Contemporary standards of care require mental health clinicians to evaluate and manage their patients' risk of violence in settings such as inpatient units and emergency rooms. However, the existing research literature provides limited guidance about what variables actually increase patients' risk of violence. Recent epidemiological studies have suggested that psychotic symptoms (
1,
2,
3) and substance abuse (
4,
5,
6) may be particularly useful indicators of violence potential. However, research on the specific types of psychotic symptoms that are related to violence potential is limited (see McNiel [
7] for a review).
This study describes the relationship between a particular psychotic symptom—command hallucinations —and violence in a group of hospitalized patients. Previous research has suggested a positive though modest association between hallucinations and violence (
8,
9). Clinical experience suggests that some patients who have hallucinations commanding them to engage in violent behavior do engage in such behavior. The empirical literature on the relationship between command hallucinations and violence is small and contains widely conflicting results. Some authors have reported that patients rarely comply with command hallucinations (
10,
11,
12,
13), whereas others have reported that unquestioning obedience is quite common (
14).
Previous research on this topic has been limited by failure to consider concurrently other correlates of violence such as demographic variables and substance abuse, use of unstandardized measures of symptoms and violence, and failure to consider response sets in evaluating self-reports of hallucinations—that is, some people are motivated to exaggerate or minimize deviant experiences for reasons such as secondary gain.
Our study provides information about the relationship between command hallucinations and violence in a group of patients hospitalized in a civil, nonforensic context. We describe the frequency of command hallucinations to harm others, the rate of compliance with such command hallucinations, and the relationship between this type of command hallucination and violent behavior. To place these hallucinatory experiences in the context of other correlates of violence, we also report analyses that include demographic variables, history of substance abuse, other psychotic symptoms, and proclivities toward a social desirability response bias that might influence patients' self-reports of hallucinations.
Methods
The study was conducted on a short-term psychiatric inpatient unit at a university hospital. Between November 1995 and June 1996, a total of 103 patients filled out a series of questionnaires as part of a larger study of psychopathology, mood, and aggression. The subset of the questionnaires pertinent to this report is described in the sections that follow. To recruit participants when they were stable enough to complete the questionnaires in a consistent fashion, we invited all eligible patients to participate in the study three days after admission or later, when they were organized enough to participate. Participants were paid $10 for their participation in the larger study.
After the study was completely described to the subjects, informed consent was obtained. The protocol for the study was approved by the committee on human research of the University of California, San Francisco. Patients were not eligible to participate if they were not literate in English, had a diagnosis of dementia, were under 18 years of age, or had been hospitalized for less than four days.
Measures
Hallucinatory experiences. Given the subjective nature of command hallucinations and the absence of a generally accepted standardized measure of them, we developed a series of questions with face validity concerning different types of hallucinations. In this broader array of content, we embedded two items specifically about command hallucinations: "During the past year, how often have you heard voices telling you to hurt other people?" and "During the past year, how often have you complied with voices telling you to hurt other people?" Patients rated each item on a 5-point scale ranging from 0, never, to 4, very often.
Psychotic symptoms. The Psychiatric Epidemiology Research Interview (PERI) has been widely used in studies of psychopathology and has demonstrated reliability and validity in this context (
2,
3,
17,
18). The psychotic symptoms subscale of the PERI (
17) includes 13 items about positive psychotic symptoms, such as thought control, thought insertion, paranoia, thought broadcasting, and thought withdrawal. Subjects are asked to rate their experience with these symptoms in the past year on a 5-point scale ranging from 0, never, to 4, very often.
Violence. We assessed violence using a questionnaire based on items from the MacArthur Community Violence Instrument (
19). The MacArthur scale includes items about various aggressive behaviors, and it has documented reliability and validity in the measurement of violent behavior by psychiatric patients (
6,
20), including demonstrated correspondence with other indicators of violence such as reports from collateral sources (for example, family members and friends).
On the violence scale, we operationally defined violent behavior as a report of any act of physical aggression against other people or of threatening others with a lethal weapon within the past two months. This definition corresponds to level 1 and level 2 violence as originally defined by the MacArthur Foundation Research Network on Mental Health and Law (
20) or to the more recent categorization of "violence" and "other aggressive acts" (
6).
