Samples
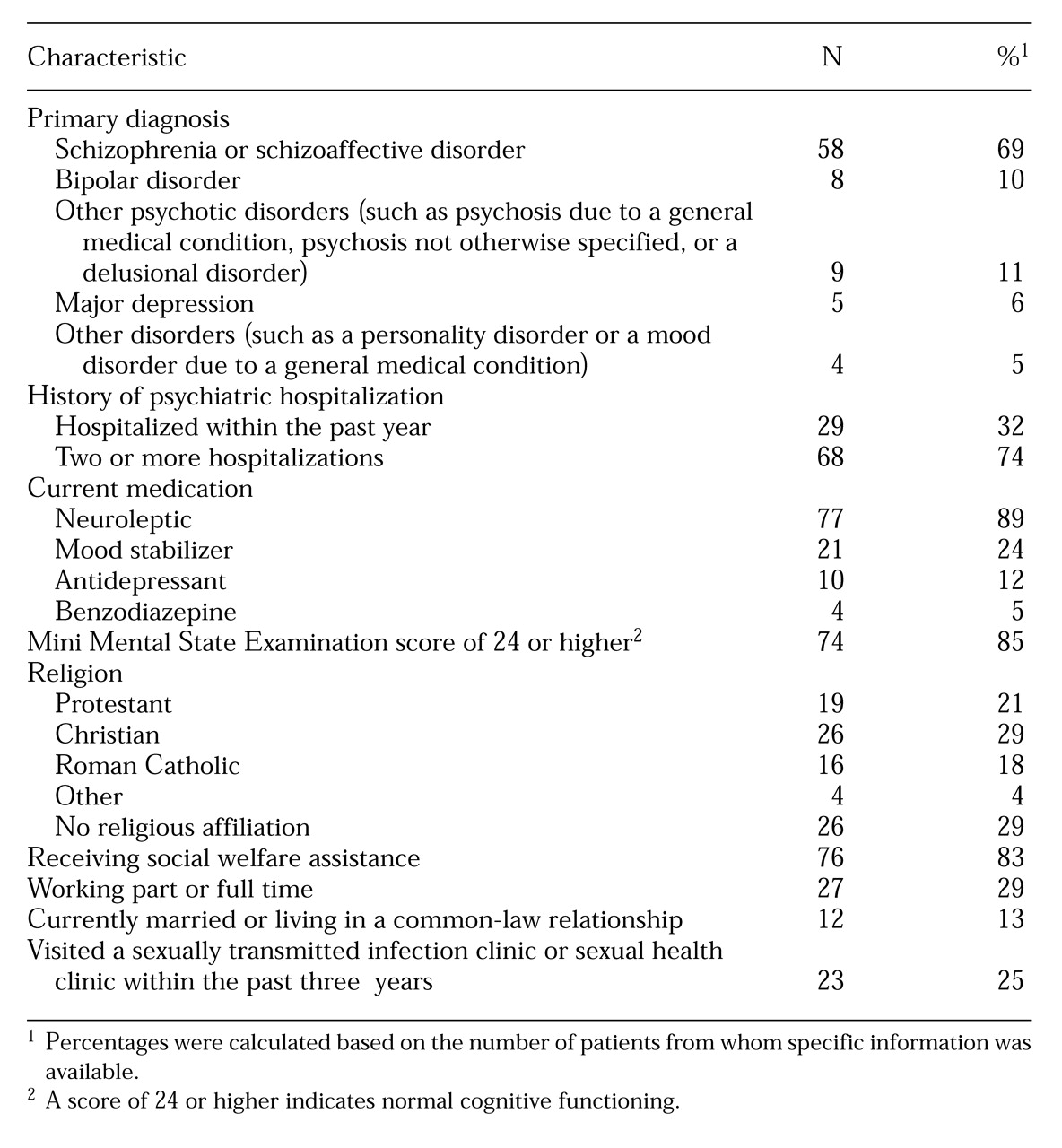
The mean±SD age of the patients was 35.6±8.2 years, and that of the comparison subjects was 35.3±8.2 years. The mean±SD duration of mental disorder was 12.9±8.8 years. Additional psychiatric and medical information for the patient group is provided in
Table 1. The most common psychiatric diagnoses, which were obtained by retrospective chart review and by consultation with the CMHC staff, were schizophrenia or schizoaffective disorders. Twelve patients (14 percent) were classified as having both an additional alcohol and drug abuse problem, five patients (6 percent) had an additional alcohol abuse problem only, and three (4 percent) had an additional drug abuse problem only.
