behavioral health stays.
Outpatient behavioral health use.
Provider training.
Behavioral health severity and comorbid conditions.
Sociodemographic and access characteristics.
Data Analysis
Results
Behavioral Heath Inpatient and Outpatient Cohort Characteristics
| Only VHA care (N=148,284) | Any community care (N=55,810) | |||||
|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | Standardized mean difference | p |
| Veteran behavioral health condition group | .25 | <.001 | ||||
| Serious mental illness | 47,037 | 31.7 | 21,781 | 39.0 | ||
| Substance use disorders | 41,759 | 28.2 | 16,263 | 29.1 | ||
| Posttraumatic stress disorder | 13,059 | 8.8 | 3,115 | 5.6 | ||
| Personality disorders | 1,332 | .9 | 170 | .3 | ||
| Mood disorders | 38,852 | 26.2 | 13,237 | 23.7 | ||
| Anxiety disorders | 2,998 | 2.0 | 399 | .7 | ||
| Other behavioral health disorders | 3,247 | 2.2 | 845 | 1.5 | ||
| Gagne physical health score (M±SD)a | 1.26±2.14 | 1.21±1.98 | −.02 | <.001 | ||
| Veteran characteristic | ||||||
| Age (M±SD) | 51.45±14.89 | 49.97±14.34 | −.10 | <.001 | ||
| Sex | .06 | <.001 | ||||
| Male | 132,261 | 89.2 | 48,697 | 87.3 | ||
| Female | 16,023 | 10.8 | 7,106 | 12.7 | ||
| Missing | 0 | — | 7 | .0 | ||
| Race | .02 | <.001 | ||||
| American Indian or Alaska Native | 1,533 | 1.0 | 649 | 1.2 | ||
| Asian | 1,151 | .8 | 410 | .7 | ||
| Black or African American | 37,633 | 25.4 | 13,637 | 24.4 | ||
| Native Hawaiian or other Pacific Islander | 1,135 | .8 | 485 | .9 | ||
| White | 99,563 | 67.1 | 37,789 | 67.7 | ||
| Multiple races | 1,754 | 1.2 | 719 | 1.3 | ||
| Missing | 5,515 | 3.7 | 2,121 | 3.8 | ||
| Ethnicity | .04 | <.001 | ||||
| Hispanic | 9,690 | 6.5 | 4,279 | 7.7 | ||
| Non-Hispanic | 135,181 | 91.2 | 50,114 | 89.8 | ||
| Missing | 3,413 | 2.3 | 1,417 | 2.5 | ||
| Marital status | .13 | <.001 | ||||
| Married | 44,879 | 30.3 | 15,265 | 27.4 | ||
| Previously married | 62,309 | 42.0 | 24,006 | 43.0 | ||
| Never married | 38,596 | 26.0 | 14,706 | 26.4 | ||
| Missing | 2,500 | 1.7 | 1,833 | 3.3 | ||
| Homeless status | .09 | <.001 | ||||
| Homeless | 46,259 | 31.2 | 18,997 | 34.0 | ||
| Not homeless | 97,685 | 65.9 | 34,601 | 62.0 | ||
| Missing | 4,340 | 2.9 | 2,212 | 4.0 | ||
| Access to health care system | ||||||
| Distance to VHA specialty care | .22 | <.001 | ||||
| >40 miles | 38,580 | 26.0 | 19,757 | 35.4 | ||
| ≤40 miles | 108,080 | 72.9 | 34,988 | 62.7 | ||
| Missing | 1,624 | 1.1 | 1,065 | 1.9 | ||
| Rurality | .02 | <.001 | ||||
| Urban | 108,242 | 73.0 | 41,219 | 73.9 | ||
| Rural | 35,256 | 23.8 | 12,855 | 23.0 | ||
| Highly rural or island | 1,222 | .8 | 353 | .6 | ||
| Missing | 3,564 | 2.4 | 1,383 | 2.5 | ||
| VHA priority group assignment | .15 | <.001 | ||||
| 1–6 (high-priority service on the basis of service-connected disability or income) | 137,687 | 92.9 | 52,903 | 94.8 | ||
