Health care has ceased to be the exclusive concern of individual physicians and individual patients for some time. The large majority of privately insured individuals now receive behavioral health services through managed systems of care in which decisions about the type and amount of treatment are influenced by factors other than patients' and providers' wishes (
1). The effects of managed behavioral health organizations on decisions about the medical necessity of mental health treatment are at the heart of legal and ethical criticism of the managed behavioral health industry (
2,
3,
4).
Critics charge that managed systems attempt to reduce expenditures by denying payment for medically necessary care. Evidence for these concerns comes from two sources. One source is an inference drawn from the very evidence that has driven growth in the managed behavioral health industry: demonstrations of large economic savings from managed behavioral health care (
5,
6,
7,
8,
9,
10). Economic evaluations alone do not support or refute concerns that a particular managed behavioral health organization adversely affects treatment by not paying for needed mental health services. Some studies demonstrate that in managed systems of care overall access to mental health services remains stable or increases, while savings are produced or maintained for the health care purchaser (
5,
6). Savings may result from other changes brought about by managed care, such as use of a specialized network of providers, shifts of care from inpatient to lower-intensity settings, and discounted fees schedules.
Another source of concern is providers' and patients' negative experiences with managed behavioral health organizations that are reported in the media, in legislative hearings, and in professional journals (
11,
12,
13) The American Psychological Association and others have opposed utilization review, particularly for outpatient treatment, on the grounds that management is unlikely to affect the length of treatment, which is typically brief and inexpensive (
14). For example, one study found that the cost of treating depression was only 8 percent of the mental health premium (
15). Others have noted the joint influence of highly publicized "atrocity incidents" and the erosion of public trust in medical care (
16,
17).
Despite the intensity of the debate, no systematic analyses have examined the extent to which patients and providers agree with the utilization review decisions of managed behavioral health organizations. This study reports on a brief survey of patients' and providers' perceptions of why outpatient treatment ended in a large national managed behavioral health organization. The survey allowed us to address three questions: What are the most common reasons cited by patients and providers about why outpatient treatment terminates? To what extent do patients and providers agree about reasons for termination? To what extent is the reason for termination related to the patient's perceived satisfaction with the therapist and the outcome of treatment?
Methods
Sample
A sample of 386 patients were randomly selected from the population of outpatient psychotherapy users ending treatment in United Behavioral Health (UBH), a large managed behavioral health organization. UBH, formerly U.S. Behavioral Health, is a carve-out organization that manages mental health and substance abuse benefits through direct contracts with self-insured employers. Patients enter treatment by calling an 800 intake line and obtaining a referral and initial authorization, usually for ten sessions of treatment. Treatment is reviewed at periodic intervals by licensed mental health professionals to evaluate the appropriateness and necessity of ongoing treatment.
Patients were contacted to participate in the study if their treatment involved an outpatient psychotherapy procedure code. To be included in the study, patients had to be over 17 years old, to have completed outpatient treatment with a network provider between January 22 and March 11, 1998, and to agree to be contacted by mail or telephone.
Patient survey
Data were taken from a questionnaire that is routinely used by UBH to assess patient satisfaction. The questionnaire asks three questions each about improvement in therapy and satisfaction with the therapist, and one question about overall satisfaction with treatment. Questions are answered on Likert-type scales ranging from 1, strongly disagree, to 5, strongly agree. Questions about therapy ask about improvement over the course of therapy in the patient and in his or her relationships and work or school functioning. Questions about the therapist ask whether the therapist listened to the patient and treated the patient respectfully.
A principal components analysis of the seven items yielded a single factor accounting for 68 percent of the item variances. All factor loadings exceeded .75. A satisfaction scale was constructed by summing the seven items and showed good internal consistency (alpha=.91).
A second set of questions in the survey asked patients to indicate the primary reason treatment ended. Patients were presented with nine choices, including "other," that paralleled those given to providers. Most often "other" responses could be classified according to one of the other eight reasons. For example, a response such as "a family member died" was recoded as "I discontinued treatment on my own." Thirty-five responses were reclassified in this way. In the remaining cases, respondents specified the "other" category and left the response line blank or stated that they returned to treatment. One respondent stated that treatment ended because the respondent had gone to jail.
