Suicide is the second leading cause of death among 10- to 25-year-olds (
1). Suicidal behaviors are three to four times more likely among youths in the juvenile legal system (
2–
5) than among their peers outside the system. Fifty percent of youths experience suicidal ideation while in juvenile detention (
6). Because of social and structural factors, including racism (
7), Black youths are disproportionately represented in detention (
8). Thus, placement in detention is an event that puts youths at high risk for suicidal behavior and that disproportionately affects Black youths. Comprehensive implementation of suicide prevention is needed in juvenile detention to support this group of at-risk youths and to ensure that existing disparities in mental health care for Black youths are not exacerbated (
9).
The National Center on Institutions and Alternatives conducted the only national survey in the United States of youth suicide in confinement, identifying 110 deaths by suicide between 1995 and 1999 (
10). The survey assessed the implementation of suicide prevention programming in facilities where suicide deaths occurred. Nearly all (95.5%) facilities with a youth suicide death had implemented a suicide prevention practice, but only 20% had implemented the national standard for suicide prevention at the time. More than 40% of suicide deaths occurred in facilities that did not provide suicide prevention training to their staff. The author of the study reporting the survey findings concluded with a call to channel resources to the juvenile legal system in order to improve suicide prevention implementation and to provide comprehensive suicide prevention training to facility personnel.
In response to these alarming findings, the Youth in Contact With the Juvenile Justice System Task Force of the National Action Alliance for Suicide Prevention (NAASP) developed evidence-based guidelines, organized into eight components (
Table 1), to inform juvenile detention centers’ suicide prevention implementation (
11). Juvenile legal systems receive oversight at the state level and policy administration at the county level. In the northeastern state that was the site of the study reported here, the state regulations in place to protect the health, safety, and well-being of youths in juvenile detention align with the NAASP juvenile detention guidelines. However, administration of state regulations falls under the purview of local counties, which could lead to variable implementation across counties.
The field of implementation science is dedicated to understanding and targeting the causes of variability in implementation of evidence-based practices (EBPs) (
12). Aligned with core implementation outcomes frameworks (
13), key implementation outcomes include the appropriateness of the EBP (i.e., perceived fit), adoption of the EBP within the system (i.e., number of stakeholders using the practice), and the fidelity with which the EBP is implemented (i.e., degree to which a practice is implemented as intended) (
13). Prior research demonstrates that one of the most influential determinants of EBP implementation is organizational leadership (
14–
19). For example, Aarons et al. (
15) evaluated the systemwide implementation of an EBP and found that organizational leaders were crucial to both the implementation and sustainment of the intervention. Given this finding, detention center leaders (e.g., executive directors) likely have a pivotal role in influencing suicide prevention implementation in their centers and are best positioned to describe that role and their centers’ current suicide prevention practices.
The aim of the current study was to evaluate, for the first time, implementation of the NAASP guidelines for suicide prevention in one state’s juvenile detention centers and the guidelines’ influence on youth suicidality during detainment. We investigated four research questions. First, we explored leaders’ and staff members’ perceptions of the role of detention centers with regard to suicide prevention (i.e., appropriateness). Second, we identified which suicide prevention components leaders and staff report using in their juvenile detention centers (i.e., adoption). Third, we explored the quality with which these components were implemented. Finally, we considered whether there were associations between leaders’ perspectives on juvenile detention centers’ role in suicide prevention, the quality of suicide prevention implementation, and suicidality of youths while detained.
Methods
Recruitment and Data Collection
Our work was conducted within the context of a community-academic partnership (
20) and was grounded in principles of community-based participatory research (CBPR) (
21). Executive directors of detention centers in a northeastern state were recruited by e-mail. A juvenile detention center was eligible if it was located in the state of interest. The first e-mail was sent by the executive director of the National Partnership for Juvenile Services (NPJS), a national organization that provides technical assistance to juvenile detention centers. All subsequent weekly e-mails (up to five attempts to contact were made) were sent by the study team. The detention center executive director could decide to be interviewed or to delegate participation to another leader (e.g., deputy director) and whether to include other members of their team in the interview. The study team ensured that a director (executive or deputy) was interviewed at each site because these individuals arguably have the most comprehensive knowledge of both overarching organizational policies and day-to-day procedures.
We exhaustively sampled for all detention centers in the state. Twelve detention centers were eligible for the study. Of these, we successfully recruited stakeholders from 10 (83%). The remaining two centers did not respond to e-mail inquiries; the study team did not contact the two centers beyond the e-mails described above, and the team did not solicit feedback as to why the centers elected not to participate.
