Sample description
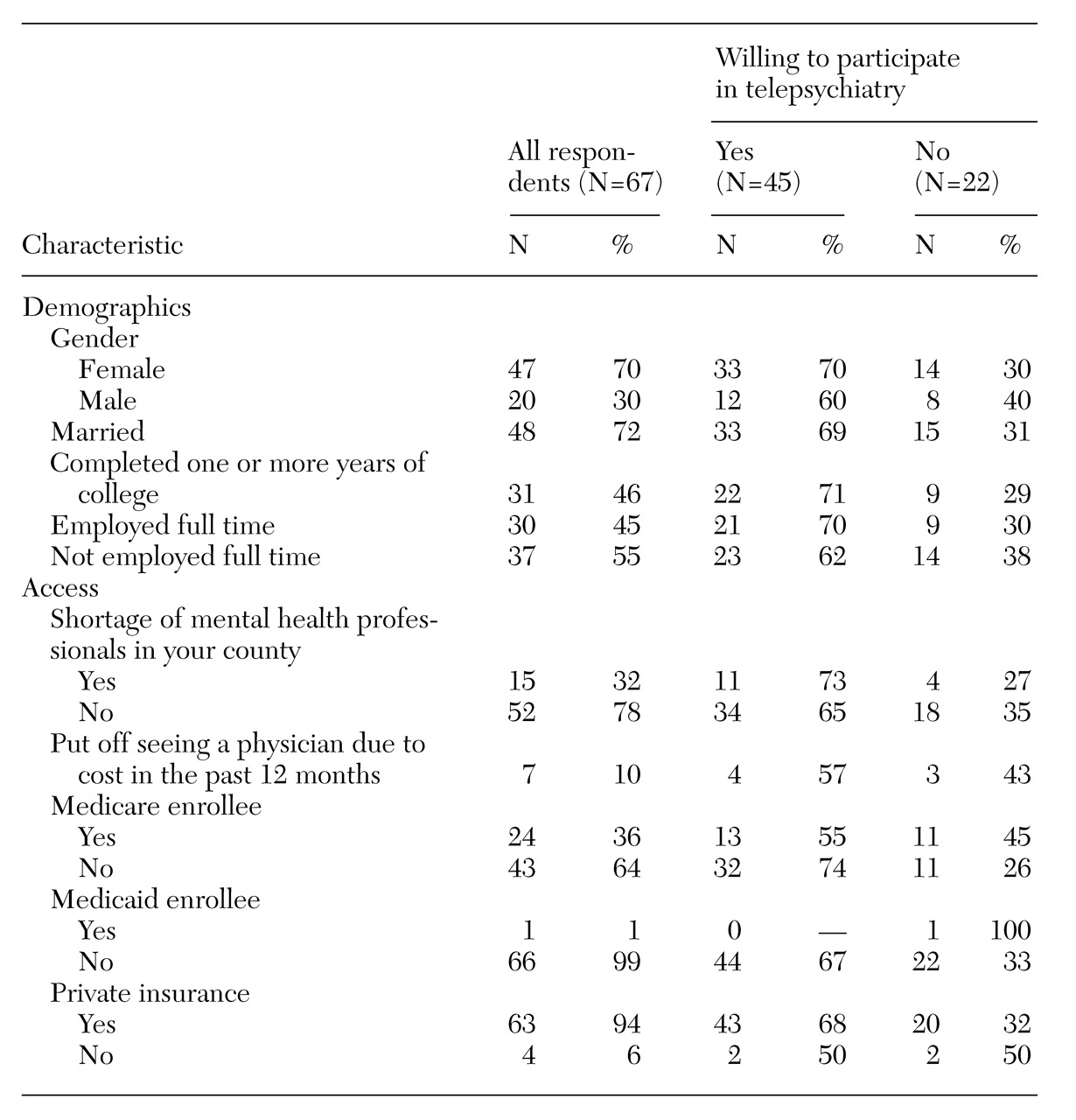
Of the 202 persons contacted, 67, or 33 percent, agreed to participate in the survey. Their mean±SD age was 53.3±17.4 years. Survey responses related to demographics and access are summarized in
Table 1.
The respondents had a mean±SD of 2±6.3 encounters with a family physician in the past six months, with a lower mean of 1.2±4 encounters with a medical specialist during the same period. More than four-fifths of the respondents (N=56) indicated that they had a personal provider they could go to if they needed medical care, and two, or 3 percent, had been hospitalized during the preceding six months.
Thirty of the survey respondents (45 percent) reported a shortage of family physicians in their counties, and 15 (22 percent) perceived a shortage of mental health professionals. Most respondents had private insurance, and only seven (10 percent) reported that they had put off seeing a physician in the past 12 months because they could not afford to pay for care. However, 58 of the 67 respondents, or 87 percent, were not satisfied with the local health care system. The mean±SD score for satisfaction with visits to the physician's office was 17.9±4.0 for the group as a whole, 18.2±3.7 for those willing to participate in telepsychiatry, and 17.3±4.4 for those unwilling to participate. Scores on the satisfaction scale ranged from 0 to 25, with 25 indicating extreme satisfaction.
Willingness to participate in telepsychiatry
Forty-five of the survey respondents, or two-thirds of the sample, expressed a willingness to use telemedicine for mental health services, and 49 of the 67, nearly three-quarters, said that they would recommend the service to a friend. About half of the Medicare enrollees in the sample of respondents were willing to participate in telepsychiatry, compared with 74 percent of those who were not covered by Medicare; however, the difference was not significant. Not surprisingly, the mean±SD age of those interested in telepsychiatry was significantly lower than those who were not, 50.1±17.6 years versus 59.9±15.4 years (t=2.21, df=65, p<.05).
The respondents who perceived their health as being good, very good, or excellent—38 respondents, or 57 percent of the total—were more willing to participate in telepsychiatry than respondents who felt their health was fair or poor. Of those who said their health was good, very good, or excellent, 79 percent were willing to participate in telepsychiatry, compared with 21 percent of those who said their health was fair or poor (χ2=5.53, df=1, p<.05).
The mean±SD number of days of abnormal activity due to physical illness in the past 30 days was 2.1±6.8 for the group as a whole, 2±6.81 for those willing to participate, and 2.18±7 days for those who were not. Chronic illness was reported by 21 of the respondents, or 46 percent, of whom 58 percent were willing to participate in telepsychiatry. The mean± SD mental health status score for all respondents was 9.8±3.2 on a scale ranging from 0 to 25, with 25 indicating optimal mental health. For those willing to participate, the mean score was 9.6±3.1, and for those unwilling to use telemedicine, it was 10.3±3.4.
The group that was willing to use telepsychiatry had a mean±SD adaptive coping score of 10.9±1.8 on a 15-point scale, with 15 indicating optimal adaptive coping skills; the group that showed no interest scored 9.9±2.3. The mean adaptive coping score for the entire group was 11±2.5. No significant difference between groups was found in the coping scores.
One-third, or 22, of the respondents were not willing to participate in telepsychiatry. The two most frequently cited reasons were a concern about confidentiality, cited by 12 respondents (55 percent), and the impersonal approach to care that the service entails, cited by 17 respondents (77 percent). Lack of knowledge about the technology was cited by six respondents (27 percent). Three respondents (14 percent) said they were unwilling to participate because of problems with hearing or vision.