The use of physical restraint in psychiatric settings is highly controversial, and the issue is all the more contentious for the lack of systematic data collection and careful evaluation of indications, methods, outcomes, and adverse events. In July 1999 the Health Care Financing Administration (HCFA), now the Centers for Medicare and Medicaid Services, issued rules on restraint and seclusion for general and psychiatric hospitals that participate in Medicare and Medicaid (
1).
The rules require that a physician or a licensed independent practitioner make a face-to-face assessment of a patient within one hour of the initiation of restraint or seclusion. The "one-hour rule" has provoked tremendous debate as smaller and rural facilities struggle to comply with this "un-funded mandate." The rules also shorten the interval between mandatory renewal orders, codify requirements for staff training, and create more stringent requirements for documentation. No data on the use of restraints on inpatient psychiatric wards have been published since these rules were put into effect.
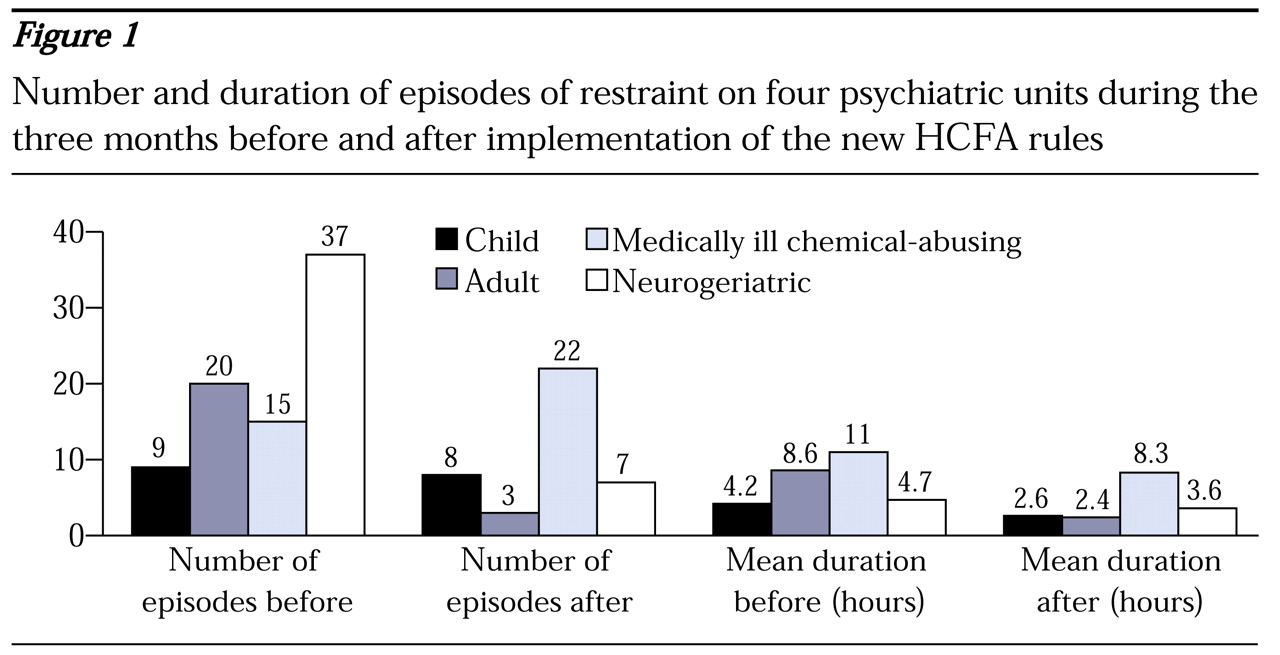
We report information about restraint episodes on four psychiatric units with a total of 80 beds at the University of Rochester Medical Center during the three months before and the three months after the new rules were initiated. Throughout this period the units' occupancy rate remained between 95 and 100 percent. The medical center has four specialty units—a child and adolescent unit, a general adult unit, a unit for medically ill chemical-abusing patients, and a unit for neurogeriatric patients.
Figure 1 presents data for the four units. A total of 121 restraint episodes were documented over the six-month period. The overall number of episodes decreased by more than 50 percent after the new rules went into effect. Reductions in the use of restraint were seen on all units except the unit for chemical-abusing patients, where a 46.7 percent increase occurred. The mean duration of an episode declined by 40.8 percent overall and 72.1 percent on the general adult unit. The higher rate of restraint on the unit for chemical-abusing patients may reflect the large number of delirious patients in drug and alcohol withdrawal who were served on the unit. The use and duration of seclusion decreased at similar rates (data not shown).
Trends in adverse outcomes were also examined. There were no increases in the already very low rate of injuries to staff by patients. However, a significant increase in the number of patient falls without injuries was noted on the neurogeriatric unit.
Use of restraint at this medical center had slowly decreased in the two years before the rules were implemented, although not at the rate documented here. More detailed studies are needed to determine whether such changes can be sustained over time and to identify factors associated with successful outcomes. Although the data here are preliminary, a reduction of more than 50 percent in restraint episodes and of nearly 50 percent in their duration suggest that institutional preparations to accommodate the HCFA rules have reduced overall use of restraint in at least one academic medical center with no apparent significant adverse outcomes to date.