All interviews were completed by the first author (B.N.R.) from February 6, 2020, to March 13, 2020. At the beginning of each interview, a script was read to facilitate verbal consent to participate. After consent was received, an interview guide was utilized to facilitate the semistructured interviews. The mean±SD interview duration was 42.75±11.50 minutes. Most interviews occurred in a single session, although two interviews were completed across two dates because of the abundance of information communicated. Consistent theme recurrence began by the fifth interview, suggesting that saturation was met. All interviews were conducted through HIPAA-compliant BlueJeans technology and were recorded for transcription. All interviews were transcribed by the study team verbatim for analysis, with one team member acting as a transcriptionist and a second person (E.N.P.) checking the finalized work. Participants were not compensated because of union and employment laws. The University of Pennsylvania Institutional Review Board deemed this research exempt.
Semistructured Interview Guide
A semistructured interview guide was developed with the goal of learning about the suicide prevention components used within the juvenile detention centers as well as barriers to and facilitators of suicide prevention implementation. This study focused on the use of suicide prevention components. (The interview guide questions relating to the current study are available in the
online supplement to this article.) Inclusion of community members and stakeholders in the design of qualitative research processes is a standard practice of qualitative research and of CBPR more broadly (
21). We partnered with the executive director of NPJS in the development of the research design and interview guide. One author (S.E.S.) was a detention center staff member at the time of the project and confirmed the usability of the interview guide. This author was not employed by any of the detention centers in the sample.
The interviewer began by asking participants to describe their role at the center. Subsequently, the interviewer asked open-ended questions to understand the use of suicide prevention at each center. The first six interview guide questions were asked of all interviewees, whereas the remaining questions functioned as subprompts to gather further information about the NAASP guidelines. The interviewer also sought to identify information that detention centers regularly collect through administrative data, especially variables related to youth mental health and suicidality. This information included average census and the frequency of crisis stabilization calls and critical incidents (e.g., incidents related to suicidality and behavioral incidents such as use of restraints and aggression) a facility experienced. Because this was an exploratory process with the goal of determining the optimal wording to elicit the most accurate information, the wording of these questions differed slightly across interviews. For example, the interviewer initially asked how many crisis calls a facility received in the past month but learned that it was most helpful to ask for the average number of crisis calls per month.
Data Analysis
Implementation appropriateness: juvenile detention centers’ role in suicide prevention.
The study team thematically analyzed (
22) all interviewee responses to the interview guide question, “What role do juvenile detention centers play in preventing suicide?” Four team members independently reviewed and summarized their notes, and then met to consolidate findings and create a consensus summary.
Implementation adoption: suicide prevention components utilized in juvenile detention centers.
The study team developed a strategy grounded in content analysis techniques (
23) to code the interview transcripts for mentions and descriptions of suicide prevention components. A deductive approach was used to iteratively design the codebook (
24), with a priori codes informed by NAASP guidelines (
11) (the codebook is available in the
online supplement).
Two coders (C.N.G., S.E.S.) double-coded all transcripts, with coding discrepancies arbitrated through discussion. In alignment with existing literature (
25–
29), the study team elected not to conduct interrater reliability testing for this study, because the number of uncoded transcript segments (i.e., segments irrelevant to suicide prevention) would have inflated the final kappa coefficient and because full consensus was achieved. The study team calculated the level of adoption of suicide prevention components for each facility. A suicide prevention component was included in a facility’s total adoption score if it was mentioned in the interview (i.e., quality was not considered). Component adoption scores range from 0 to 8, with higher scores indicating a greater number of adopted components.
Implementation quality.
The study team was unable to assess the fidelity with which the suicide prevention components were implemented because observation was not possible. The team developed a method to preliminarily assess implementation quality via the interview (
13). The NAASP guidelines (
11) specify how to comprehensively implement each suicide prevention component. Forty-two quality indicators comprise the eight suicide prevention components. For example, for housing, one quality indicator is that the emergency equipment in each housing unit is checked by staff daily.
Two coders (C.N.G., S.E.S.) reviewed all interview transcripts and identified excerpts in which center leaders or staff described adhering to quality indicators. These excerpts formed the basis for a final quality rating for each facility. A facility’s quality rating used the total number of quality indicators adhered to across all eight suicide prevention components. These quality ratings were calculated as a percentage (i.e., a facility that met 10 of the 42 quality indicators would receive a quality rating of 24%). We also disaggregated the number of quality indicators by each of the eight individual components. (The final quality indicator codebook is available in the online supplement.)
Associations between the quality of suicide prevention implementation, leadership perspectives on detention centers’ role in suicide prevention, and youth suicidality.