Social desirability. We measured social desirability response biases with a 13-item version of the Marlowe-Crowne Social Desirability Scale (
21), a widely used questionnaire. The items were originally selected for inclusion on the scale to describe culturally approved behaviors that have a low incidence of occurrence (
22) and are also not linked to psychopathology. This questionnaire frequently has been used to permit interpretation of responses on self-report measures while taking into account individuals' general tendencies to describe themselves in ways that are or are not approved of by society.
Demographic and diagnostic characteristics. We reviewed patients' medical charts to obtain information on demographic characteristics and clinical diagnoses.
Data analysis
Chi square analysis, corrected for continuity, was used to evaluate the association between command hallucinations and violence. Multivariate logistic regression was used to determine the relationship between command hallucinations and violence while concomitantly considering other correlates of violence.
Results
Study group characteristics
Of the 103 participants in the study, 61 (59.2 percent) were male. Sixty-one (59.2 percent) were white, 22 (21.4 percent) were African American, and 20 (19.4 percent) were of other ethnic backgrounds. The mean±SD age was 40.7±13.6 years (range, 18 to 84 years). Fifty-seven patients (55.3 percent) had never been married; 30 (29.1 percent) were separated, divorced, or widowed; and 16 (15.5 percent) were married or living with a partner.
On the basis of DSM-IV chart diagnoses, 21 (20.4 percent) had schizophrenic disorders, 13 (12.6 percent) had other psychotic disorders, 11 (10.7 percent) had bipolar disorder (manic episode), 44 (42.7 percent) had other mood disorders, 30 (29.1 percent) had substance-related disorders, 13 (12.6 percent) had personality disorders, 11 (10.7 percent) had adjustment disorders, and seven (6.8 percent) had other disorders. (The total exceeds 103 because of comorbidity.) Forty-six patients (44.7 percent) reported that they had engaged in violent behavior during the two months before hospital admission.
Rates of command hallucinations
Thirty-one of the patients (30.1 percent) reported having heard voices telling them to hurt others during the past year—four had heard such voices very often, seven had heard them often, 12 sometimes, and eight almost never. Twenty-three patients (22.3 percent) said they had complied with voices telling them to hurt other people—five said they had complied often, nine sometimes, and nine almost never. Patients who reported having experienced command hallucinations to hurt others constituted a subset of patients who had hallucinations. Fifty-seven patients (55.3 percent) reported having heard things that others say they cannot hear, and 52 (50.4 percent) said they had had visions or seen things that other people say they cannot see.
Command hallucinations and violence
To evaluate the relationship between command hallucinations and violence, the study group was divided into those who did and those who did not report having had any command hallucinations to hurt others. Patients who had command hallucinations to hurt others were significantly more likely to report a history of violence during the two months before hospital admission. Twenty-one of 31 patients (67.7 percent) who reported having heard voices telling them to hurt others also reported a recent history of violence, compared with 25 of 72 patients (34.7 percent) who had not had violent command hallucinations (χ2=8.27, df=1, p=.004).
To put the relationship between command hallucinations and violence in context, we performed supplemental analyses of the relationship between violence and other variables that previous research had suggested to be related to violence. Kendall's tau correlations showed that violence was associated with higher levels of psychotic symptoms as measured by the PERI (tau=.35, p<.001), presence of a substance-related disorder (tau=.24, p<.02), and male gender (tau=.23, p<.03), but not with age (tau=.15, ns). Patients who reported violence tended to score lower on the Marlowe-Crowne Social Desirability Scale (tau=-.24, p<.004).
