Relatively poor outcomes among persons with schizophrenia and related disorders (
1,
2,
3,
4,
5,
6) may partly be associated with delay in treatment, lack of integration and phase specificity of medical and psychosocial treatments, and a system of care that fails to address patients' specific needs. Interest in early and preventive interventions for psychotic disorders has grown in recent years (
7,
8,
9,
10,
11), spurred by a variety of factors: the intuitive appeal of such interventions, reports of a relationship between a greater duration of untreated psychosis and poor outcome (
12,
13,
14,
15), the development of novel antipsychotic drugs less likely to produce extrapyramidal side effects (
16,
17,
18,
19,
20), and shifts in the care of persons with severe mental illness from the hospital to the community. Several programs have been established that address issues related to the early phases of psychotic disorders (
21), and there is evidence to support a comprehensive early intervention strategy (
22).
Intervening early in the course of psychotic disorders poses several challenges related to specific needs of persons who, in general, are young, are inexperienced with mental health services (
23), and are unlikely to follow through with treatment designed for more chronic stages of the illness. Birchwood and colleagues (
24) have promoted the idea of a critical period after a first episode of psychosis, during which appropriate intervention is likely to enhance positive outcomes. Improvements and modifications in the delivery of care (
11,
25) that address specific needs of patients with first-episode psychosis could improve the modestly favorable outcomes reported in previous studies, particularly if treatment is provided early (
26).
The development of a comprehensive early intervention program for psychotic disorders requires a new set of strategies that are likely to improve outcome. These include using lower dosages of antipsychotic medications, relying mostly on novel antipsychotics, and applying psychological interventions that address the specific needs of young patients and their families.
In this article we describe a comprehensive approach to treating first-episode psychosis, and we report the clinical status at one year of an epidemiological cohort of patients with first-episode psychosis who were treated in a comprehensive program designed to address the specific needs of this patient group.
The Prevention and Early Intervention Program for Psychoses
The Prevention and Early Intervention Program for Psychoses (PEPP) was established to assess and treat all cases of first-episode nonaffective psychosis among persons between the ages of 16 and 50 years in a predominantly urban population of about 390,000 and to promote early recognition and referral. Referrals are accepted and encouraged from all sources, including the patient and his or her family. Both patient and family are systemically informed and educated about psychosis as a serious mental illness. No parallel service exists in this jurisdiction, and the population has equal and free access to all health services. Hospitalization for initial treatment is available, but treatment provided by the program in the community is preferred.
An initial screening assessment, conducted within 48 hours of referral, identifies the presence of psychotic symptoms, which then serves as justification for further comprehensive psychiatric, family, and cognitive assessment with a standard protocol.
The program uses a modified version of an assertive case management model that recognizes patient characteristics specific to the early phase of the illness (
23). These specific issues are addressed through modifications in the content of psychosocial interventions. Treatment is based on the stress-vulnerability model of the development and course of psychotic disorders (
27,
28), and it includes low dosages of novel antipsychotics and several psychosocial interventions. Patients who have not achieved remission after one year with an adequate trial of at least two antipsychotic drugs—most often risperidone and olanzapine at a maximum tolerated daily dosage of up to 6 mg and 20 mg, respectively—are advised to try clozapine therapy. Benzodiazepines are used initially to control agitation and anxiety and are gradually tapered. Antidepressants (selective serotonin reuptake inhibitors) and mood stabilizers are used when indicated.
Various psychosocial interventions are provided. A group intervention called "recovery through activity and participation" (RAP) is provided in an outpatient setting to both inpatients and outpatients twice a week for two hours for a maximum of three months. The objectives of this intervention are assessment and bolstering of basic life skills, communication, and mutual support during the transitional phase of recovery from acute symptoms of psychosis.
An eight-week "youth education and support" (YES) group is conducted weekly for two hours with six to eight patients between the ages of 16 and 30 years whose acute psychotic symptoms have undergone at least partial resolution. The sessions, organized in the following sequence, reflect pairing of relevant themes: an introductory session, self identity and the definition of psychosis, peer pressure and drug and alcohol use, family and social relationships and medications, stigma and strategies, social skills and recovery, return to school or work and warning signs, and a final review.
Cognitively oriented skills training is provided in ten weekly two-hour group sessions. Usually this intervention is provided to patients who have completed the interventions described above and who are likely to be seeking to reenter school or the workforce.