| 7–8 (lower priority; above annual income threshold) | 9,556 | 6.4 | 2,715 | 4.9 | ||
| Missing | 1,041 | .7 | 192 | .3 | ||
| Health insurance status | .21 | <.001 | ||||
| No health insurance | 85,620 | 57.7 | 36,104 | 64.7 | ||
| Health insurance (private, Medicare, or Medicaid) | 59,901 | 40.4 | 17,501 | 31.4 | ||
| Missing | 2,763 | 1.9 | 2,205 | 4.0 | ||
| County characteristic | ||||||
| VA medical center | −.23 | <.001 | ||||
| Yes | 72,212 | 48.7 | 20,885 | 37.4 | ||
| No | 76,072 | 51.3 | 34,925 | 62.6 | ||
| Ratio of population to behavioral health providers (in thousands) (M±SD) | .88±1.59 | .97±1.61 | .05 | <.001 | ||
| Median income (in thousands) (M±SD) | 58.92±14.80 | 57.13±13.06 | −.13 | <.001 | ||
| Unemployment rate (M±SD) | 4.5±1.2 | 4.6±1.2 | .02 | <.001 | ||
| Percentage of households with income below federal poverty level (M±SD) | 15.3±4.8 | 15.6±4.9 | .08 | <.001 | ||
| Only VHA care (N=3,335,426) | Any community care (N=131,584) | |||||
|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | Standardized mean difference | p |
| Veteran behavioral health condition group | .64 | <.001 | ||||
| Serious mental illness | 407,176 | 12.2 | 26,428 | 20.1 | ||
| Substance use disorders | 428,445 | 12.9 | 20,264 | 15.4 | ||
| Posttraumatic stress disorder | 671,222 | 20.1 | 45,058 | 34.2 | ||
| Personality disorders | 14,921 | .5 | 840 | .6 | ||
| Mood disorders | 555,706 | 16.7 | 20,669 | 15.7 | ||
| Anxiety disorders | 139,192 | 4.2 | 3,673 | 2.8 | ||
| Other behavioral health disorders | 60,756 | 1.8 | 1,462 | 1.1 | ||
| Non–behavioral health diagnosisa | 1,058,008 | 31.7 | 13,190 | 10.0 | ||
| Gagne physical health score (M±SD)b | .95±2.01 | .54±1.39 | −.24 | <.001 | ||
| Veteran characteristic | ||||||
| Age (M±SD) | 58.07±17.79 | 50.34±15.53 | −.46 | <.001 | ||
| Sex | .27 | <.001 | ||||
| Male | 2,976,720 | 89.3 | 105,196 | 80.0 | ||
| Female | 358,694 | 10.8 | 25,481 | 19.4 | ||
| Missing | 12 | .0 | 907 | .7 | ||
| Race | .15 | <.001 | ||||
| American Indian or Alaska Native | 29,674 | .9 | 1,851 | 1.4 | ||
| Asian | 35,730 | 1.1 | 2,530 | 1.9 | ||
| Black or African American | 712,943 | 21.4 | 22,471 | 17.1 | ||
| Native Hawaiian or other Pacific Islander | 29,696 | .9 | 1,716 | 1.3 | ||
| White | 2,308,833 | 69.2 | 91,770 | 69.7 | ||
| Multiple races | 35,758 | 1.1 | 2,158 | 1.6 | ||
| Missing | 182,792 | 5.5 | 9,088 | 6.9 | ||
| Ethnicity | .12 | <.001 | ||||
| Hispanic | 231,318 | 6.9 | 12,502 | 9.5 | ||
| Non-Hispanic | 2,994,520 | 89.8 | 113,437 | 86.2 | ||
| Missing | 109,588 | 3.3 | 5,645 | 4.3 | ||
| Marital status | .09 | <.001 | ||||
| Married | 1,615,480 | 48.4 | 63,913 | 48.6 | ||
| Previously married | 1,096,465 | 32.9 | 39,429 | 30.0 | ||
| Never married | 566,983 | 17.0 | 23,308 | 17.7 | ||