Provider survey
Providers' perceptions of reasons for termination were obtained from closing reports submitted at the end of treatment using the same categories as for patients. Providers have a routinely high rate of compliance in supplying information for this database, and only five cases were dropped because the provider did not complete the section on reasons for termination.
Procedures
The initial survey was mailed to 386 patients with a personalized cover letter and self-addressed stamped return envelope. The 386 patients were randomly assigned to one of four follow-up procedures: phone follow-up, letter and phone follow-up, no follow-up, or no follow-up but a dollar bill in the initial mailing. A secondary purpose of the study was to determine whether different follow-up procedures would increase response rates. Each cohort had a sample of about 100 patients. Patients were eliminated if the initial mailing was returned because of an incorrect address.
Statistical analyses
Analyses computed the frequency and percentage of self-reported reasons for termination. Kappa coefficients were conducted to compare agreement between patients' and providers' responses. Kappa coefficients measured the degree of concordance between patient and providers, correcting for chance agreement (
18). T tests were used to examine the relationship between reasons for termination and patients' satisfaction ratings. All analyses were performed using SAS statistical software.
Results
Sample characteristics
A total of 190 patients responded to the survey, for a response rate of 49.2 percent. A comparison of respondents and nonrespondents showed that respondents were slightly older; however, the two groups were comparable in gender distribution. Most of the 190 respondents were female (139 patients, or 73.2 percent). The mean±SD age of the sample was 48.97±6.92 years. Data on race-ethnicity were not obtained.
Respondents' most common diagnoses were adjustment disorder (95 patients, or 50 percent) and major depression (92 patients, or 48.4 percent). Smaller proportions of patients had anxiety disorders (38 patients, or 20 percent) and personality disorders (19 patients, or 10 percent). Some patients had more than one diagnosis. In the year before the survey, the mean±SD number of outpatient visits for the sample was 8.1±5.4. More than half of the sample (109 patients, or 57.4 percent) had six or more visits.
Response rates varied significantly among the follow-up cohorts. The rates for each cohort were 56.3 percent (N=46) for phone reminders, 74.2 percent (N=69) for letter and phone reminders, 36.2 percent (N=45) for no letter or phone reminders, and 39 percent (N=30) for no letter or phone reminders but with a dollar bill in the initial mailing. No significant response biases were found between cohorts in improvement ratings, satisfaction with the therapist, and reasons for termination.
The sample was seen by 190 providers, of whom 96, or 50.5 percent, were doctoral-level psychologists; 89, or 46.8 percent, were social workers; and five, or 2.6 percent, were psychiatrists. No differences in the provider's reason for termination were found by provider type.
The mental health benefits of the sample were generous, although typical of the growing number of employers who expand benefits and simultaneously adopt managed behavioral health care. Most patients had no annual limits on outpatient visits. The minimum benefit was 40 sessions annually. The modal copayment for outpatient treatment was $15, with a range from $10 to $30. Inpatient benefits were equally generous, with all patients having an unlimited benefit. Inpatient coinsurance was 90 percent, with a range of $100 per admission to 100 percent coinsurance.