Logistic regression analyses
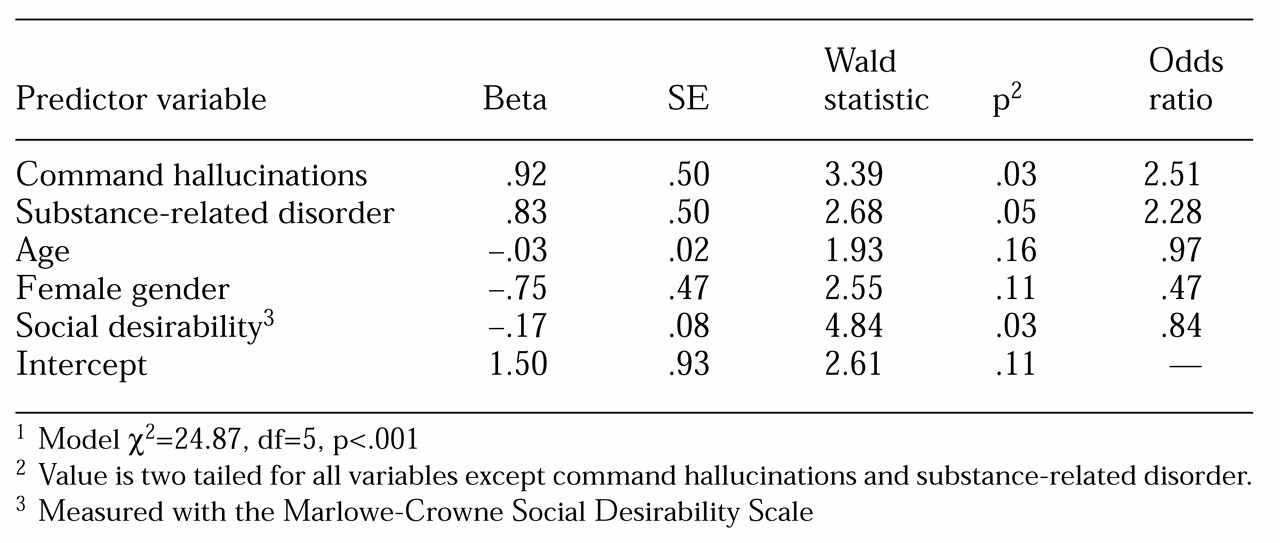
We used multivariate logistic regression analysis to determine the relationship between command hallucinations and violence when other correlates of violence are also taken into account. Specifically, we conducted a forced-entry logistic regression in which the presence or absence of violence was predicted by the presence of command hallucinations to harm others, the presence of a substance-related disorder, age, sex, and score on the Marlowe-Crowne Social Desirability Scale.
As shown in
Table 1, the presence of command hallucinations was a significant predictor of violence. Computation of odds ratios showed that patients who experienced command hallucinations were more than twice as likely to be violent. Among the control variables, the presence of a substance-related disorder predicted violence, as did male gender and low levels of social desirability response bias.
To determine whether command hallucinations contributed to prediction of violence even when the analysis controlled for a diagnosis of a schizophrenic disorder or bipolar disorder (manic episode), we conducted subsidiary logistic regression analyses that included the presence or absence of these diagnoses. In these subsidiary analyses, command hallucinations continued to be a significant (p<.05) predictor of violence, suggesting that the relevance of this symptom to violence risk is not redundant with diagnosis.
However, when we conducted an additional logistic regression analysis that included the extent of any psychotic symptoms, as measured by the psychotic symptoms subscale of the PERI, command hallucinations no longer made a significant contribution in determining violence risk over and above the other predictors. Hence, although command hallucinations do appear to be reliably associated with violent behavior, this association occurs in the context of other positive psychotic symptoms' also being associated with violence. This collinearity may represent an association between violence and an underlying disease process that is associated with both command hallucinations and other positive psychotic symptoms.
Discussion
As health care moves toward a greater emphasis on evidence-based practice, clinicians are increasingly expected to have a scientific basis for their opinions and decisions (
23). Similarly, mental health testimony in forensic settings is increasingly expected to have a demonstrable scientific basis (
24). Clinical evaluation of patients' risk of violence requires consideration of various demographic, personal history, clinical, and situational variables (
7,
19,
25). Command hallucinations are one clinical variable with widespread commonsense acceptance in the professional lore as a risk factor for violence, despite an inconsistent scientific database. This study provides data related to this widely held belief.
Our findings suggest that on a unit where most patients are civilly committed, when patients are asked specifically about command hallucinations to hurt others, they fairly commonly report having had such experiences. Roughly one-quarter of the patients in our study group acknowledged having had command hallucinations to hurt others in the past year. Previous research with forensic inpatients (
14) and voluntary outpatients (
13) has suggested that when interviewers specifically inquire about command hallucinations, higher rates are reported than in routine clinical assessments.