The patients with mental disorders were compared with the comparison subjects on visits to a general practitioner or sexually transmitted infection clinic and on socioeconomic factors, including social welfare assistance, current employment, marital status, and education. Twenty-three patients with mental disorders (25 percent) had been to a sexually transmitted infection clinic at any time in the past, compared with 20 of the comparison subjects (22 percent), but the difference was not statistically significant. Sixty-one psychiatric patients (66 percent) and 78 comparison subjects (85 percent) had visited a general practitioner in the past year (χ2=6.70, df=1, p<.01).
Significantly more psychiatric patients than comparison subjects were receiving social welfare assistance (85 percent compared with 23 percent; χ2=70.3, df=1, p<.001), and fewer patients than comparison subjects were currently employed (29 percent compared with 75 percent; χ2=38.42, df=1, p<.001). Significantly fewer patients than comparison subjects were in a married or common-law relationship (13 percent compared with 66 percent; χ2=54.52, df=1, p<.001). The mean age at which patients completed schooling was 16.2 years, compared with 16.4 years for the comparison subjects. Only 14 patients had attended a technical college or university compared with 31 of the comparison subjects.
Within the previous year, 45 patients with mental disorders (49 percent) had heterosexual intercourse, and another four (4.3 percent) had homosexual contact. In contrast, 77 comparison subjects (84 percent) had engaged in heterosexual intercourse in the past year, and another subject had homosexual contact. The patients were significantly less likely than the comparison subjects to have been sexually active over the past year (χ2=21.38, df=1, p<.001).
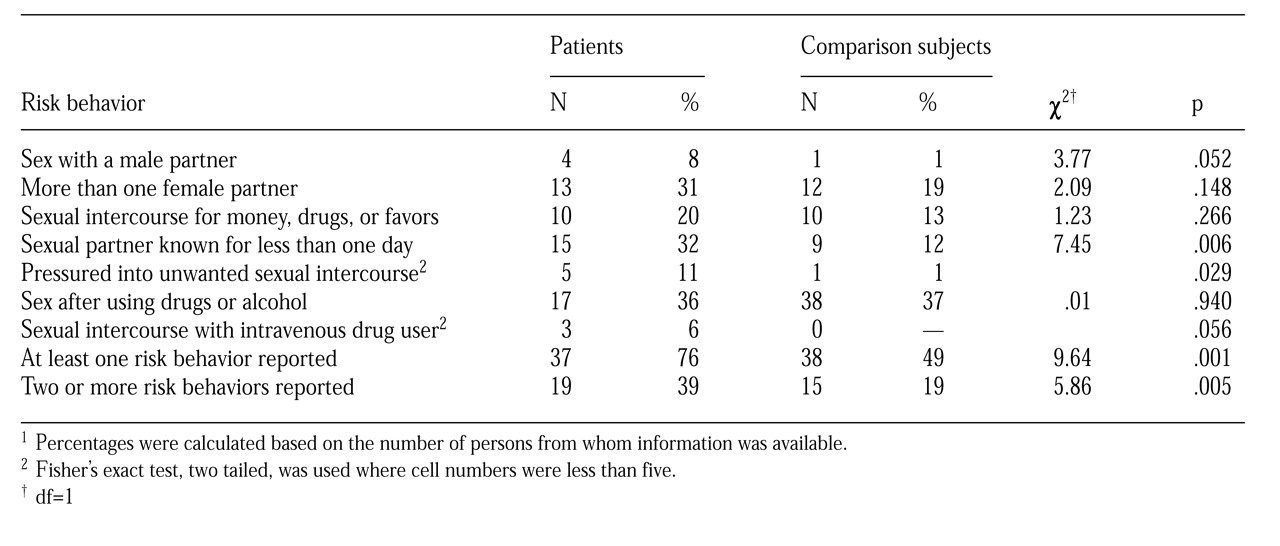
As shown in
Table 2, the 49 patients who were sexually active were significantly more likely than the 78 sexually active comparison subjects to have known their sexual partner for less than one day and to report having been pressured into unwanted sexual intercourse during the preceding year. A strong but not significant trend was found for patients with mental disorders to be more likely to have had sex with a male partner and to have had sex with a suspected or known intravenous drug user during the preceding year.
Furthermore, 11 patients, three of whom had shared needles, had injected themselves with drugs at some point in the past, including two patients within the past year. The three comparison subjects who had injected themselves with drugs had all done so more than a year ago. Three-quarters (76 percent) of the sexually active patients reported at least one of the risk factors listed in
Table 2, compared with 49 percent of the comparison subjects (χ
2=9.64, df=1, p=.001).