We conducted a mixed-methods analysis using two joint display tables. Joint displays are an emergent technique for organizing, comparing, and integrating qualitative and quantitative data to illuminate new insights (
30). Our first joint display shows the association between center characteristics and the frequencies of crisis calls and critical incidents with staff members’ and leaders’ perceptions of detention centers’ role in suicide prevention. Our second joint display enables comparison of the detention centers with the highest and lowest quality ratings in our data set with regard to the quality of their suicide prevention implementation, their size, their frequencies of crisis calls and critical incidents, and their leaders’ perspectives on detention centers’ role in suicide prevention.
Results
Table 2 provides information regarding interviewee and site characteristics. In alignment with CBPR and qualitative research standards, analytical results were disseminated to NPJS leadership for review. Such a procedure is known as member checking, a qualitative research technique in which researchers increase the accuracy and internal validity of their results by requesting feedback from community members with lived experience or subject matter expertise (
31). Both individuals who participated in the study’s member check agreed that the results were in line with their knowledge of and experience with juvenile detention. They further felt that the results were representative of detention centers at the state and national levels.
Implementation Appropriateness
Many detention center leaders struggled to identify the role detention centers play in preventing suicide (i.e., proactive responsibility). One center leader (site 5) said, “I’ve never thought of us as [preventing suicide]. . . . I’ve had kids tell me that them being there is what’s causing [their] suicid[al] ideations, because no one wants to be in detention.” This leader highlighted the potential iatrogenic effects that detention center placement can have on youth mental health and suicide risk. Nearly all leaders mentioned placement in a detention center as an opportunity to identify youth suicidality that had not previously been detected (i.e., reactive responsibility). For example, one center leader (site 3) said, “I think one of the best things that detention does is . . . we do a really good job of assessing [youths] and beginning the treatment process.” Leaders mentioned that, when feasible, the goal of providing services within centers is to stabilize youths and return them to society rather than to provide long-term or preventive care.
Detention center leaders believed that their primary responsibility for suicide prevention is ensuring the physical safety of all youths, which is accomplished via three avenues. First, detention centers detect existing suicidality through formal and informal assessments. As one detention center leader (site 10) commented, “[We’re] making sure we’re establishing a rapport with our children to make sure they can feel comfortable with disclosing anything.” Second, centers monitor youths to maintain their physical safety: “I think the biggest [way we prevent suicide] is obviously monitoring, but also identifying . . . the kids and [their] behavior or the mental health signs that they might be showing . . . on an hour-to-hour basis” (site 4). Last, leaders noted that centers ideally act as a bridge between a youth’s past placement and wherever they are discharged to: “We [hold youths] until [the courts] determine what the best course of action [is] for treatment” (site 7).
Implementation Adoption
Leaders at all 10 detention centers mentioned using at least seven of the eight NAASP components. Only one facility (site 10) explicitly reported using mortality-morbidity review.
Implementation Quality
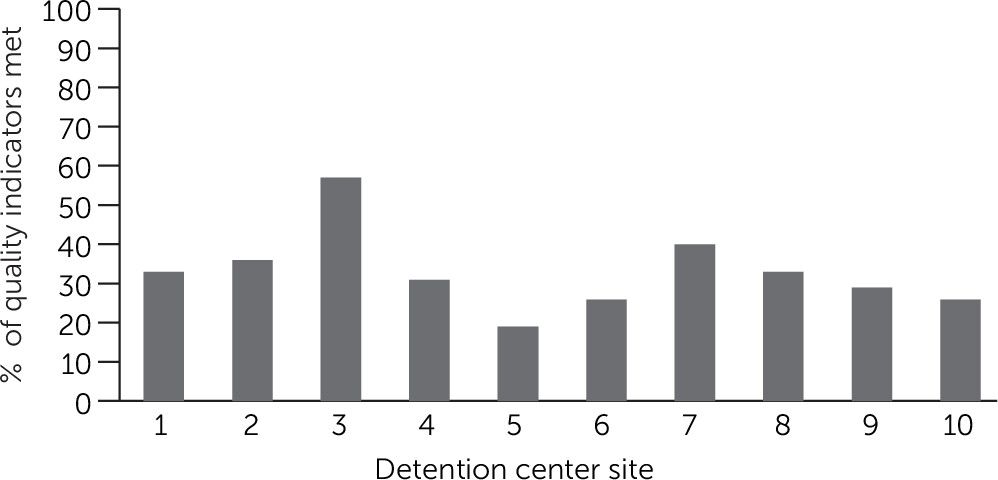
Figure 1 and
Table 3 show suicide prevention quality ratings by detention center, and
Table 3 also stratifies quality ratings by NAASP component. Quality ratings ranged from 19% (eight of 42 quality indicators) to 57% (24 of 42 quality indicators). The component that was implemented with the highest quality was communication, with facilities describing an average adherence rate of 70% (4.2 of 6.0 possible quality indicators). The components that were implemented with the lowest quality were mortality-morbidity review and intervention, each with only one facility reporting a single quality indicator of that component.
