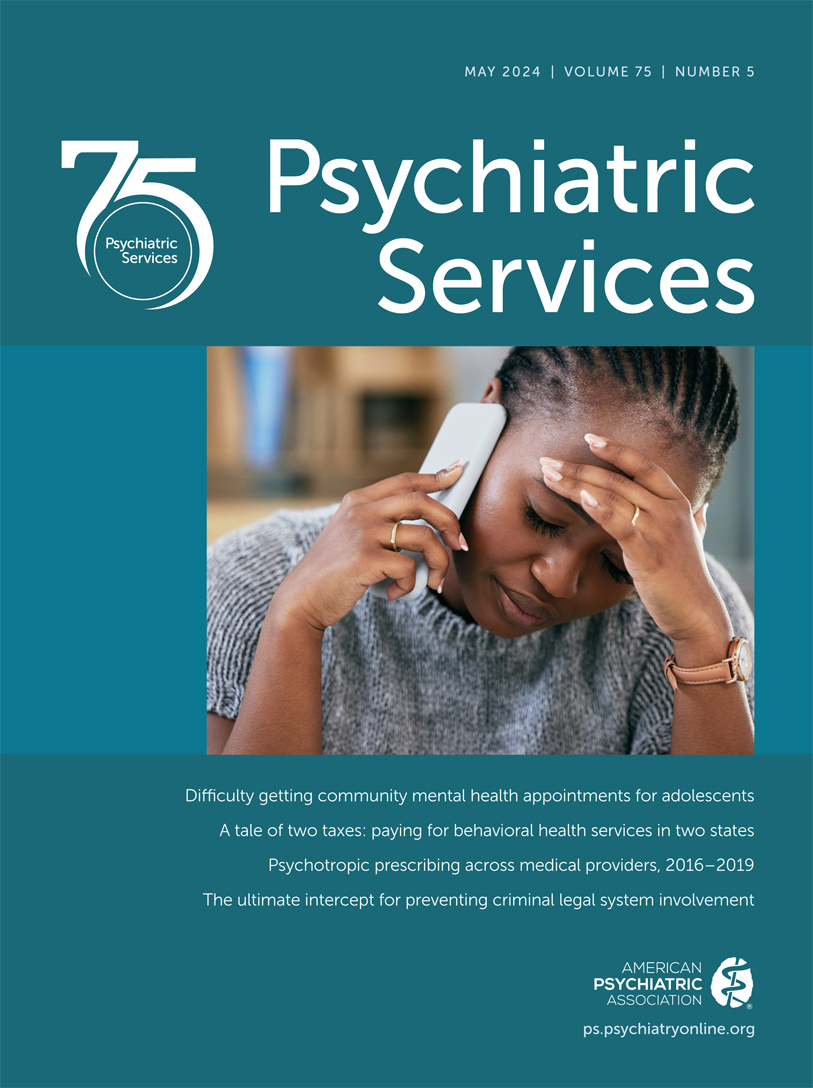
The experience of adverse childhood events (ACEs) increases the likelihood of deleterious mental health outcomes. Individuals from disadvantaged backgrounds and minoritized racial and ethnic groups experience a disproportionate number of ACEs relative to their counterparts. The COVID-19 pandemic exacerbated mental health hardships that youths experienced because of social isolation, lack of peer interaction, financial hardships, and surges in domestic violence and sexual abuse. Youths from racial and ethnic minority groups also experienced a disproportionate share of COVID-19–related morbidity and mortality, which may have further increased their need for mental health treatment. This higher need proves troublesome in that minoritized groups historically have had lower rates of mental health treatment access and use.
Trauma-informed care is a critical component of mental health treatment, especially so for youths who have experienced some form of trauma. This treatment approach is guided by patient empowerment, collaboration, safety, trust, and patient preference. Engaging in trauma-informed care may lead to improvements in anxiety, depression, emotional dysregulation, and posttraumatic stress disorder and to reductions in risky behaviors. Having timely access to this form of care can be helpful for youths experiencing higher rates of ACEs.
In this issue, Adams and colleagues (
1) used a mystery shopper study design to examine differences in trauma-informed mental health service access at safety-net health centers (community mental health centers [CMHCs] and federally qualified health centers [FQHCs]) by insurance type (Medicaid and private) and care seekers’ race and ethnicity. Findings suggest that accessing any mental health care was difficult: only 17% of contacts with either a CMHC or FQHC resulted in an appointment. Of completed contacts, 38% of schedulers reported having trauma-informed care, whereas 38% reported not being sure and 10% reported not having that type of service; in 13% of calls, schedulers ended contact before the question could be raised. When schedulers were unsure whether their facility offered trauma-informed care, only 4% provided callbacks with additional information on services. The most common reason for no appointment at FQHCs was lack of an in-network provider (62%). At CMHCs, capacity was an issue; most callers were placed on a waitlist (39%) or told the waitlist was closed (28%). The odds of not getting an appointment at either an FQHC or a CMHC were significantly higher for Black and Latinx callers versus White callers.
The inability to receive timely treatment when needed may intensify youths’ mental health conditions and lead to negative consequences in the long term. Researchers’ findings that Black and Latinx callers were more likely to be denied an appointment indicate that existing mental health treatment disparities will be exacerbated, adversely affecting populations with high ACE rates.
This study highlights many of the nationwide barriers to accessing services for youths. The shortage of mental health professionals accepting any insurance, the increasing demand for services due to Medicaid expansion and the health insurance exchanges, and the growing need for treatment because of pandemic effects are overwhelming the mental health care system. Pairing these barriers with implicit bias and institutional racism further complicates treatment access—and for some, treatment becomes unattainable.
Efforts are needed at state and federal levels to increase mental health treatment access for youths seeking treatment. To increase the mental health workforce, policy makers should consider increasing reimbursement rates, enforcing health insurance parity, reimbursing new provider types, and reimbursing care delivered by trainees or license-eligible providers. Better financing of safety-net facilities is also needed to avoid administrative barriers to care and staffing shortages. Safety-net facilities, which provide services to a disproportionate share of low-income racial and ethnic minority groups, should continue focusing on the needs of culturally and linguistically diverse individuals. As the U.S. population continues to endure the ramifications of the pandemic and the exacerbation of ACEs, the systems of care need to equitably increase the availability of evidence-based trauma-informed care.