Family intervention based on the model of Anderson and associates (
29), with modifications to address the specific needs of younger first-episode patients, is also provided. After a period of engagement, initial crisis management, and support, intervention is provided in two stages—an initial series of three evening psychoeducation workshops that provide information relevant to the early phase of the illness for a group of four to eight families, followed by individual support and intervention based on specific needs. The specific issues covered are ambivalence about diagnostic issues, dealing with stigma, substance use and abuse, family relations, coping with symptoms, and the family's role in the patient's adherence to treatment regimens.
Three video modules that depict real-life scenarios have been developed to give families practical guidelines about the management of various issues specific to families of persons with first-episode psychosis. A problem-solving approach is used to provide individual family intervention to each family according to its specific needs. In addition, an active family support group comprising parents and other relatives of first-episode patients meets regularly to discuss concerns, provide emotional support to one another, and work closely with the program staff in planning additional services for patients.
Individual therapeutic interventions include supportive psychotherapy and problem solving, which are provided by the nurse case managers. This program is the primary vehicle for assisting patients in dealing with day-to-day problems and the trauma of psychosis.
Cognitive-behavioral interventions are provided to address anxiety, depression, and nonresponsive psychotic symptoms.
All group and family interventions are based on manuals. Details can be obtained from the authors or on the program's Web site (www.pepp.ca).
In this article we describe the status, at the end of one year, of a cohort of patients who entered this program between January 1997 and September 1998 and underwent treatment and follow-up for at least one year.
Methods
A total of 122 patients were referred for initial assessment during the study period. Eighty-five patients who met
DSM-IV diagnostic criteria for a psychotic disorder were admitted to the program. The Structured Clinical Assessment for DSM-IV (
30) was administered at baseline and one year later for diagnostic assessment. A modified version of the Interview for Retrospective Assessment of Onset of Schizophrenia (
31) was used to ascertain the timing of onset of both psychotic and general psychiatric symptoms. The duration of untreated psychosis was estimated from the time of onset of psychotic symptoms to the time of entry into the program and prescription of regular antipsychotic therapy. The prodromal period—the time between onset of any psychiatric symptoms and the onset of psychosis—was determined for each patient.
The Scale for Assessment of Positive Symptoms (SAPS) (
32) and the Scale for Assessment of Negative Symptoms (SANS) (
33) were used to assess the severity of symptoms at baseline and at one year. Possible total composite scores range from 0 to 150 for the SAPS and 0 to 100 for the SANS, with higher scores indicating more severe psychopathology. All clinical ratings were made by experienced clinicians (AKM, RM, LC, RH), who had at least 80 percent agreement to within one point for all items on the SAPS and the SANS. Symptoms were rated with reference to the one-month period before the assessment.
Total positive and negative symptom scores were derived by adding all composite scores on each subscale of the SAPS and the SANS. Syndrome scores for reality distortion, psychomotor poverty, and disorganization and items constituting each syndrome were based on the previously reported factor analysis (
34) and were confirmed by using a larger sample of patients with first-episode psychosis in the program. Complete remission—that is, absence of psychotic symptoms—was defined as a score of 1 or 0 on all global items—hallucinations, delusions, bizarre behavior, and formal thought disorder—of the SAPS for at least one month before the assessment.
At one year, remission status, percentage change in symptoms from baseline to one year (total SAPS score, total SANS score, reality distortion, disorganization, and psychomotor poverty), number of hospitalizations after initial treatment, and number of days in the hospital during the follow-up period were examined. For within-group comparisons across time, paired t tests were used. For between-group comparisons, t tests for independent samples and chi square tests were used.
Approval for the early intervention study was obtained form the research ethics board for health sciences involving human subjects of the University of Western Ontario, and all patients gave signed consent to participate in the assessment, treatment, and follow-up protocol.
Results
Complete baseline and one-year data were available for 53 of the 85 patients admitted to the program with a diagnosis of a first episode of nonaffective psychosis. Only eight patients (11 percent) withdrew from treatment during the one-year period. Follow-up data were either missing or incomplete for 15 patients, and nine patients had either no baseline data or incomplete data.
No significant differences were noted in age, age at onset of illness, education, sex, marital status, or alcohol or drug abuse between the group of 53 patients for whom complete data were available and the other 32 patients. A lower proportion of patients in the latter group had a diagnosis of schizophrenia or a schizophreniform or schizoaffective disorder (14 patients, or 44 percent, compared with 33 patients, or 62 percent), although the difference was not statistically significant. These patients also had a shorter mean±SD duration of untreated psychosis (10.1±14.4 compared with 20.9±28.5 months, t=2.28, df=80, p<.03). A comparison of the baseline scores on the SAPS and the SANS between 18 of the 32 patients who did not complete the one-year follow-up and the 53 patients who did complete the follow-up showed no significant differences.