| Missing | 56,498 | 1.7 | 4,934 | 3.8 | ||
| Homeless status | .15 | <.001 | ||||
| Homeless | 339,084 | 10.2 | 11,595 | 8.8 | ||
| Not homeless | 2,977,822 | 89.3 | 119,579 | 90.9 | ||
| Missing | 18,520 | .6 | 410 | .3 | ||
| Access to health care system | ||||||
| Distance to VHA primary care | .16 | <.001 | ||||
| >40 miles | 165,552 | 5.0 | 11,532 | 8.8 | ||
| ≤40 miles | 3,164,488 | 94.9 | 119,757 | 91.0 | ||
| Missing | 5,386 | .2 | 295 | .2 | ||
| Rurality | .15 | <.001 | ||||
| Urban | 2,292,912 | 68.7 | 85,981 | 65.3 | ||
| Rural | 956,048 | 28.7 | 40,235 | 30.6 | ||
| Highly rural or island | 35,102 | 1.1 | 1,917 | 1.5 | ||
| Missing | 51,364 | 1.5 | 3,451 | 2.6 | ||
| VHA priority group assignment | .23 | <.001 | ||||
| 1–6 (high-priority service on the basis of service-connected disability or income) | 2,925,189 | 87.7 | 122,871 | 93.4 | ||
| 7–8 (lower priority; above annual income threshold) | 359,024 | 10.8 | 7,195 | 5.5 | ||
| Missing | 51,213 | 1.5 | 1,518 | 1.2 | ||
| Health insurance status | .24 | <.001 | ||||
| No health insurance | 1,408,595 | 42.2 | 67,703 | 51.5 | ||
| Health insurance (private, Medicare, or Medicaid) | 1,856,243 | 55.7 | 59,260 | 45.0 | ||
| Missing | 70,588 | 2.1 | 4,621 | 3.5 | ||
| County characteristic | ||||||
| VA medical center or community-based outpatient clinic | .14 | <.001 | ||||
| Yes | 2,352,547 | 70.5 | 91,184 | 69.3 | ||
| No | 960,622 | 28.8 | 39,601 | 30.1 | ||
| Missing | 22,257 | .7 | 799 | .6 | ||
| Ratio of population to behavioral health providers (in thousands) (M±SD) | 1.00±1.71 | .84±1.29 | −.10 | <.001 | ||
| Median income (in thousands) (M±SD) | 58.73±14.72 | 60.27±14.57 | .10 | <.001 | ||
| Unemployment rate (M±SD) | 4.5±1.2 | 4.5±1.3 | −.01 | <.001 | ||
| Percentage of households with income below federal poverty level (M±SD) | 15.1±4.9 | 14.9±4.6 | −.05 | <.001 | ||
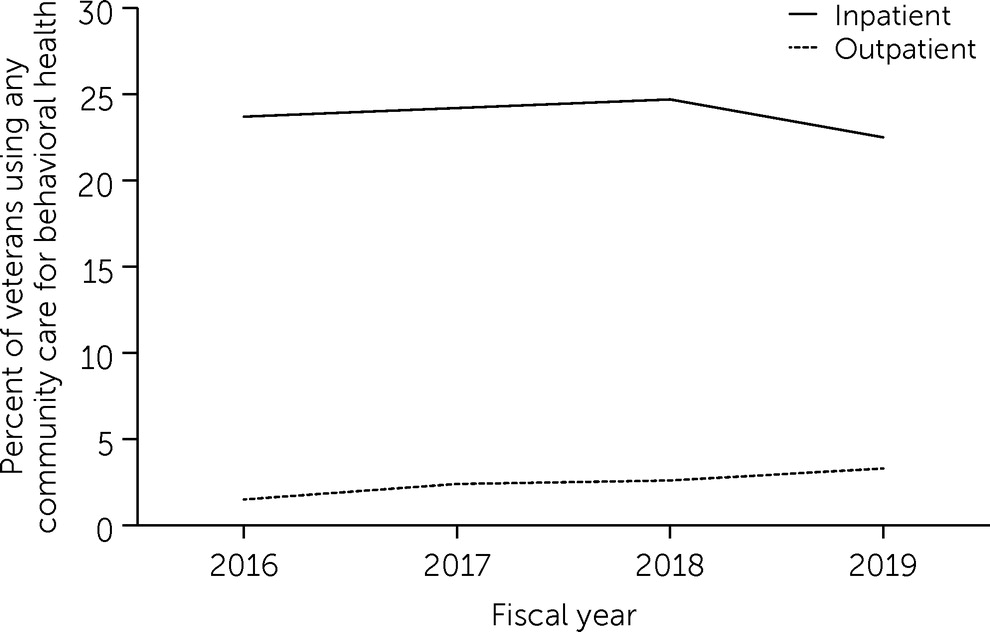
Unadjusted VHA and Community Care Behavioral Health Utilization
Provider Training
| VHA visits | Community care visits | |||
|---|---|---|---|---|
| Provider type | N | % | N | % |
| Psychiatry and behavioral neurology | 11,769,045 | 22.1 | 172,661 | 10.2 |
| Psychology | 13,574,507 | 25.5 | 306,056 | 18.0 |
| Behavioral health advanced practice provider | 2,818,914 | 5.3 | 45,048 | 2.7 |
| Behavioral health counseling and therapy | 3,799,639 | 7.1 | 681,181 | 40.1 |
| Behavioral health social worker | 19,154,090 | 35.9 | 246,609 | 14.5 |
| Psychiatric pharmacist | 176,647 | .3 | 8,217 | .5 |
| Other | 2,053,889 | 3.9 | 237,104 | 14.0 |
Adjusted Probabilities for Behavioral Health Utilization in VHA or Community Care
| Inpatient stay | Outpatient visit | |||
|---|---|---|---|---|
| Characteristic | Probability | 95% CI | Probability | 95% CI |
