First Surgeon General's Report on Mental Health Stresses Effectiveness of Treatment, Notes Many Fail to Seek Help
The first U.S. Surgeon General's report on mental health, released last December, emphasizes that mental health care is effective and that a range of treatments exist for most disorders. But it points out that nearly half of all Americans who have a severe mental illness do not seek treatment, in many cases because of the stigma society has attached to mental illness.
The 487-page report is the product of more than two years' work by staff of the Center for Mental Health Services and the National Institute of Mental Health as well as almost 200 mental health providers, consumers, consultants, and other contributors. Directed to the general public, it summarizes major findings from a review of more than 3,000 research articles in the scientific literature.
The report presents data from epidemiological surveys indicating that about 20 percent of the U.S. population are affected by mental disorders during a given year. Among the adult population age 18 to 54, an estimated 22 to 23 percent, or 44 million people, have a diagnosable mental disorder, while 3 percent have both mental and addictive disorders, and 6 percent have addictive disorders alone. These data indicate that within a one-year period, from 28 to 30 percent of the population has either a mental or an addictive disorder.
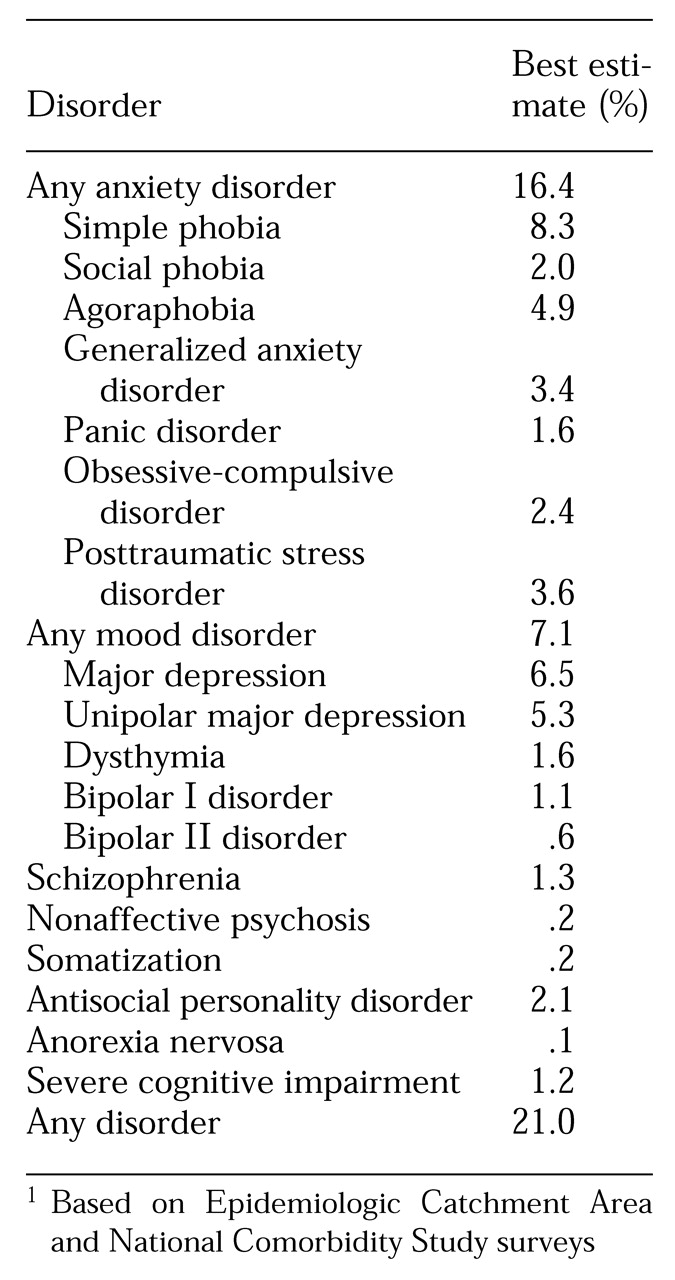
Table 1 shows the best estimate of prevalence rates for specific mental disorders, based on data from the Epidemiologic Catchment Area surveys and the National Comorbidity Study.
