The State Comprehensive Mental Health Services Plan Act of 1986 (Public Law 99–660) supported development and implementation of community-based case management programs to address treatment needs of severely mentally ill adults (
1). Case management programs have since proliferated. Although programs share the primary goals of identifying clients' needs and coordinating services for comprehensive care, they often differ in how they provide services, the services they provide, and the duration of care.
Provision of case management to adults with serious mental illness is complicated by the prevalence of substance use problems. Co-occurring substance use disorders have been consistently associated with negative outcomes, including the failure of clinicians to provide correct diagnoses (
2), exacerbation of psychotic symptoms (
3), and noncompliance with medication (
4). Among adults with serious mental illness, those who are substance dependent are usually hospitalized more often than those who are not (
5,
6), and they make fewer visits to alcohol and drug outpatient clinics (
7). They may have less access to aftercare services (
8) and a greater reliance on acute services, such as emergency room treatment and hospital and jail services (
5,
7,
9).
This article presents six-month outcomes of a randomized trial that compared the relative effectiveness of two case management service delivery models—intensive clinical case management and expanded brokerage case management—for substance-dependent and nondependent adults with serious mental illness. The programs used assertive case management and shared the goals of enabling clients to be maintained in community treatment settings, reducing the number and length of psychiatric hospitalizations, and improving quality of life. They differed in the duration and intensity of services provided and the role of the case managers.
The negative outcomes associated with substance dependence co-occurring with serious mental illness and the acknowledged difficulties in treating this group of patients led us to hypothesize that substance-dependent subjects would benefit more from intensive clinical case management and that nondependent subjects would benefit equally from the two types of case management. We postulated that the more intensive, one-to-one activity of intensive case management on behalf of clients would be the necessary ingredient to improve outcomes of substance-dependent adults with serious mental illness.
We prospectively followed subjects and collected outcome data for a total of 18 months. This report presents data on outcomes at six months, the first phase of case management treatment and the period most focused on preventing psychiatric hospitalization, establishing outpatient supports, and coordinating housing, medical, and vocational services. The goal of both case management programs is to effect changes in these areas within six months.
Methods
Subjects
Subjects were 268 frequently hospitalized English-speaking patients with serious mental illness who were consecutively admitted to the psychiatric service of San Francisco General Hospital, a county general hospital and a teaching hospital of the University of California, San Francisco. Subjects were recruited from May 1994 to November 1996. To be included in the study, patients had to be between the ages of 18 and 59 years and to have had at least one inpatient psychiatric admission in the 12 months preceding the target hospitalization. They could not be currently participating in comprehensive community-based services and had to be coherent enough to provide informed consent and to complete the entry interview. They also had to be discharged within the local metropolitan area. The University of California, San Francisco, committee on human research approved the study procedures.
Treatments
One program was community based and provided intensive clinical case management; the other was hospital based and provided expanded brokerage case management (
8). Case managers in the intensive program provided psychotherapy and a wide array of integrated services, including brokerage and placement, for an unlimited time. The therapeutic relationship was conceptualized as the means by which a seriously mentally ill client could be engaged in treatment.
The expanded brokerage case management program focused on brokerage and placement services, which were provided for an average of 45 days after discharge, with a maximum of 60 days. Case managers in this program provided intensive support during the initial postdischarge period and worked assertively toward linking clients with comprehensive community services to address their specific needs. Services could be reactivated when clients were rehospitalized.
Procedures
During their hospitalization, subjects provided informed consent to participate in the study. They were then administered a comprehensive assessment battery in which their substance dependence status was determined. Subjects were stratified by the presence of at least one current co-occurring substance dependence disorder (that is, occurring in the last 12 months) and were randomly assigned, from within strata, to either intensive clinical case management or expanded brokerage case management. Before hospital discharge, subjects completed structured interviews.
Follow-up interviews were conducted one, two, and six months after discharge in community or treatment settings. We attempted to locate each subject for each interview, except for those who moved beyond a 100-mile radius of San Francisco, died, or withdrew from the study. Data on mental health services for six months before and after the index hospitalization were obtained from the management information system of the San Francisco City and County Division of Mental Health Services.
Measures
At study intake the Quick Diagnostic Interview Schedule—Revised (
10) was used to assess past-12-months criteria for substance dependence disorders. The Quality of Life Interview (QOLI) (
11) was used to assess life satisfaction in five domains: living situation, leisure activities, social relations, finances, and legal and safety. The sixth domain, work, was not used because almost none of the clients were employed. Although the QOLI contains a global life satisfaction question, we used a global quality-of-life composite score derived through principal components analysis.