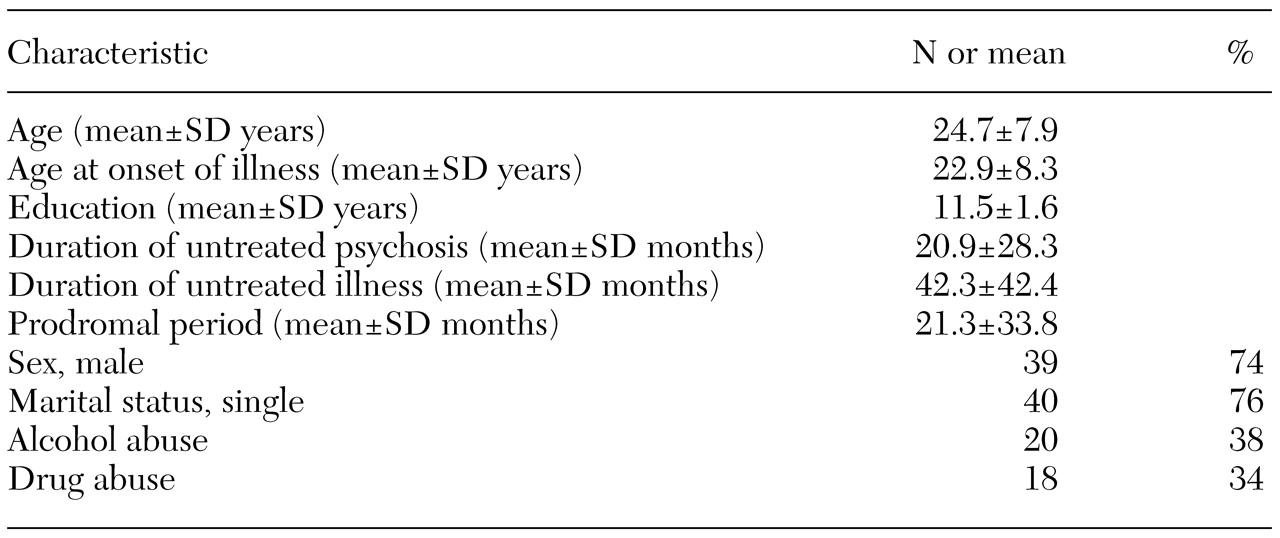
Patient characteristics
The 53 patients had been in our program for a mean±SD duration of 56± 11 weeks. As
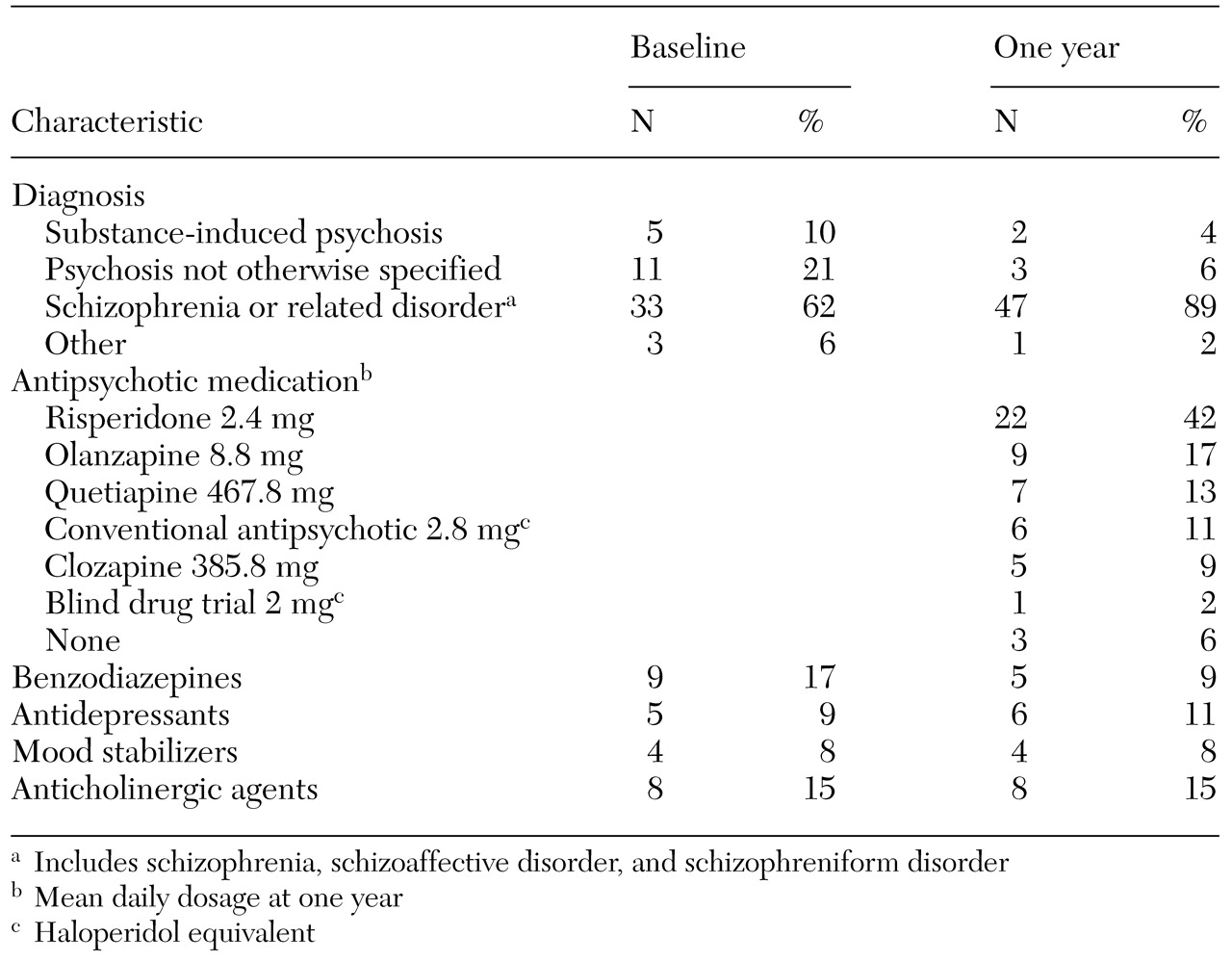
Table 1 shows, the patients were generally young and had relatively large variations in duration of untreated psychosis and duration of the prodromal period. As
Table 2 shows, most of the patients (47 patients, or 89 percent) received a
DSM-IV diagnosis of schizophrenia, schizoaffective disorder, or schizophreniform disorder after one year.
Remission and change in symptom dimensions
Thirty-seven patients (70 percent) were in complete remission at one year. No significant differences in age, age at onset of illness, education, duration of the prodromal period, or schizophrenia-spectrum diagnosis were found between patients who were and those who were not in remission. The median duration of untreated psychosis was twice as long for the patients who were not in remission as it was for those who were (10.5 compared with 5.6 months). However, this difference was not significant by