One homosexual psychiatric patient who said he was HIV positive had receptive anal intercourse during the past year, although he reported using condoms on every occasion of intercourse. Another homosexual patient reported having had sex with a male whom he knew had AIDS but denied engaging in anal intercourse. He also had not been tested for the AIDS virus. Two other patients, one of whom had 12 male partners in the past year, denied having anal intercourse.
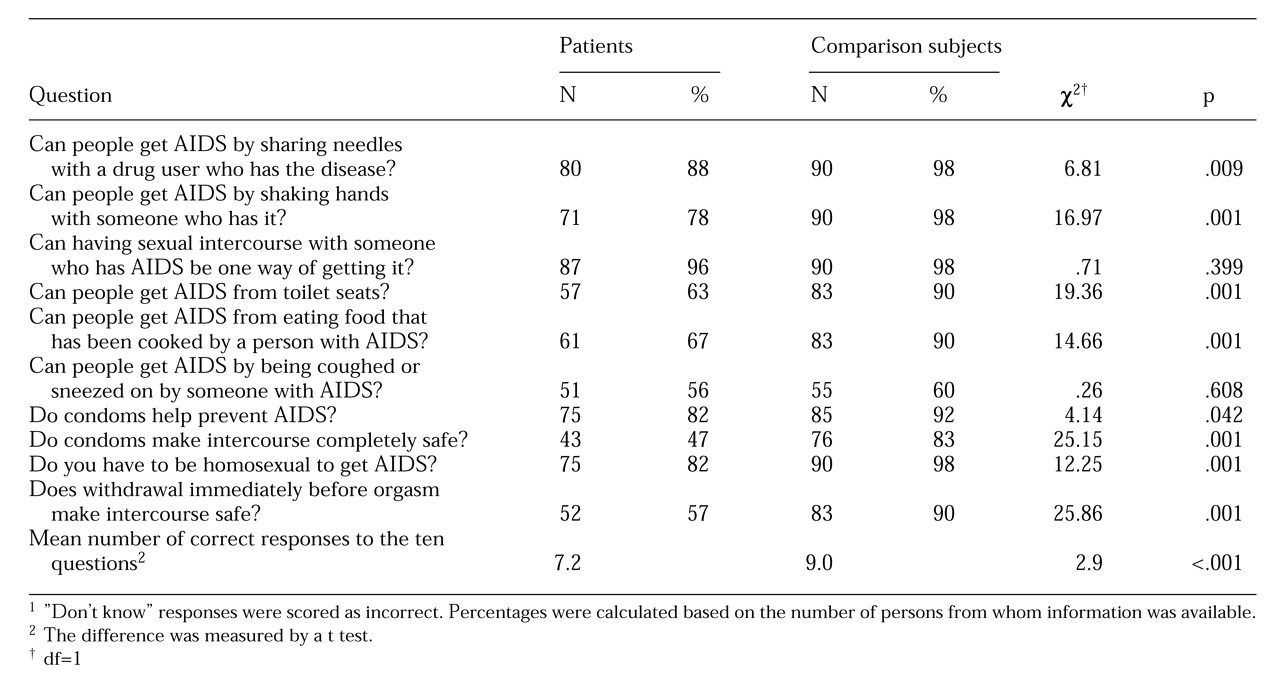
Table 3 shows the percentages of patients with mental disorders and comparison subjects who gave correct responses to ten questions about AIDS. For seven of the ten questions, the patients with mental disorders scored significantly lower than the comparison subjects. The patients scored significantly fewer mean correct answers than the comparison subjects.
Patients with mental disorders and comparison subjects were asked whether they had ever had a sexually transmitted infection. Only one patient reported being HIV positive. Eighteen patients said that they had had gonorrhea, compared with eight comparison subjects (χ2=5, df=1, p=.025). Five patients reported having had syphilis, compared with none of the comparison subjects (p=.027, Fisher's exact test, two tailed). Eight persons in each group reported having had chlamydia. Five patients reported genital herpes, compared with 12 comparison subjects, but the difference was not significant. When asked about current symptoms, two patients reported discharge from the penis, pain passing water, and itching in the genital region, indications of current infection. None of the comparison subjects reported such symptoms.
Twenty-six of the 92 patients with mental disorders (28 percent) said that they had talked to a doctor or nurse about AIDS. Of the 35 patients who were sexually active within the past year and had a least one risk factor for a sexually transmitted infection, 13 (37 percent) had at some time talked to a doctor or nurse about AIDS.