The Addiction Severity Index (ASI) (
12) was used to calculate a substance use severity score. The score reflects the sum of the number of days in the past 30 days that subjects used alcohol to intoxication or used any of 12 illicit substances listed on the ASI. For example, if three substances were used, each for 15 days, the score would equal 45 days.
The Center for Epidemiological Studies—Depression Scale (CES-D) (
13) was used to measure psychological distress. It showed high internal consistency across the four assessments; alpha coefficients were above .98.
Service utilization
We derived four variables from the mental health utilization data downloaded from the mental health management information system. The case management practice variable consisted of the total number of procedures provided by case managers in either the intensive clinical program or the expanded brokerage program. Besides brokerage and placement provided by case managers exclusively, these procedures included a range of outpatient services such as contact with collaterals (family, friends, or other providers), assessment and evaluation, individual or group therapy, and medication support. This variable was used to examine case management practices of the two programs and their fidelity to the respective models.
The outpatient mental health services variable consisted of services rendered by community providers other than the program case managers. It consisted of all services listed above with the exception of brokerage and placement and crisis intervention.
The hospitalization variable consisted of the number of days a subject was an inpatient on a psychiatric unit or in a state psychiatric hospital. The psychiatric emergency service variable consisted of visits to the psychiatric emergency services at San Francisco General Hospital, the only hospital-based psychiatric emergency service for public-sector patients in San Francisco. Outpatient services, psychiatric hospital days, and visits to the psychiatric emergency service were outcome variables.
Data analyses
Service use outcomes.
These analyses were concerned with treatment, comorbidity, and time effects on utilization outcomes. Distributions of service utilization outcomes were negatively skewed because of subjects who did not receive services. We addressed the skewed distributions by testing differences in the percentage of subjects who received services and the mean number of services, including only those subjects who received services.
Time effects were first examined by comparing the six-month period before subjects entered the hospital with the six-month period after discharge. We also examined potential changes over time during the six months after discharge by dividing that period into three two-month periods.
We used McNemar tests for correlated proportions (
14) to examine changes in proportions over time. Logistic regression for each time interval was used to examine differences in proportions due to between-subjects main effects and interactions.
For continuous variables, a three-way analysis of variance was used to test between-subjects effects and interactions.
Psychosocial outcomes.
Psychosocial outcomes were examined by comparing study entry scores with scores at three time points during the follow-up period. The prototypic analytic model for these outcomes was a three-way analysis of covariance (ANCOVA) using treatment condition (two levels), substance dependence status (two levels), and time (four time points). Gender, age, and ethnicity were used as covariates in the ANCOVA. Data analysis was conducted with SPSS version 8.0 (
15).
To impute missing values for the CES-D, the QOLI composite scale, and the substance use severity indicator, we used the expectation maximization algorithm of SPSS 8.0. Before using the algorithm, patterns of missing data were examined to evaluate whether values were missing completely at random, a necessary condition for the appropriate use of the expectation maximization algorithm.
Results
We conducted intent-to-treat analyses in which all subjects who were randomly assigned were included. Of 534 patients eligible to participate in the study, 201 (38 percent) refused, and 278 (52 percent) agreed and signed an informed consent. The remaining 55 patients (10 percent) were not acceptable to the case management programs and therefore could not be randomly assigned to a program. Reasons for nonacceptance were a history of violence toward mental health professionals and geographic inaccessibility. Patients who signed an informed consent form did not differ from those who did not in age or duration of the target hospitalization. No other data were available by which to compare these groups because of a lack of informed consent.