Patients' perceptions
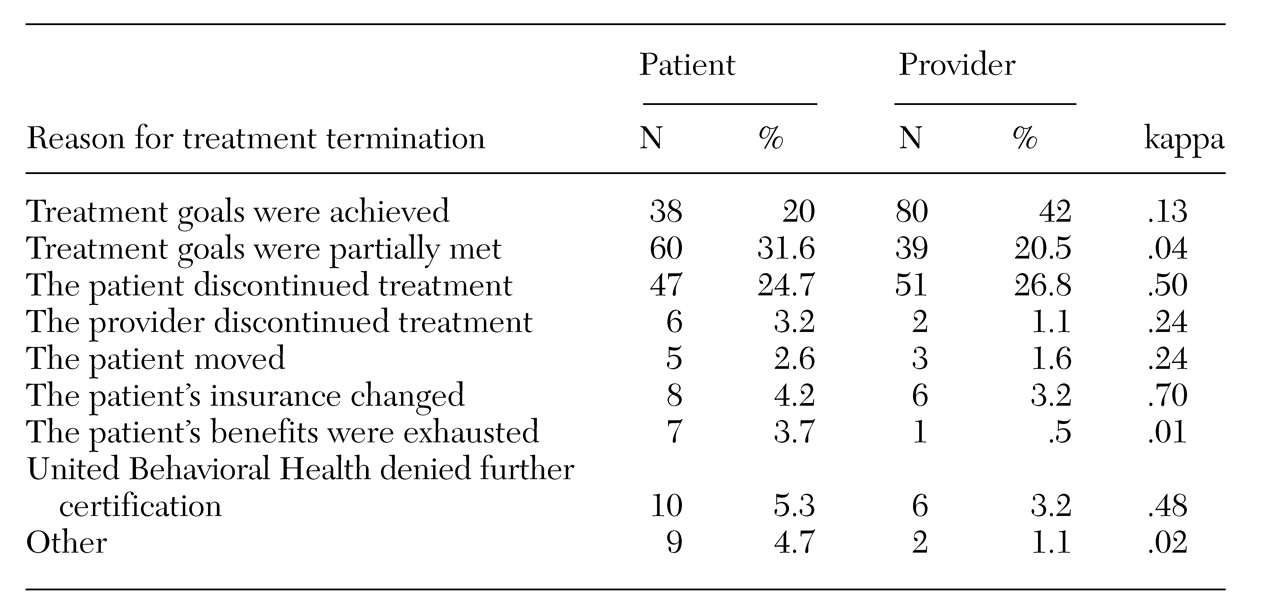
As shown in
Table 1, among patients the leading reason for termination was that treatment goals were partially or completely met. Patients stated that their own decisions resulted in the end of outpatient treatment in the vast majority of cases (150 cases, or 78.9 percent).
A small percentage of patients reported that outpatient episodes ended because of limits placed on treatment by the managed behavioral health organization or by the employer's benefit design. Seven patients reported that treatment ended because an annual or lifetime limit on their benefits had been reached. To verify the reason for termination in these seven cases, patients' self-reports were compared with administrative records kept by UBH. None of the seven patients had maximized their mental health benefits, and all were still eligible for outpatient treatment at the time of termination.
Just as uncommon were patients' reports that UBH had not authorized continued treatment. Ten patients cited this reason, but in only one of these cases did administrative records show that a formal decision was made disallowing payment by UBH for further treatment. In one case the provider initiated termination. In three cases the provider did not request additional sessions, and medical necessity was never questioned by the care manager, suggesting that termination was initiated by the provider. In three other cases, the care manager recommended that treatment be concluded, and the provider agreed (or acquiesced) with the recommendation. In two cases, the care manager's approval for continued treatment depended on additional clinical information that was never received from the provider.
Providers' perceptions
As
Table 1 shows, the distribution of providers' reasons for termination was comparable to that of patients. The leading reasons for treatment termination were patient-related decisions (173 cases, or 91.1 percent). Benefit exhaustion was mentioned by only one provider as a reason for termination, but administrative records indicated that the patient had not exhausted the benefits.
Six providers mentioned that treatment ended because payment was not authorized by UBH due to lack of medical necessity. Administrative data showed that only one provider received notification of a formal decision not authorizing ongoing treatment. In two cases, the care manager recommended that treatment end, and the provider agreed (or acquiesced) with the recommendation. In the remaining three cases examined, no evidence was found of discussion between providers and care managers about medical necessity or the length of treatment.
Congruence of responses
Although the distributions of patients' and providers' survey responses about reasons for termination were very similar, little agreement was noted for given individuals. The rate of agreement was only partly improved by combining the categories about treatment goals being fully and being partially met (kappa=.38). Agreement was good for some reasons: change of insurance (kappa=.70), patient discontinued (kappa=.50), and UBH denied further certification (kappa=.48). Patients and providers showed poor agreement on all other reasons for termination, including whether treatment goals had been met or partially met. The coefficients of agreement between patients and providers are presented in
Table 1.