About 20 percent of children between age nine and 17 are estimated to have mental disorders with at least mild functional impairment. From 5 to 9 percent have a serious emotional disturbance, defined as a diagnosable mental health problem that severely disrupts their ability to function socially, academically, and emotionally.
Among adults ages 55 years and older, almost 20 percent have a diagnosable mental disorder during a one-year period. Almost 4 percent have a serious mental illness, and just under 1 percent have a severe and persistent mental illness.
The report states that a range of treatments of proven efficacy are available for most mental disorders. Most treatments fall under two general categories, psychosocial and pharmacological. A combination of the two can sometimes be more effective than each individually.
Data on the mental health treatment system show that only about 6 percent of the adult population and about 8 percent of children and adolescents are treated in the specialty mental health sector, which includes mental health professionals such as psychiatrists, psychologists, psychiatric nurses, and psychiatric social workers. Another 6 percent of the adult population and 3 percent of children and adolescents use the general medical sector, which consists of health care professionals such as internists, pediatricians, and nurse practitioners.
About 5 percent of adults and 3 percent of children receive mental health services in the human services sector, which consists of social services, school-based counseling, residential rehabilitation services, vocational rehabilitation, and criminal justice and prison-based services. Voluntary support networks, consisting of self-help groups such as 12-step programs and peer counselors, are a rapidly growing component of treatment for mental and addictive disorders, used by about 3 percent of the adult population.
In 1996 the U.S. spent $69 billion for diagnosis and treatment of mental illness, of which 53 percent, or $37 billion, was paid by public funds and 47 percent, or $32 billion, was paid by private sources. Between 1986 and 1996, mental health expenditures increased at an average annual rate of more than 7 percent. Overall, the annual growth rate in the public sector during that period was slightly more than 8 percent, while the annual increase in the private sector was little more than 6 percent.
Of the $69 billion spent in 1996 for diagnosis and treatment, more than 70 percent was for the services of specialty providers, with most of the remainder for general medical services providers. Multiservice mental health centers received 18 percent of the funding, psychiatric hospitals 17 percent, psychiatric units in general medical hospitals 10 percent, and general medical hospitals 6 percent. By discipline, 14 percent of the expenditures went to psychologists and social workers, 10 percent to psychiatrists, and 5 percent to general medical physicians.
The indirect costs of all mental illness was $79 billion in 1990, the most recent year for which estimates are available. Most of that amount—$63 billion—reflects morbidity costs, or the loss of productivity in usual activities because of mental illness. But mortality costs—lost productivity due to premature death—reached almost $12 billion in 1990. Almost $4 billion was attributed to productivity losses for incarcerated individuals and for the time spent by individuals providing family care.
Based on findings of the efficacy of treatments for mental illnesses and the range of treatments available, the report makes a single, explicit recommendation: persons who have a mental health problem or think they have symptoms of a mental disorder should seek treatment. But it notes that if this recommendation is to be followed, society must resolve to dismantle significant barriers to seeking help.
The report describes several courses of action designed to help lower barriers to treatment, including continuing to build the science base to provide new opportunities for treatment; overcoming stigma; improving public awareness of effective treatments; ensuring the supply of mental health services and providers; ensuring delivery of state-of-the-art treatments; tailoring treatment to age, gender, race, and culture; facilitating entry into treatment; and reducing financial barriers to treatment.
The report, entitled Mental Health: A Report of the Surgeon General, is available on the World Wide Web at http://www.surgeongeneral.gov. It also may be ordered from the Government Printing Office for $51 per copy; phone, 202-512-1800; fax, 202-512-2250.
NAMI Review Finds Only a Third of NIMH Funding Goes to Support Research on Severe Mental Illnesses
The National Alliance for the Mentally Ill (NAMI) charged that the National Institute of Mental Health (NIMH) has failed in its primary mission to support research on severe mental illnesses after a NAMI analysis showed that only about a third of NIMH research funds supported such research. NAMI recommends that severe mental illnesses receive at least two-thirds of NIMH's research resources in any given year.