Associations Between Quality of Suicide Prevention Implementation, Perceived Role of Detention Centers, and Youth Suicidality
The data provided in our first joint display examined the association between center characteristics and the frequencies of crisis calls and critical incidents with staff members’ and leaders’ perceptions of detention centers’ role in suicide prevention (
Table 4). Interviewees from detention centers with the lowest number of crisis calls viewed suicide prevention as an important part of their centers’ mission or clearly explained how the role of detention centers fits into a larger picture of suicide prevention, including by intervening to support youths while they are detained. Interviewees from centers with a moderate number of crisis calls were likely to define the role of detention centers in suicide prevention as being a connector to care outside the detention center rather than as focusing on intervention while youths are detained. Finally, interviewees from detention centers with the highest number of crisis calls were unsure of the role of these centers in suicide prevention or thought that they caused rather than prevented suicidality. Taken together, these data preliminarily suggest that staff members’ and leaders’ perceptions of the role of detention centers in suicide prevention may be associated with the level of suicidality in a center.
A second joint display (online supplement) juxtaposes the suicide prevention practices, leadership perceptions, and facility characteristics of the highest-performing site (overall quality rating, 57%) with those of the lowest-performing site (overall quality rating, 19%). It illustrates divergences in the quality of suicide prevention implementation and suggests how these differences may correspond with both the perceived role of detention centers in suicide prevention and youth suicidality.
The highest-performing site (site 3) was classified as a medium-to-large facility and had approximately 35 beds. The site averaged six to 12 crisis stabilization calls and five critical incidents per year. Per the interview, the site’s leader believed that juvenile detention centers played a critical role in suicide prevention. Interviewees at this detention center were able to identify their center’s role in suicide prevention (i.e., the facility’s triage procedures used to assess and respond to a youth’s needs). Interviewees framed their center as being the “first step” in treating the root causes that led to a youth’s detention. The lowest-performing site (site 5) was classified as a small facility and had approximately 15 beds. The site averaged 55 crisis stabilization calls and 27 critical incidents per year. The interviewee at this detention center (a facility leader) stated that they had “never thought of” their center as playing a role in suicide prevention, and, in fact, felt that detention was iatrogenic. They noted that the facility’s resources and monitoring could play a role in suicide prevention.
Despite housing more youths than the lowest-performing site, the highest-performing site had fewer crisis stabilization calls and critical incidents. Taken together, the contextual information about the two sites and the sites’ suicide prevention quality suggest that having higher-quality suicide prevention implementation may be related to the number of crisis stabilization calls and critical incidents. In addition, facility leaders’ and staff members’ perceptions about the role their center plays in suicide prevention may influence the quality of suicide prevention in juvenile detention centers.
Discussion
We conducted a case study of suicide prevention implementation at juvenile detention centers in one northeastern state. We sought to understand how well juvenile detention centers are serving the needs of suicidal youths under their purview. Most leaders considered their role to be reactively managing suicidality, when it manifests during youth detainment, rather than proactively preventing it. One leader felt that detention was iatrogenic, and existing literature supports this idea. Placement in a detention center can lead to negative psychosocial outcomes (
32), including increased mental health concerns (
33) and vulnerability to complex trauma (
34). These outcomes, in turn, may contribute to the high rates of suicidality among youths in these settings (
35). The center leaders in our sample emphasized that detention centers are not treatment facilities; rather, they are a short-term placement to maintain youths’ physical safety before they reintegrate into the community.
Many leaders believed that placement in juvenile detention is an opportunity to identify suicidality and that this identification can be used to maintain physical safety and influence discharge planning. These views align with proactive models of suicide prevention, including the National Strategy for Suicide Prevention—i.e., the Zero Suicide model (
36–
38). The Zero Suicide model proposes that comprehensive suicide prevention requires health care organizations to universally screen for suicide risk, use that information to make decisions about care and discharge planning, and provide interventions that maintain patient safety. Our findings suggest that implementing proactive suicide prevention models, including the Zero Suicide model, may be appropriate in juvenile detention. Given that youths are detained for short periods, brief interventions (i.e., delivered in a single session) targeting suicidality are needed within these models for this setting. Evidence suggests that brief suicide interventions can prevent suicidality (
39) and that interventions such as the Stanley-Brown Safety Planning intervention (
40) are feasible in juvenile detention centers (
41).