the Mann-Whitney U test. The remission rate was higher among female patients (12 female patients, or 86 percent, compared with 34 male patients, or 64 percent), but, again, the difference was not significant.
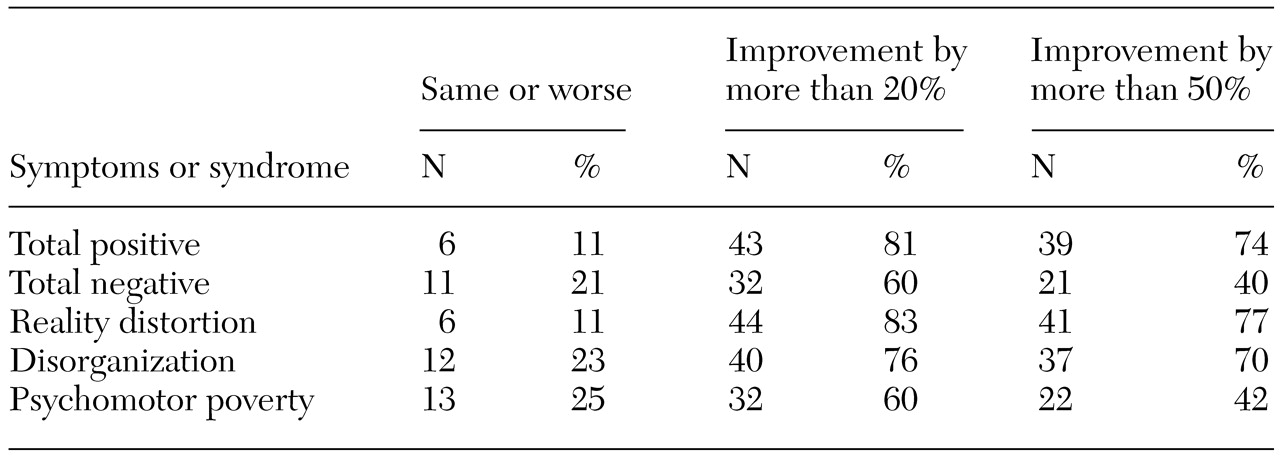
The group as a whole exhibited a highly significant (p<.001) reduction in total scores on the SAPS (t=7.7, df=52, p<.001) and the SANS (t=4.7, df=52, p<.001); reality distortion (t=7.5, df=52, p<.001); disorganization (t=5.1, df=52, p<.001); and psychomotor poverty syndrome (t=4.1, df=52, p<.001). As
Table 3 indicates, positive symptoms showed either no improvement or worsened in 11 percent of the sample, and negative symptoms showed no improvement or worsened in 40 percent. No relationship was found between mean percentage change in psychomotor poverty syndrome and reality distortion or disorganization (rho=.24 and .18, respectively), which suggests that change in psychomotor poverty was independent of change in positive symptoms. Changes in reality distortion and disorganization were interrelated (rho=.53, p<.01).