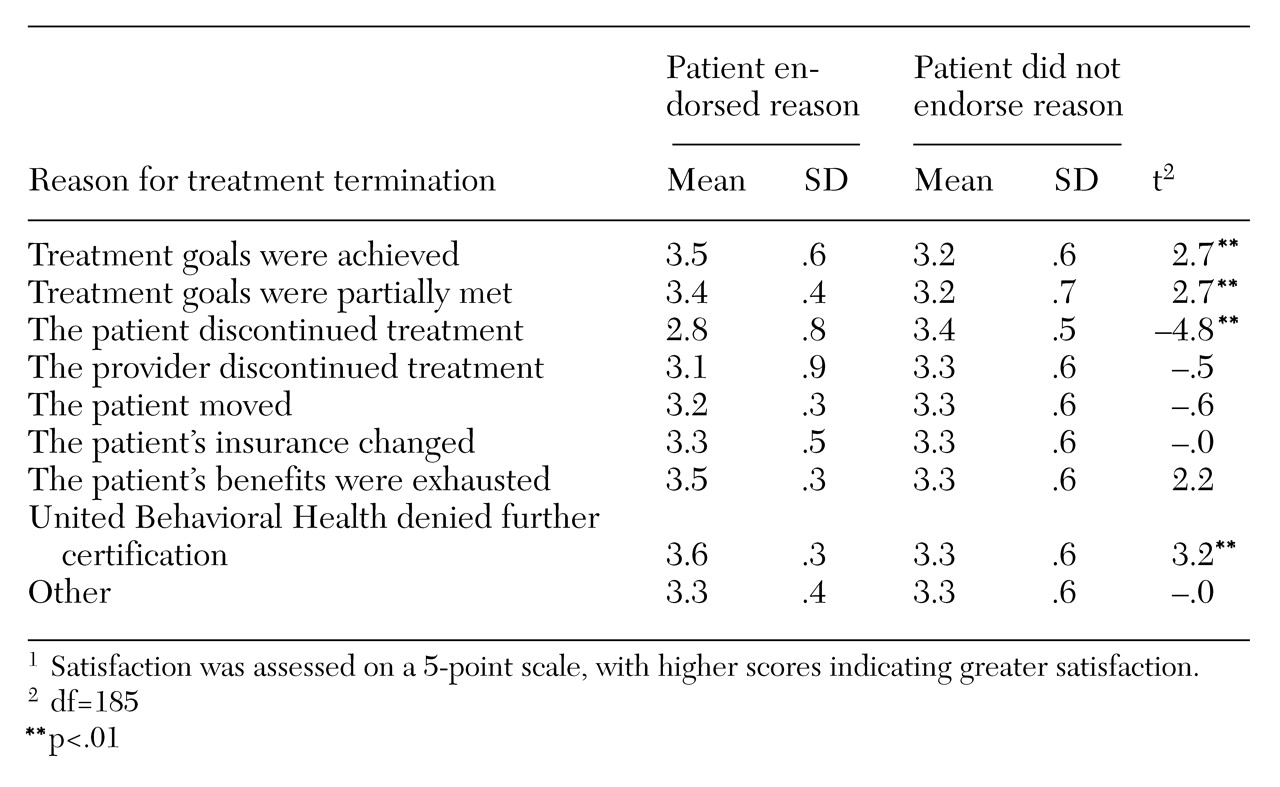
Reason for termination and satisfaction
The final set of analyses tested the relationship between reasons for termination and patients' satisfaction ratings. The results are presented in
Table 2. Patients were more satisfied when they perceived that they had partially or completely achieved their treatment goals than when they terminated for other reasons. Lower satisfaction was noted when patients reported discontinuing treatment on their own. Unexpectedly, patient satisfaction was positively associated with treatment ending due to lack of medical necessity. Patients who cited treatment ending because payment was denied reported being more satisfied with therapy and their therapist.
Discussion
This study suggests that outpatient mental health treatment is most likely to end when patients have partly or completely met their treatment goals. A small percentage of patients and providers cited benefit limitations or utilization review decisions as the cause of termination; however, many of these perceptions were incongruent with administrative records of the managed behavioral health organization.
The results of this study of one cohort from a large managed behavioral health organization challenge the notion that utilization review decisions are greatly at odds with those made by patients and providers. The results are consistent with some previous research findings suggesting that the duration of outpatient treatment in a managed behavioral health organization, also UBH, corresponds to expert consensus about the length of outpatient treatment for major depression (
19). Similarly, results are consistent with those of Howard and associates (
20) on dose-response in psychotherapy, which suggests that patients often report benefits very early in treatment—within six to eight sessions.
