General hospital psychiatric units have served an important role in treating persons with mental illness since their beginnings in London in the late 1720s and in the United States in 1902 (
1) and their establishment in major U.S. teaching hospitals in the 1930s (
2). The number of psychiatric units in the country grew rapidly in the 1940s and 1950s, and by 1963 more patients were treated on general hospital psychiatric units than in public mental hospitals (
1).
The quality of psychiatric care provided on psychiatric units is higher than that provided on general hospital wards (
3,
4,
5), yet psychiatric treatment on general wards is still common, even for patients with severe disorders (
6). Little is known about the factors that influence the decision to treat a patient on a psychiatric unit or on a general ward. Although in theory this decision should be made solely on the basis of clinical need, other patient and provider characteristics may have a role.
Greenhill (
1) suggested in 1979 that less than 10 percent of hospitals with psychiatric units put psychiatric patients on general wards and that psychiatric patients treated on general wards, in scatterbeds, tended to be those with medical comorbidity or neuroses. However, no quantitative studies or even recent anecdotal accounts are available to confirm or disprove these speculations. The only existing study was descriptive and did not distinguish between patients treated in a general hospital bed within a facility that had a psychiatric unit and those treated in general hospital beds because the admitting hospital did not have a psychiatric unit (
6).
The study reported here addressed this limitation by using data for Medicare beneficiaries admitted to general hospitals with psychiatric units to examine which patient and hospital characteristics predicted treatment on the psychiatric unit.
Methods
The study population was 169,798 aged and disabled Medicare beneficiaries with a primary ICD-9 psychiatric diagnosis who were admitted in 1990 to nonfederal general hospitals with a psychiatric unit. Only initial admissions were analyzed. Psychiatric units were defined as those exempt from Medicare's prospective payment system—about two-thirds of all hospital-reported psychiatric units.
Data were obtained from the 1990 census and the following Medicare files: 1989-1990 inpatient standard analytic claims; 1990 denominator, provider-of-service, and exempt units files; and 1990 cost reports. A total of 2,170 episodes were excluded because unit availability could not be determined; because the beneficiary had discontinuous or group health plan coverage, non-U.S. residence, or overlapping stays; or because zip code data were missing.
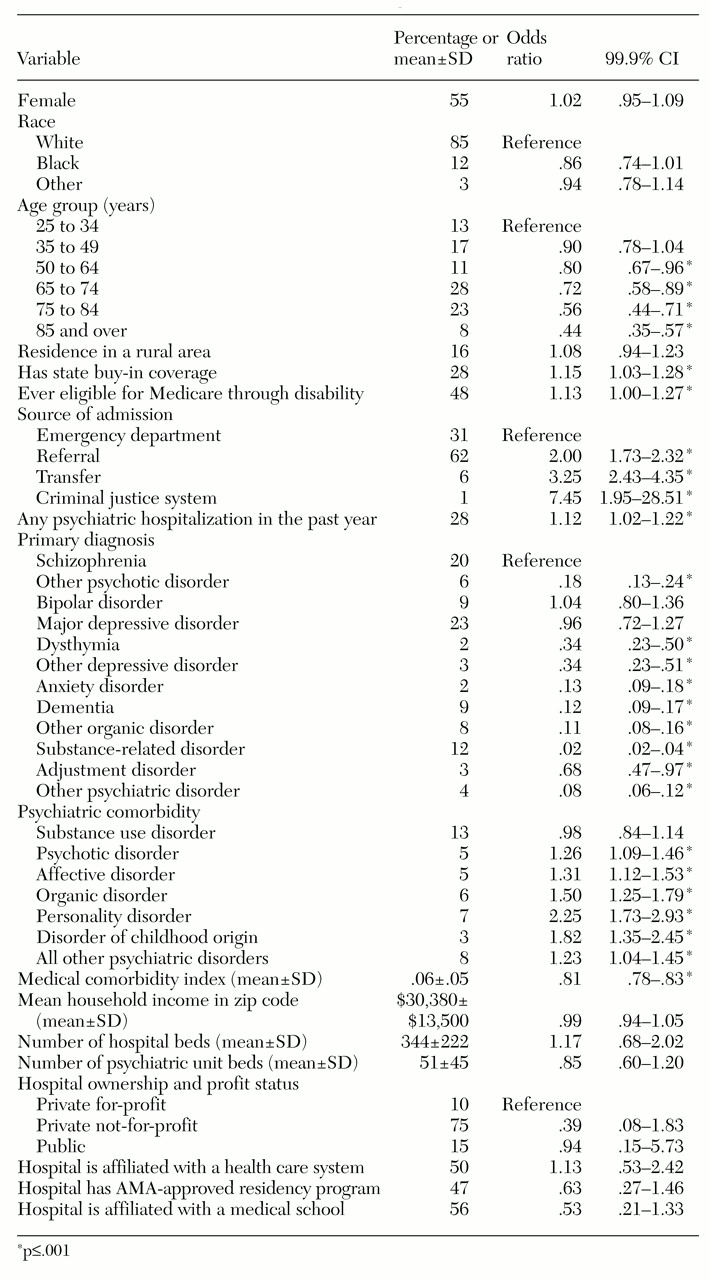
Descriptive statistics were calculated, and multiple logistic regression was used to examine patient and hospital characteristics associated with treatment in the psychiatric unit of beneficiaries admitted to hospitals that had such units. Clustering corrections were used to account for within-hospital correlation. Percentages or means, odds ratios, and 99.9 percent confidence intervals are reported.