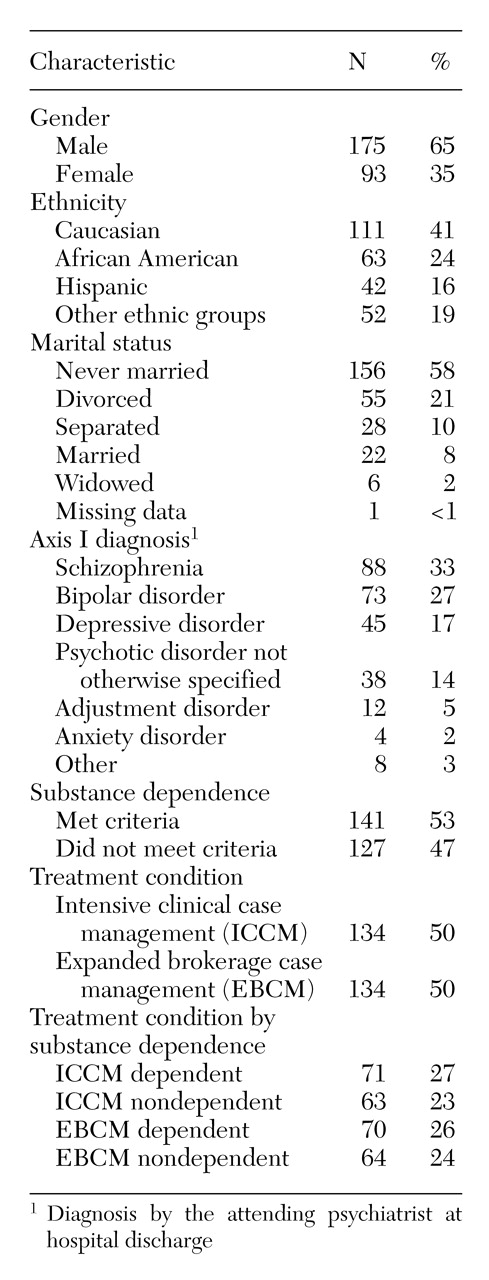
We excluded ten of the 278 subjects before the intent-to-treat analyses because their interviews were conducted in Cantonese or Spanish. The final sample of 268 patients consisted of 175 men (65 percent) and 93 women (35 percent). Of this sample, 188 (70 percent) completed six-month follow-up interviews. Patients' characteristics are presented in
Table 1.
Experimental manipulation check
Randomization.
No significant postrandomization differences were found in age, ethnicity, gender, psychiatric disorders, or psychological distress between subjects assigned to intensive clinical case management and those assigned to expanded brokerage case management.
Fidelity.
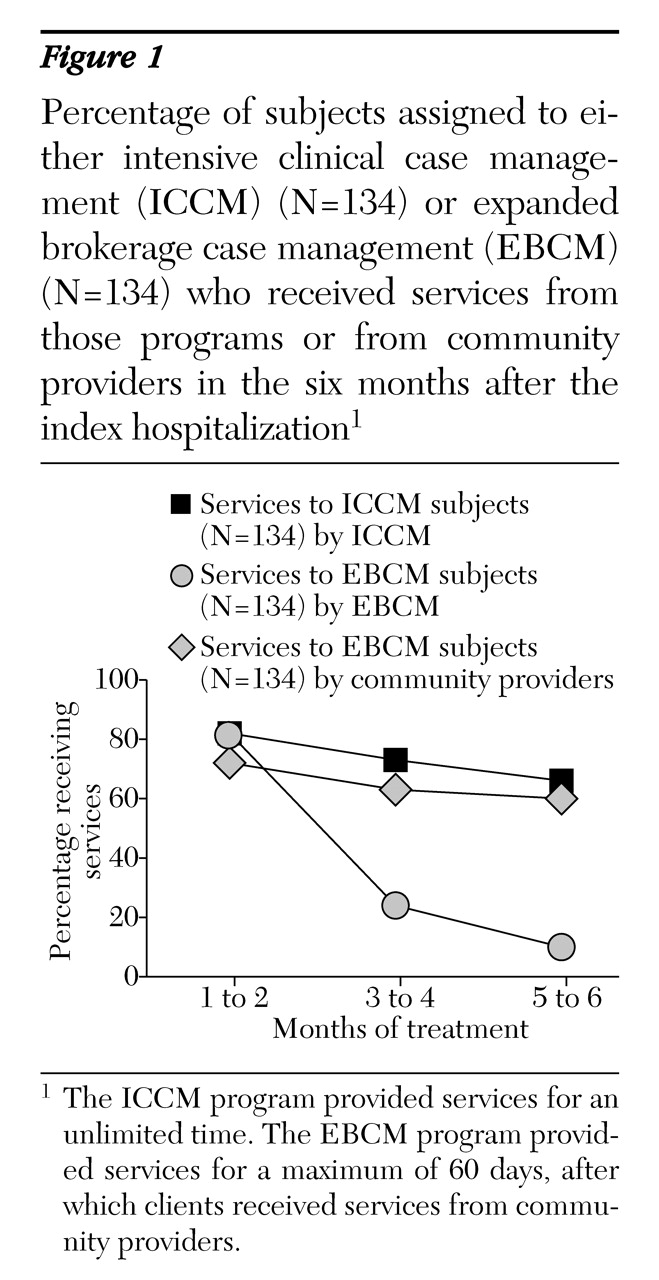
We ascertained fidelity to the respective treatment models. Subjects assigned to intensive clinical case management were expected to receive relatively more services during the first 60 days than later. They were also expected to continue to receive a relatively high level of services. During the 45-day intervention of the expanded brokerage case management program, subjects were expected to receive a similar number of services as subjects in the intensive clinical program. After approximately 45 days, their treatment was to be provided by community-based providers. As
Figure 1 shows, both case management programs generally conformed to these aspects of their respective models.