The finding that few patients exhausted their benefits is consistent with research suggesting that expansion of outpatient benefits would not dramatically affect costs in organized care systems (
21). This speculation was further reinforced by a review of administrative records that found that none of the survey respondents exhausted their benefits even though some reported doing so. Several issues are raised by this finding. Patients may not understand their mental health benefits or may receive incorrect information about their benefits from their employer, their managed behavioral health organization, providers, or family and friends. One of the most important roles of the formal care system, including managed behavioral health care, is educating patients about their benefits. A typical managed behavioral health organization may manage thousands of benefit designs, and miscommunications between patients, providers, and managed behavioral health organizations may result in premature termination from treatment (
22).
The survey also found that some patients incorrectly attribute treatment termination to decisions made by the managed behavioral health organization. Beliefs about termination are likely to stem from communications between patients, providers, and managed behavioral health organizations during the course of treatment. Inaccurate and unclarified communications may result in the kinds of results observed in this survey.
Empirical data collected in this study do not offer a direct explanation for the fact that the majority of providers who reported denials of coverage did not formally request additional sessions or even informally discuss the need for ongoing treatment with care managers. Anecdotal experience, however, suggests some contributing factors. First, complaints about the paperwork required by managed behavioral health organizations suggest that some providers may not request ongoing treatment because they are discouraged by the perceived "hassle factor" or by the administrative costs to them of utilization review. In effect, providers may buy reductions in administrative time by not completing paperwork or not submitting information to the managed behavioral health organization to continue treatment.
Managed behavioral health organizations must recognize the burdens of paperwork related to utilization review in terms of the costs to providers and their motivation to deliver treatment. Solutions such as less frequent reviews and electronic or telephonic submission of review information require managed behavioral health organizations and providers to invest in an infrastructure.
Second, experience suggests that in some cases providers do not request ongoing treatment because they do not believe that it will be approved. Some discussions with care managers may leave providers with the impression that ongoing treatment would not be authorized due to limited benefits or restrictive policies, or both, and that a care manager's request for additional information or a preliminary recommendation regarding length of treatment is a formal denial.
Compounding the problem is that providers may not be familiar with the varied processes necessary to obtain payment for ongoing treatment from different managed behavioral health organizations. Providers find that navigating the maze of a large managed behavioral health organization can be difficult. The majority of providers know that most requests for outpatient treatment are approved by certain organizations.
Still another dynamic may be operating. A decade ago many providers would treat a patient to the limits of the patient's benefit. For example, they would hospitalize the patient for a 30-day stay corresponding to a 30-day inpatient benefit. Currently, some providers may treat to the imagined limit of the initial outpatient authorization. The imagined limit may derive from the hope of pleasing the referral source through misplaced overcompliance with the initial authorization. Others have suggested that providers may avoid advocating for patients out of dislike of the utilization review process (
16).
Regardless of the underlying factors, attribution for responsibility for treatment termination is shifted to the managed behavioral health organization. Another finding of this survey underscores the idea that reasons for terminating outpatient treatment are not tied to administrative realities as much as to the subjective impressions of patients and providers. In this study, patients' and providers' reasons for termination did not agree beyond chance levels except for when treatment ended because of a utilization review decision. In such cases, patients reported higher levels of satisfaction with therapy and their therapist, raising the possibility that a shared perception of culpability of the managed behavioral health organization may strengthen the bond between patient and therapist. Attributions about termination appear to be communicated and shared between patients and providers, but they may not be based on the actual utilization review decisions made by managed behavioral health organizations.
Conclusions
The overall findings of this survey are encouraging and suggest that the majority of outpatient treatment is terminated because of patients' and providers' decisions. However, the survey findings should be understood in the context of some methodological limitations attributable to the survey design. Most notably, the response rate was approximately 50 percent, raising the possibility of response bias. Although results from the experimental manipulation of response rates do not suggest such a bias, we cannot rule out the possibility.
Second, providers' responses may have been biased by the knowledge that their responses were directed to an important referral source, which may have led them to more favorable portrayals of termination. These results require replication by other investigators with no ties to managed behavioral health care organizations, and studies must include samples from multiple systems of care.
More research needs to examine the conditions that facilitate or hinder providers from acting on behalf of patients during the utilization management process (
17). Conditions that may hinder providers include complex and burdensome procedures for requesting treatment and risk-sharing arrangements between providers and managed behavioral health organizations. Risk-sharing arrangements such as subcapitation and case rates, although not used by UBH, may remove providers' incentives to act as patient advocates.