The availability of novel antipsychotic medications over the past ten years has dramatically increased therapeutic options in the treatment of patients with psychotic disorders. These drugs—clozapine, risperidone, olanzapine, and quetiapine—are less likely than traditional antipsychotics to cause unpleasant and sometimes disabling extrapyramidal side effects. Moreover, clinical trials have provided evidence that the novel drugs may be more efficacious than previously available agents in improving positive and negative symptoms of schizophrenia (
1). On the basis of this evidence, clinical practice guidelines have recommended the use of these agents for patients experiencing their first psychotic episode (
2,
3). The Veterans Health Administration guidelines for schizophrenia state that either novel or conventional antipsychotics can be used as first-line agents and that patients who do not respond to a conventional agent should be switched to a novel antipsychotic (
4).
Prescribing practices for conventional antipsychotics have been shown to vary widely by patient characteristics—including age, gender, and ethnicity—and by treatment setting and geographic region. However, very few studies have examined the extent and correlates of variation in the prescription of novel antipsychotics. Many factors may influence whether or not these newer, more expensive medications are prescribed. This study focused on variations in prescribing practices among Veterans Affairs (VA) medical centers and on whether patients' sociodemographic characteristics were associated with receiving these new-generation drugs. This analysis was part of the Schizophrenia Guidelines Project, a larger project that is being funded by the Department of Veterans Affairs.
Methods
The Schizophrenia Guidelines Project is designed to examine how a concerted effort to implement schizophrenia practice guidelines in the Department of Veterans Affairs will affect the usual care that patients receive and the outcomes of that care. Sixteen VA medical centers were identified as candidate sites for participation in the project on the basis of the following criteria: at least 125 patients with a primary diagnosis of schizophrenia were discharged from the facility's inpatient psychiatry units in 1997, the facility's mental health managers were interested in participating in the project, and a second VA medical center in the candidate's Veterans Integrated Service Network also met these criteria. Of the 16 identified sites, 13 agreed to provide extracts of pharmacy and service utilization data from the local Veterans Information System Technology and Architecture databases.
Data were extracted for all patients who were discharged from inpatient psychiatry units between January 1 and December 31, 1997, and had a primary diagnosis of schizophrenia (ICD-9 codes 295.1 to 295.3, 295.6, or 295.9). For patients who were hospitalized more than once during that period, the most recent hospitalization was used. The outpatient prescription that was written closest to the patient's discharge date—within seven days before and 90 days after discharge—was designated as the index prescription. For each index prescription, we obtained information about the medication's name and strength, the quantity supplied, and the number of days for which it was supplied. Available sociodemographic data for the patients included age, gender, ethnicity, and marital status.
A total of 599 patients from the 13 facilities were included in the study sample. The number of patients at each facility ranged from seven to 79, with most facilities having between 40 and 50 patients. The mean±SD age of the patients was 48±10.3 years (range, 22 to 89 years). The majority were male (N=576, or 96 percent) and either had never been married (N=278, or 46 percent) or were divorced (N=155, or 26 percent). Forty-nine percent of the patients were Caucasian (N=292), 44 percent were African American (N=263), 6 percent were Hispanic (N=37), and less than 1 percent were Asian or Pacific Islanders (N=2). Ethnicity was not recorded for five patients.
For the analyses, we created dichotomous variables to indicate patients' marital status and ethnicity. Chi square tests were used to compare the facilities on patients' categorical variables—gender, ethnicity, and marital status—and analysis of variance was used for the continuous variable, age. A logistic regression model for the use of novel antipsychotic medications was developed, with the patients' sociodemographic factors and facility as independent variables. The facility with the median value for the use of novel antipsychotic medications was used as the reference facility. We also examined the relationship between patient ethnicity and facility.
Results
The proportion of Caucasian patients varied significantly among the 13 facilities (χ2=40, df=12, p<.001). Patient age varied somewhat, although not significantly, and no significant differences were found for gender or marital status.
Of the 599 patients in the sample, 283 (47 percent) received a prescription for a novel antipsychotic; of these, 158 (56 percent) received a prescription for olanzapine and 125 (44 percent) for risperidone. A total of 159 Caucasian patients (54 percent) received a prescription for a novel antipsychotic, compared with 124 patients (40 percent) in the other ethnic groups (χ2=12, df=1, p≤.001). No significant differences in age, gender, or marital status were found between patients who received a novel antipsychotic and those who did not.