Use of outpatient services
More subjects received outpatient services in the six-month postdischarge period than in the six months before admission. A total of 239 patients (89 percent) received such services in the postdischarge period, compared with 172 patients (64 percent) in the preadmission period χ2=47.9, df=1, p< 001). No effects of treatment group or comorbidity were found. Analyses of outpatient service utilization within the postdischarge period showed no changes over time.
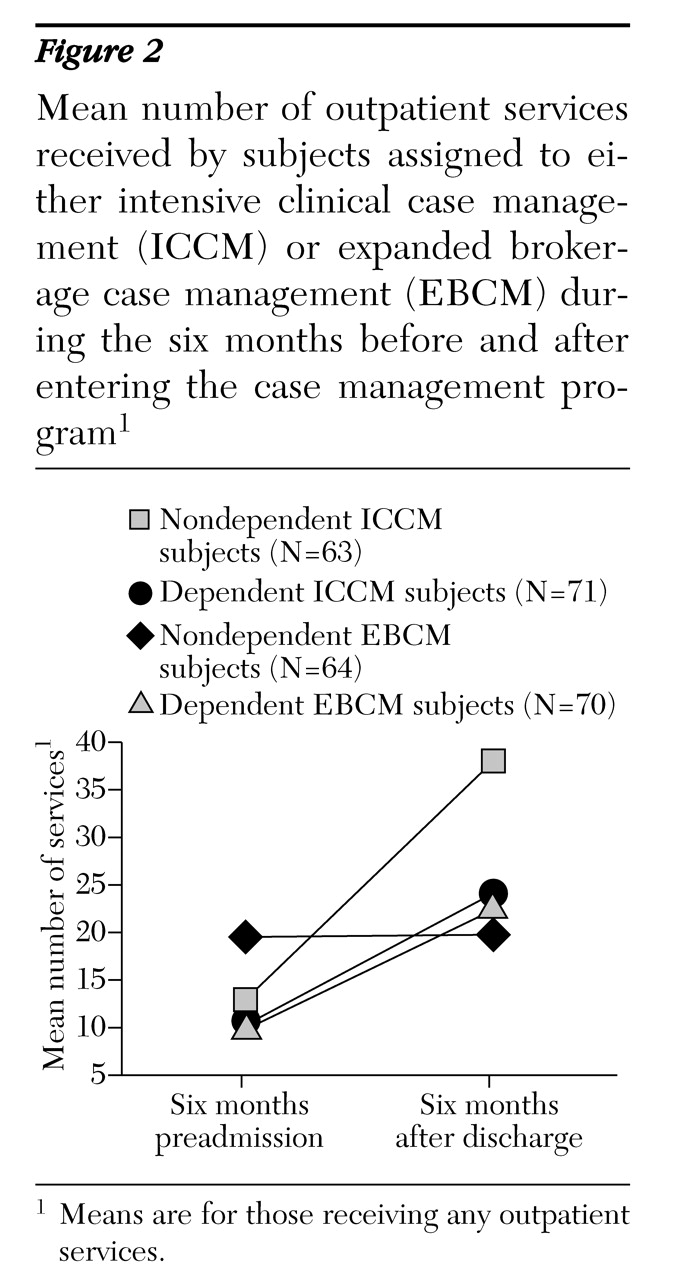
A significant three-way interaction—treatment by substance dependence by time—was found for the number of outpatient services received in the six months before admission compared with the six months after discharge (F=8.19, df=1, 156, p=.005). Subjects in the intensive clinical case management program who were not substance dependent had the greatest increase in outpatient services. They also received a significantly greater number of services in the postdischarge period than all other groups (Tukey honestly significant difference test, p<.05). The interaction is shown in
Figure 2.
No meaningful differences were found in the use of outpatient services when analyses compared postdischarge months 1 and 2 with months 3 and 4 and months 5 and 6.