Patient characteristics included the types of primary and secondary psychiatric diagnoses, a medical comorbidity index, age, sex, race, state buy-in coverage (primarily for persons with dual Medicaid or Qualified Medicare Beneficiary Coverage eligibility), disability status, rural versus nonrural residence, average household income in the zip code of residence, any prior psychiatric hospitalization, and source of admission. Medical diagnoses were assigned to Diagnostic Cost Group categories (
7) and combined into a single comorbidity index, using weights from a multiple logistic regression of one-year mortality. The index ranges from 0 to 1, with higher values indicating greater morbidity.
Hospital characteristics included the numbers of hospital and psychiatric unit beds, ownership and profit status, whether the hospital was affiliated with a medical school, whether it had a medical residency program approved by the American Medical Association (AMA), and whether it was affiliated with a health care system or hospital chain.
The analyses controlled for an intercept term and indicators for missing race (3 percent), missing source of admission (2 percent), and missing hospital health care system affiliation (9 percent). Frequencies for these variables were calculated on the basis of existing values only. Confidence intervals were adjusted for hospital-level clustering.
The odds ratios for dichotomous regressors approximated the probability of admission to the unit when the regressor was set equal to one, divided by the probability when the regressor was set equal to zero. The odds ratios for continuous regressors approximated the probability of admission to the unit when the regressor was set equal to the mean plus one standard deviation, divided by the probability when the regressor was set equal to the mean.
Discussion
Several conclusions emerge from this study. Beneficiaries who had more severe psychiatric illnesses and those who had more than one psychiatric diagnosis were more likely to be treated on psychiatric units, and those who had higher values on the medical comorbidity index were less likely to be treated on the psychiatric units. This pattern suggests that patients and providers perceive trade-offs in deciding on the optimal setting for care. Psychiatric units may do a better job of caring for mental illness, but at the expense of getting the best treatment for the patient's medical conditions. The growing awareness of the high rates of medical comorbidity among psychiatric patients and the limitations of medical and psychiatric units for patients requiring both types of care has spurred the growth of medical-psychiatric units (
8).
Patient sociodemographic and hospital characteristics generally played little role in determining the care setting. The finding that decisions about setting of care were based primarily on patient clinical characteristics is reassuring, because treatment patterns are frequently found to be related to hospital financial incentives or patient characteristics seemingly unrelated to need per se, such as race. Two possible exceptions were that beneficiaries with state buy-in coverage were more likely, and older beneficiaries less likely, to be treated on psychiatric units. The impact of state buy-in coverage might represent the influence of supplemental insurance or perhaps its association with poverty.
The age effect was particularly striking. The oldest beneficiaries were only about half as likely to be treated on psychiatric units as the youngest beneficiaries, even after psychiatric and medical morbidity were controlled for. Low use of psychiatric units among older patients may result from providers' anxiety about working with patients who have chronic medical conditions and the putative reluctance of psychiatric nurses to work with geriatric inpatients (
9). Alternatively, age may serve as a proxy for unmeasured clinical severity—that is, it may represent lower acuity of psychiatric illness or greater acuity of medical comorbidity.
Understanding the reasons for the lower use of specialty units among older patients is important. Psychiatric hospitals reputedly do not view elderly patients as central to their practice (
2), and Medicare limits lifetime coverage of psychiatric hospital care to 190 days. Unsurprisingly, therefore, 81 percent of elderly Medicare beneficiaries hospitalized for psychiatric disorders are treated in general hospitals (
6). It has been argued that psychiatric specialty units are well suited for treating the mental and medical illness of elderly patients (
9,
10), which suggests that they have a potentially important role to play in providing high-quality psychiatric care for the aged. However, to realize this potential, units may need either better integration of medical care or better provider education, depending on the reasons for the apparent barrier to access for elderly patients.
The analysis presented here is subject to certain limitations. It was not possible to distinguish between different types of general hospital beds, to examine transfers or the roles played by patient versus provider preferences, or to assess the hospital's motivations in its triage process. Furthermore, the data are from a period preceding the explosion in managed care. Although only 13.5 percent of Medicare beneficiaries are enrolled in health maintenance organizations, the rise in managed care and other trends such as public psychiatric hospital closings may have increased the predominance of psychiatric units over psychiatric hospitals because of their shorter lengths of stay and lower costs (
6). More recent data probably would show more admissions to psychiatric units and greater severity of illness among patients admitted to psychiatric units as the setting of care for persons with severe mental illness shifts away from psychiatric hospitals.