A substantial proportion of patients in our study reported compliance with command hallucinations to harm others, and patients who reported command hallucinations reported higher rates of violence than did other patients. The association between command hallucinations and violence held up even when the analysis controlled for demographic variables, substance abuse, and social desirability response sets. In our study group, both command hallucinations and other psychotic symptoms were associated with violence, but command hallucinations to harm others did not emerge as uniquely associated with violence when other positive psychotic symptoms were considered concurrently.
Previous research has suggested that patients are more likely to comply with command hallucinations if they are related to coexisting delusional beliefs (
26). Although our methods did not permit direct examination of this possibility, our results were consistent with the existence of common processes underlying the association between violence and both command hallucinations and other psychotic symptoms.
Some of the mixed results of previous research on command hallucinations and violence may have been due to vague definition of the predictor (for example, any command hallucinations versus none) rather than a specific focus on command hallucinations to harm others. In addition to the strength of the correlation between command hallucinations and violence we observed, it is in some respects self-evident that clinicians need to evaluate carefully the violence potential of any patient who reports such symptoms. If a patient reports that voices are giving commands to harm specific individuals, the patient's communication about such experiences may be on a continuum with threats. Consequently, a patient's report of command hallucinations to harm other people may prompt the clinician to consider various actions to protect the victims from the danger associated with the threatened violence (
27).
Our study emphasized symptoms rather than diagnoses as indicators of psychopathology, because research has suggested that acute symptoms are more specifically linked to violence than are diagnoses (
28). This relationship may be due to the fact that the course of many major mental disorders alternates between episodes of exacerbation and periods of remission. During periods of remission, the diagnosis may have little relationship with violence. When we conducted analyses that controlled for diagnosis, the associations between command hallucinations and violence held up.
In addition, patients' self-reports of command hallucinations have an interactional component that can be influenced by the context in which the patient is being assessed. Command hallucinations are subjective experiences and therefore may be particularly susceptible to inaccurate self-reporting because of motivational influences, such as the wish for hospital admission or discharge or for reduction in severity of criminal penalties. Our findings suggest that when the analysis controls for propensities toward a social desirability response bias—that is, a general tendency to endorse culturally approved behaviors—command hallucinations do correlate with violence. However, the clinician must still consider the context in which command hallucinations are being reported to estimate the self-report's veracity (
29).
One possible limitation of our study was its retrospective design. Future research with prospective designs would be helpful to evaluate the predictive significance of command hallucinations, although such research would be complicated by the fact that clinicians are obligated to treat such psychotic symptoms. To the extent that such treatment is effective, the apparent predictive significance of command hallucinations may be reduced.
Another possible limitation of our study was our use of questionnaires to measure violent behavior and symptoms. Self-reports, however, have increasingly been used as indicators of violent behavior in research (
2,
6,
30) and have yielded considerably higher rates of violence than institutional indicators such as arrest rates, possibly because violent psychiatric patients often are hospitalized instead of arrested. The MacArthur Community Violence Instrument was originally developed in an interview format. However, the finding that about half of the patients in our questionnaire study reported a recent history of violence is similar to the rates of violence found by others who used an interview-based format of this measure with recently discharged civil patients (
6,
31). In addition, psychometric research with the Conflict Tactics Scale, a widely used a predecessor of the MacArthur instrument, has demonstrated comparability of interview and questionnaire methods of administering items that assess violent behavior (
31,
32).
Although the PERI, a measure of psychotic symptoms, was developed as an interview-based instrument to allow assessment of symptoms in illiterate respondents (
33), all of our subjects demonstrated reading ability. Other research, such as that by Graham (
34) and by McNiel and others (
35), has shown questionnaire methods to be valid measures of symptoms in psychiatric patients, including in many with psychotic symptoms. It is conceivable that including items about violence and symptoms on questionnaires as opposed to interviews could have influenced the results. However, the consistency of our findings with expectations based on previous research and our inclusion of a measure of social desirability response bias likely attenuated this potential problem.