Utilization of inpatient services
Fewer subjects in intensive clinical case management who were not dependent on substances were hospitalized in the postdischarge period than in the preadmission period; 23 of these subjects (36 percent) were hospitalized after discharge, compared with 43 (68 percent) in the preadmission period χ2=12.89, df=1, p<.001). No other significant differences in use of inpatient services were found between the two six-month periods.
Analyses of hospitalization that compared postdischarge months 1 and 2 with months 3 and 4 and months 5 and 6 revealed a significant time effect. Subjects were more likely to be hospitalized in months 1 and 2 after discharge (83 patients, or 31 percent) than in months 3 and 4 (52 patients, or 19 percent) χ2=13, df=1, p<.001). The likelihood of hospitalization did not change for months 5 and 6 after discharge. No other differences were significant.
For individuals who were hospitalized in both preadmission and postdischarge periods, the mean number of days hospitalized was greater in the postdischarge period than in the preadmission period (mean±SE=24.54±2.65 days versus 15.26±1.50 days; F=12.41, df=1, 78, p=.001). The mean number of days hospitalized did not change across the three two-month intervals after discharge.
Psychiatric emergency service visits
No significant treatment effects or interactions were found for subjects treated in the psychiatric emergency service. The only significant effects in these analyses were main effects for substance dependence and time. Regardless of case management program, substance-dependent subjects were more likely than nondependent subjects to visit the emergency service in the six months after discharge (90 subjects, or 64 percent, versus 62 subjects, or 49 percent; χ2=6.13, df=1, p=.013).
Overall, fewer subjects visited the psychiatric emergency service in the six months after discharge than in the six months before admission (152 subjects, or 57 percent, versus 236 subjects, or 88 percent; χ2=58.4, df=1, p<.001). No other differences were found.
The mean number of visits to the psychiatric emergency service decreased significantly over time. The mean±SE number of visits in the preadmission period was 2.46±.17, compared with 2.03±.13 in the postdischarge period (F=12.17, df=1, 131, p=.02).
Psychosocial outcomes
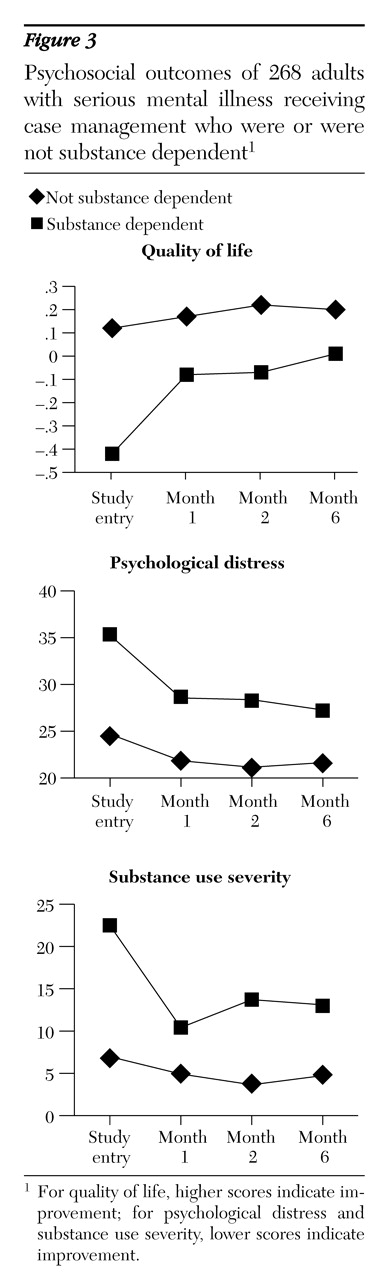
We did not find any main effects or interactions involving treatment on quality of life, psychological distress, and substance use severity. Substance-dependent subjects consistently had worse outcomes than nondependent subjects over the six months after discharge. They reported significantly lower levels of quality of life (F=11.26, df=1, 261, p=.001), greater psychological distress (F=37.60, df=1, 260, p< .001), and greater substance use severity (F=33.30, df=1,250, p<.001).
In addition to the main effects for substance dependence, substance dependence by time interactions were found between study entry and month 1 postdischarge for quality of life (F=6.57, df=1, 261, p=.01), psychological distress (F=5.53, df=1, 260, p=.02), and substance use severity (F=12.76, df=1, 250, p<.001). These interactions follow similar patterns and are shown in
Figure 3.