The analysis, released in December 1999, was based on a review of abstracts of 2,277 research grants awarded by NIMH in fiscal year 1997. Each abstract was read by two members of a five-person professional review committee, who independently rated the abstracts on whether the research was related to any disease. For 248 abstracts, the information was insufficient to permit categorization, leaving a total of 2,029.
The committee members found that 1,049 grants were disease related and 980 were not disease related. The disease-related grants accounted for $278.3 million dollars, or 66 percent of the total NIMH research budget represented in the rating process. However, when the research grants were assigned to specific disease categories, just over half, representing 36 percent of the total NIMH research budget, were targeted to research on severe mental illnesses.
The analysis showed that 18.2 percent of the total NIMH grant fundsrated were directed to research on major depression, 13.5 percent to schizophrenia, 5.2 percent to manic-depressive illness, 3.6 percent to panic disorder, and 2.1 percent to obsessive-compulsive disorder. A total of 279 grants were funded on major depression, 235 on schizophrenia, 71 on manic-depressive illness, 58 on panic disorder, and 30 on obsessive-compulsive disorder.
When the research grants were assigned to the single disease category they primarily targeted, only 589 grants, or 29 percent of the total, were found to be directed to one or more severe mental illnesses. Further analysis showed that only 161 of the 589 grants were targeted toward research on clinical and treatment issues, representing only 11.9 percent of NIMH grant funds. Ninety-four were targeted to major depression, 27 to schizophrenia, 17 to manic-depressive illness, 12 to panic disorder, and 11 to obsessive-compulsive disorder.
The analysis also showed that at least 15 percent of NIMH research funds supported research on diseases that are the primary responsibility of other institutes within the National Institutes of Health. Funds for research on AIDS constituted 14.2 percent of all NIMH research funds in 1997, a higher percentage than that allocated for all research on schizophrenia and almost three times higher than that for manic-depressive illness. Research on Alzheimer's disease received 3.6 percent of NIMH research funds, similar to the amount allocated for panic disorder. Other NIMH research funds went to support research on Parkinson's disease, spinal cord injury, multiple sclerosis, breast cancer, diabetes, heart disease, and other illnesses.
The 980 research grants for basic research unrelated to any disease were valued at $144.2 million and constituted 34 percent of NIMH's total research funds in 1997. The NAMI analysis estimated that $96.1 million of these funds were used to support basic behavioral or social science studies. Another $181.6 million in NIMH research funds were used to support basic neuroscience research. In both cases, the analysis pointed out that such expenditures represented a substantial portion of the NIMH research budget and supported research that is primarily the responsibility of other agencies.
The recommendation that severe mental illnesses receive at least two-thirds of NIMH's research resources in any given year was the first of several resulting from the analysis. NAMI also recommended that investment in research on manic-depressive illness and obsessive-compulsive disorder be tripled in the next two years.
In addition, NAMI called on NIMH to markedly increase its investment in clinical and treatment-related research on severe mental illnesses and to stop allocating its scarce resources to diseases that are the primary responsibility of other NIH institutes. It said that behavioral research on diseases should be an integral part of all NIH institutes, and that behavioral research funded by NIMH should focus on severe mental illnesses and other neuropsychiatric diseases. Basic neuroscience research should have a more modest role at NIMH.
NAMI said that congressional hearings to clarify the primary mission of NIMH would be useful. It also said that NIMH should be required to issue an annual report to Congress on the allocation of its resources.
Members of the professional review committee who rated the grants for NAMI were E. Fuller Torrey, M.D., and Michael B. Knable, D.O., of the Stanley Foundation Research Programs in Bethesda, Maryland; John M. Davis, M.D., of the department of psychiatry at the University of Illinois at Chicago College of Medicine; Irving I. Gottesman, Ph.D., of the department of psychology at the University of Virginia School of Medicine in Charlottesville; and NAMI executive director Laurie M. Flynn.