Our mixed-methods analysis of the association between staff members’ and leaders’ perceptions of the role that detention centers play in preventing suicide and the frequencies of crisis calls and critical incidents at the centers suggests that these perceptions may be a target of intervention to improve suicide prevention in juvenile detention. Interviewees from centers that had the fewest crisis calls described their center’s role in preventing suicide with clarity and ease. They emphasized how important suicide prevention is to their center’s mission. Conversely, interviewees from the centers with the most crisis calls had difficulty describing this role, and in some cases they did not appear to consider suicide prevention as part of their center’s role. Our exploratory mixed-methods analysis comparing the detention center with the highest suicide prevention quality with the center with the lowest quality suggests that leadership perspectives may be associated with the quality of suicide prevention implementation. Interviewees from the center with the highest quality rating viewed the center’s role as supporting suicide prevention, whereas the interviewee from the center with the poorest rating felt that their center had a less clear-cut role or was iatrogenic. Because these analyses were exploratory, future work should assess whether leadership’s perceptions of the role juvenile detention centers play in suicide prevention are causally related to implementation. Previous research has demonstrated that attitudes toward and beliefs about EBP implementation can influence implementation adoption (
15,
17,
19). In alignment with the Zero Suicide model, targeting leadership attitudes toward and beliefs about the role detention centers play in preventing suicide and hiring staff with these values could be important strategies to improve suicide prevention implementation.
Detention center leadership and staff reported the use of a broad range of suicide prevention components at their facilities. Two decades ago, when the National Center on Institutions and Alternatives conducted its survey, only 31% of detention centers implemented six or more suicide prevention components, as defined by the national juvenile correctional standards and practices at that time (
10,
42). In the current study, all detention centers mentioned using seven of eight of the NAASP components—an improvement. Further analysis showed that detention centers were not implementing practices with high quality. All but one site had a quality rating under 50%. Some components were implemented with higher quality than others. Facilities appeared to implement the communication component with the highest quality. Communication about detained youths among staff is not unique to suicide prevention and is needed to effectively run a facility, which may be why this component was implemented with higher quality than other strategies that were more specific to suicide prevention.
The goal of implementing suicide prevention is to prevent suicidal behavior. To preliminarily explore whether the quality of suicide prevention implementation in facilities influences youth suicidality, we conducted a mixed-methods analysis integrating the quality of suicide prevention implementation and variables related to suicidality (crisis stabilization calls and critical incidents). The facility with the highest quality rating experienced fewer critical incidents and crisis stabilization calls than the facility with the lowest quality rating, even though the former facility served more youths. If our findings are replicated, they may suggest that implementing the NAASP guidelines with higher quality corresponds to fewer suicide-related emergencies in detention. Conversely, not implementing suicide prevention well could perpetuate existing disparities in mental health. This finding emphasizes the importance of supporting juvenile detention centers in their suicide prevention implementation.
Our results should be interpreted in the context of several important limitations. This study was conducted within one state, potentially limiting generalizability. We were also unable to directly observe the implementation of the suicide prevention components (i.e., fidelity assessment) and instead relied on leaders’ and staff members’ reporting. Our method could have resulted in under- or overidentifying the number of components used by the centers. Furnishing behaviorally specific examples of how centers are following a component is likely a better way to measure and monitor quality (
43). A further limitation to the interviews was that the study team was unable to ask all interview questions at every site. We did not detect systematic patterns in which questions were asked at various sites. Finally, we did not uniformly gather information about crisis stabilization calls and critical incidents. Because this study was exploratory and aimed to inform future research, we sought to understand the types of administrative information detention centers routinely collect that are related to suicidality. We quickly learned that crisis stabilization calls and critical incidents are carefully monitored, systematically documented, and reported to the state. Because we did not systematically collect this information in every interview, we were unable to assess statistical significance of the relationships between implementation quality and these variables, and we used an exploratory mixed-methods approach. This type of investigation is ripe for future research.
Conclusions
Our findings suggest that there is room for improvement regarding the implementation of suicide prevention within juvenile detention centers. Improving the quality of suicide prevention in these centers could save lives. Although our work was conducted in one state, we believe that our findings have broad and urgent implications for all detention centers. It is imperative that all detention centers implement suicide prevention practices well. In the matter of youth suicide, a delay is not acceptable. The time to act is now.
Acknowledgments
The authors thank the National Partnership for Juvenile Services for supporting this project as well as the detention center leaders and staff, who were willing to contribute to suicide prevention reform in their state.