Discussion
Our investigation was equally focused on two issues in treatment outcomes of adults with serious mental illness: the relative effects of two comprehensive case management service delivery models and the effects of co-occurring substance dependence disorders. The first hypothesis was that there would be an interaction of case management model with substance dependence status. It was predicted that intensive clinical case management would be the most effective model for seriously mentally ill subjects who had been diagnosed as having a substance dependence disorder. The hypothesis was not supported—no differential case management treatment effects were found for substance-dependent subjects on any of the study outcomes.
However, robust and consistently negative effects of substance dependence on outcomes were found across both case management interventions. These results are consistent with the findings of our earlier report on the first 168 subjects who entered this study (
9). In that examination of data at study entry, we found that substance-dependent subjects were relatively worse on all indicators. This study shows that these negative effects were sustained during the first six months of the case management treatment interventions.
Although these effects on treatment outcomes for adults with serious mental illness have been described in the literature, we found no other example of a controlled randomized trial that examined the relative effectiveness of two case management delivery models crossed by substance dependence status.
Results suggest that the case management models studied were relatively ineffective for substance-dependent subjects compared with nondependent subjects. One of the more promising treatment strategies for substance-dependent adults with serious mental illness is integration of treatment for substance abuse and dependence with mental health treatment (
16,
17). Recent studies suggest that drug treatment interventions can be integrated with case management for adults with serious mental illness and that the outcomes are promising (
18,
19). These studies are descriptive or quasiexperimental and should be followed by randomized clinical trials. Effective integration of substance abuse treatment within the context of case management may be as important as or more important than the type of the case management intervention used.
The second hypothesis was that the two case management approaches would be equally effective for subjects not dependent on substances. This hypothesis was also not supported. Intensive clinical case management was the superior treatment for nondependent subjects. Compared with nondependent subjects in the expanded brokerage program, nondependent subjects in the intensive clinical case management program had a greater increase in use of outpatient services and were less likely to be hospitalized during the six months of case management treatment than in the six months before.
The changes in patterns of service utilization were especially interesting. The results may indicate a substitution effect in the desired direction: subjects in the intensive clinical case management program who were not dependent on substances may have "substituted" use of outpatient services for use of psychiatric hospitalization. They may have benefited sufficiently from this community-based model so that outpatient services could be used in place of hospitalization. We found no studies that demonstrated this effect. Very few studies of case management have examined use of outpatient services concomitant with hospitalization outcomes. Of the roughly 75 studies assessed in major reviews of the literature (
16,
20,
21), only three included utilization of community services as an outcome measure, and none of them described a substitution effect. Nevertheless, such substitution of services is one of the goals of both case management programs. We anticipate that more information will be forthcoming on the substitution effect when we analyze data for months 7 through 18.
Given the differences between the two programs and their fidelity to their respective models of care, the lack of evidence that the two case management interventions had any differential impact on psychosocial outcomes was unexpected. The result is not surprising, however. The research literature in this area is inconsistent, perhaps because of the range of rigor of study designs and the methods of measurement. A few studies demonstrate positive effects of case management on psychosocial variables, and many do not (
18,
19,
20,
21,
22,
23,
24,
25,
26). Two excellent literature reviews provide summaries of the domains that indicate positive changes (
16,
26).
The value of the results reported here is enhanced by the methodological strengths of the study, which contribute to its internal validity. Among the most prominent are the use of an objective research diagnostic measure that mapped onto DSM-III-R to determine the presence of a substance dependence disorder and stratified random assignment, by substance dependence status, to treatment conditions. Another methodological strength was the completion of a fidelity analysis that indicated the two case management programs provided services in a manner that was generally consistent with their articulated models and that two different case management interventions had been implemented. Other strengths included a large sample size and reliance on billing management information systems rather than subjects' self-reports for data on service use. Few studies have had this number and combination of strengths.
Conclusions
The six-month results of this controlled randomized trial of two case management service delivery models for seriously mentally ill adults with and without co-occurring substance dependence disorders did not support the study's hypotheses. However, the study did provide evidence that neither intensive clinical case management nor expanded brokerage case management is effective for seriously mentally ill adults with substance dependence disorders. Results also indicated that intensive clinical case management provided to nondependent adults with serious mental illness can yield positive changes in patterns of service use within the first six months of treatment.
Acknowledgments
This work was supported by grant MH-58056 (Dr. Havassy, principal investigator) from the National Institute of Mental Health. The authors acknowledge the contributions of David Fariello, M.S.W., William A. McConnell, Ph.D., Joanne Wile, M.S.W., and Aline G. Wommack, R.N., M.S.