The report, entitled The Failure of the National Institute of Mental Health to Do Sufficient Research on Severe Mental Illnesses is available on the Internet at www.nami.org.
DAWN Data Indicate Emergency Drug Visits Remained Stable in 1998
Data from the Drug Abuse Warning Network (DAWN) show that an estimated 542,544 drug-related visits were made to hospital emergency departments in 1998, about 3 percent more than in 1997, a statistically insignificant increase.
DAWN is a national probability survey of hospitals with emergency departments that is conducted annually by the Substance Abuse and Mental Health Services Administration (SAMHSA). A total of 471 hospitals in 21 metropolitan areas and other locations outside those areas participated in the study in 1998. Data for 1998 were released in late December.
Analysis of the data showed that total drug-related emergency department visits were stable across gender, race and ethnicity, and most age subgroups between 1996 and 1998. However, emergency department visits among 12- to 17-year-olds declined by 8 percent, to 59,086, from a peak of 63,949 in 1996. Total emergency room episodes involving patients age 35 and older increased by 14 percent between 1996 and 1998, from 210,105 to 239,172.
Among the drugs most frequently mentioned in 1998, cocaine was reported in 172,014 emergency department visits compared with 152,443 in 1996, an increase of 13 percent. Visits involving heroin or morphine totaled 77,645 in 1998 compared with 73,846 in 1997, a 5 percent increase. Visits involving marijuana or hashish increased 43 percent, from 53,789 in 1996 to 76,870 in 1998.
In 1998 suicide, involving 189,897 emergency department visits, and drug dependence, involving 189,094 visits, were the most frequently cited motives for taking substances. Overdose, accounting for 245,164 visits, was the most frequently cited reason for coming to the emergency department. Between 1997 and 1998, the number of episodes of patients citing withdrawal as the reason for the visits increased by 18 percent, from 15,176 to 17,979.
Among the 21 metropolitan areas covered by DAWN, only Dallas had a significant increase in overall drug-related emergency department episodes. They rose from 6,195 in 1997 to 7,198 in 1998, a 16 percent increase.
Along with data from the DAWN survey, SAMHSA also released 1997 information on drug-induced or drug-related deaths reported by medical examiners and coroners who voluntarily participated in the DAWN survey. A total of 145 medical examiner facilities in 42 metropolitan areas reported 9,616 drug-related deaths in 1997, up 2 percent from the 9,410 deaths reported in 1996. Cocaine was the most frequently mentioned drug, followed by heroin-morphine. Between 1996 and 1997, deaths involving methamphetamine-speed increased by 28 percent, and deaths involving PCP by 15 percent. Because the medical examiners were voluntary participants, counts of drug-related deaths were not representative of the nation as a whole.
The report is accessible on the Internet at http://www.samhsa.gov/media.htm.
News Briefs
Sertraline approved for PSTD: Sertraline hydrochloride has become the first drug to be approved by the U.S. Food and Drug Administration (FDA) for the treatment of posttraumatic stress disorder. A selective serotonin reuptake inhibitor introduced in 1992, sertraline was developed by Pfizer and is marketed under the trade name Zoloft. It previously had been approved by FDA for the treatment of major depression, panic disorder, and obsessive-compulsive disorder.
Grants for research on anxiety disorders: The Anxiety Disorders Association of America (ADAA) has established new junior faculty research grants that are intended to increase the pool of independent investigators with interest and expertise in research on anxiety disorders. Two awards will be offered annually, each with a possible second-year continuance. Each will provide partial salary support totaling $39,000 a year. Grant applications may cover a broad range of topics but must be relevant to ADAA's mission to promote the prevention, treatment, and cure of anxiety disorders. Information about eligibility requirements and copies of application forms can be found on the ADAA Web site at www.adaa.org or obtained by calling 301-231-9259, ext. 299. Deadline for applications is March 1, 2000.