A wide variation in the use of novel agents was found among the 13 facilities, ranging from 23 percent to 62 percent (χ
2=24, df=12, p=.019). The logistic regression model indicated that Caucasians were more likely than non-Caucasians to have received novel antipsychotics (χ
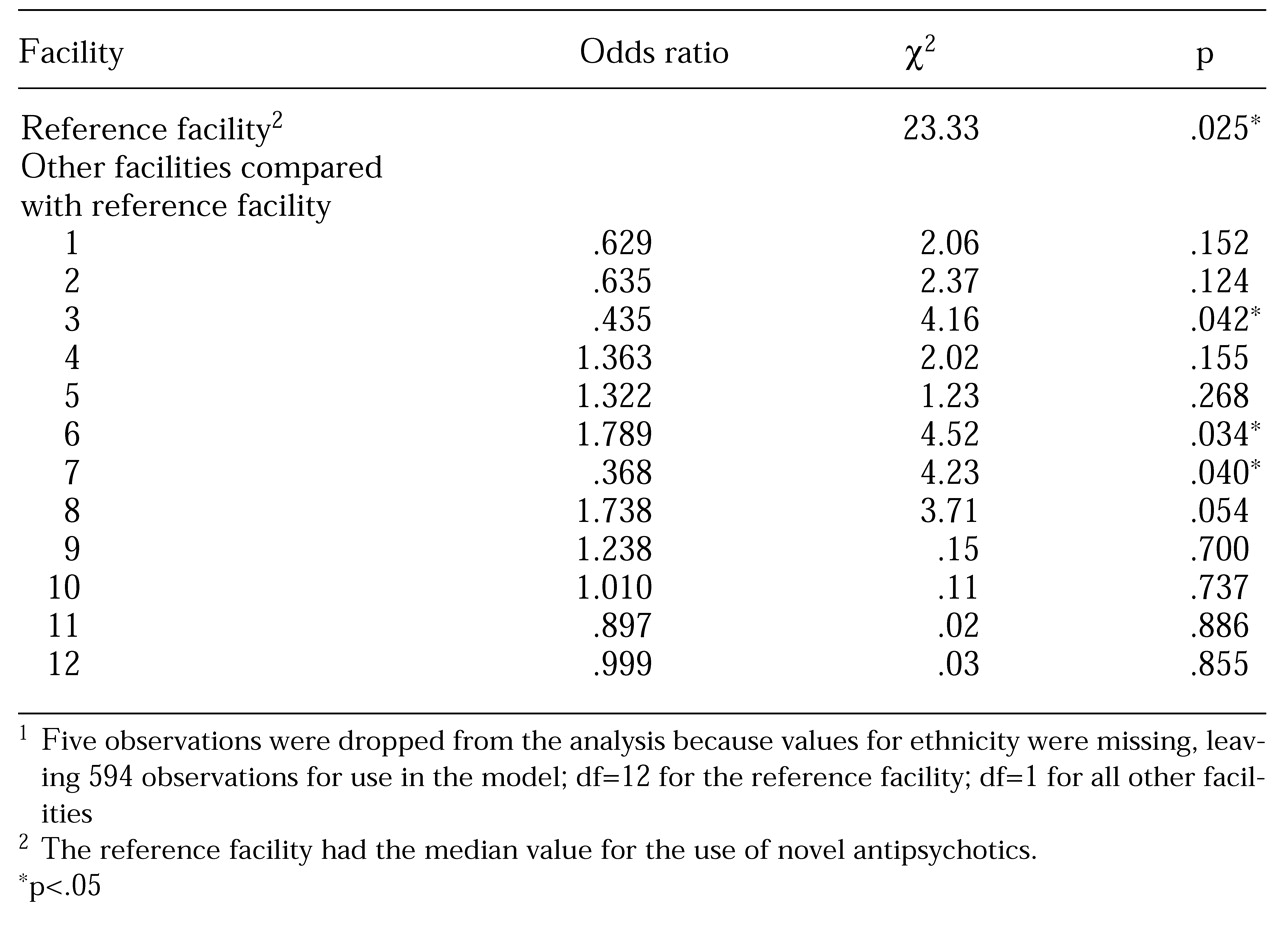
2=14.2, df=1, p≤.001; odds ratio=.509). No significant differences were found for the other sociodemographic factors. In the model, the use of novel antipsychotics among facilities varied significantly (
Table 1). No significant relationship was found between ethnicity and facility.
Discussion
In this study, the prescription rate for novel antipsychotic medications was higher than the rates reported in other studies of patients hospitalized for treatment of schizophrenia (
5,
6) and not as high as the rate reported in a more recent study (
7). Our study also found substantial variation in prescribing practices among the 13 VA medical centers examined. This finding adds to the growing body of evidence that suggests that local organizational climate may have a profound effect on prescribing practices (
5). However, without detailed data from each of the study sites, further interpretation is difficult. For instance, some of the facilities in our sample may have had specific policies that created barriers to the use of novel antipsychotics. Future research should examine specific organizational factors that could influence prescribing practices, such as local policies, provider characteristics, geographic location, academic affiliation, and perhaps differences in the regulation and marketing of drugs.
Less than half of the subjects in our study received a prescription for a novel antipsychotic when they were discharged from the hospital. However, Caucasians were twice as likely as non-Caucasians to have received such a prescription. Of the few studies that have examined the relationship between patient characteristics and prescription of novel agents, only the study by Ziguras and colleagues (
8) did not find an association between ethnicity and the receipt of a novel agent. Our study does not allow us to suggest an explanation for our findings. Possible reasons might include differences in patient preferences, the clinical appropriateness of a novel agent, or provider bias in the clinical decision-making process. Recent research suggests that in many areas of medicine, non-Caucasians appear less likely than Caucasians to receive newer, "better," and more expensive medications or technological procedures (
9,
10).
The strengths of this study include the large size and ethnic diversity of the sample. However, there are limitations inherent in the use of administrative data (
6). We were not able to control for numerous factors that could influence prescribing decisions, such as a patient's treatment history and severity of illness, nor were we able to examine specific organizational characteristics that may influence prescribing practices. Our findings reflect the practices at 13 VA facilities for a patient sample composed primarily of male veterans. Thus our results may not be generalizable to other settings and to female patients. Further study is needed to confirm the extent of variation in prescribing practices among other inpatient facilities and outpatient settings.
Conclusions
The significant variations found among facilities and ethnic groups in the rate of prescription of novel antipsychotic agents indicate that research is needed to identify the factors that explain disparities in prescribing practices. Additional research is needed to determine the clinical appropriateness of these practices and to test interventions to improve practices.
Acknowledgments
This work was supported by grants CPG 97-027 and MNH 98-001 (Mental Health QUERI Coordinating Center) from the Office of Research and Development, Department of Veterans Affairs Health Services Research and Development Service, and the Veterans Integrated Service Network 16 Mental Illness Research, Education, and Clinical Centers. Dr. Owen's work on this project was partially supported by a Health Services Research and Development Service Advanced Research Career Development Award. The authors also acknowledge help from Greer Sullivan, M.D., M.S.P.H.