| Behavioral health condition group (reference: other behavioral health disorders) | ||||
| Serious mental illness | .00 | −.01, .01 | −.02* | −.03, −.02 |
| Substance use disorders | .00 | −.01, .01 | −.00 | −.01, .00 |
| Posttraumatic stress disorder | −.05* | −.07, −.04 | −.00* | −.01, −.00 |
| Personality disorders | −.12* | −.13, −.10 | −.02* | −.02, −.01 |
| Mood disorders | .04* | .03, .05 | −.00 | −.00, .00 |
| Anxiety disorders | −.07* | −.08, −.05 | −.00* | −.01, −.00 |
| Non–behavioral health diagnosis | na | na | −.03* | −.03, −.03 |
| Gagne physical health score | −.00* | −.00, −.00 | −.00* | −.00, −.00 |
| Sociodemographic characteristic | ||||
| Age | −.03* | −.05, −.02 | −.00 | −.00, .00 |
| Male (reference: female) | −.03* | −.05, −.02 | −.01* | −.02, −.01 |
| Race (reference: White) | ||||
| American Indian or Alaska Native | −.02 | −.04, −.01 | −.01* | −.01, −.01 |
| Asian | −.02* | −.04, −.01 | −.01* | −.01, −.00 |
| Black or African American | −.00 | −.02, .01 | −.01* | −.01, −.00 |
| Native Hawaiian or other Pacific Islander | .01* | .01, .01 | −.01* | −.01, −.01 |
| Multiple races | .00 | −.01, .01 | −.01* | −.01, −.00 |
| Non-Hispanic ethnicity (reference: Hispanic) | .01* | .01, .01 | .00* | .00, .00 |
| Marital status (reference: never married) | ||||
| Married | .00 | −.00, .01 | .00 | −.00, .01 |
| Previously married | .00 | −.00, .01 | .00* | .00, .00 |
| Not homeless (reference: homeless) | .02* | .02, .02 | .02* | .02, .02 |
| Access to health care systems | ||||
| Distance to VHA primary or secondary care ≤40 miles (reference: >40 miles) | −.05* | −.06, −.05 | −.03* | −.03, −.03 |
| Rurality (reference: urban) | ||||
| Rural | −.03* | −.03, −.03 | −.01* | −.01, −.01 |
| Highly rural | −.06* | −.06, −.06 | −.01* | −.01, −.01 |
| VHA priority group assignment 1–6 high priority service (reference: lower priority; above annual income threshold) | .01* | .01, .02 | .00* | .00, .00 |
| Health insurance (reference: no health insurance) | −.05* | −.07, −.03 | −.00 | −.02, .01 |
| County characteristic | ||||
| VA medical center or community-based outpatient center (reference: none) | −.00 | −.02, .02 | .01 | −.01, .02 |
| Ratio of population to behavioral health providers | −.00 | −.02, .02 | −.00 | −.01, .01 |
| Median income | −.00 | −.03, .03 | −.00 | −.01, .01 |
| Unemployment rate | −.00 | −.06, .05 | −.00 | −.01, .01 |
| Percentage of households with income below federal poverty level | −.00 | −.04, .04 | −.00 | −.02, .01 |
| Fiscal year (reference: FY2016) | ||||
| 2017 | .01 | −.01, .02 | .01 | −.01, .02 |
| 2018 | .01 | −.01, .02 | .02 | −.00, .03 |
| 2019 | −.02* | −.03, −.00 | .03* | .01, .04 |
| Intercept | −.08 | −.11, −.05 | .14 | .13, .16 |
Discussion
Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 374.24 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).