Hospital admissions
Twenty-five patients (47 percent) received their initial treatment at home through the outpatient case management program without being admitted to the hospital, and 28 patients (53 percent) were admitted to the hospital at the time of entry into the program. Neither admission or readmission to the hospital during the follow-up period nor the total number of days in the hospital was related to whether initial treatment was provided in the hospital or in the community.
On the basis of previous reports of better outcomes among patients who received phase-specific treatment within six months of the onset of psychosis (
26), we compared remission rates between patients whose psychosis had gone untreated for six months or less (23 patients) and those whose psychosis had gone untreated for more than six months (30 patients). A comparison of the two groups showed a remission rate of 83 percent in the group that had untreated psychosis for six months or less, compared with 60 percent in the group that had untreated psychosis for more than six months. A scatter plot of patients who were in remission compared with those who were not against duration of untreated psychosis showed that more than 50 percent of the patients in remission had less than six months of untreated psychosis, compared with 19 percent of the patients who were not in remission. The patients who were in remission also had a significantly greater change in total positive symptoms (80 percent compared with 44 percent, t=2.4, df=50, p<.02, two-tailed), reality distortion (79 percent compared with 48 percent, t=2.0, df=50, p<.04), and disorganization syndrome (74 percent compared with 11 percent, t=2.2, df=46, p<.04). The difference in change in negative symptoms was not significant.
Discussion
Patients who were treated in the prevention and early intervention program very likely represent a community sample of persons who have experienced their first episode of nonaffective psychosis. We assessed and treated 85 new cases in the first 20 months of the development of the program. On the basis of an estimated incidence of nonaffective psychotic disorders of 15 per 100,000, we would have expected to assess 97 patients (15×3.9×1.66) over a period of 20 months in a population of 390,000. The estimated incidence used for this calculation is higher than that reported for schizophrenia (ten to 12 per 100,000) (
35), because it includes related psychotic disorders. The characteristics of our sample were similar to those reported by the Early Psychosis Prevention and Intervention Center study, a large community-based program of early intervention in psychosis (
7,
21,
26). The large proportion of patients who were still in treatment at one year (89 percent) may suggest a major benefit of the phase-specific comprehensive approach to treating patients with first-episode psychosis.
Nearly half of the patients in the program were initially treated as outpatients. Organizational factors such as the inpatient unit's being part of the program, a stated preference for delivering care to patients while they are living at home, a strategy of using low dosages of novel antipsychotics integrated with phase-specific psychosocial interventions, and the availability of intensive case management from the time of the initial assessment, may have helped keep a significant proportion of patients out of the hospital for their initial treatment.
These strategies for reducing dependence on inpatient treatment of first-episode psychosis, apart from costing less (
36), may also help patients avoid the trauma and demoralization associated with admission to a psychiatric unit (
37). Our data show that the initial treatment setting was not associated with later use of inpatient resources.
A remission rate of 70 percent at one year, although significantly higher than that reported in earlier studies of first-episode psychosis (
38,
39), is comparable to recent reports from programs specifically designed for early detection and treatment (
22,
40). Even higher rates of response to treatment were reported in a selected sample of patients who did not represent a naturalistic community sample of first-episode psychosis and who were treated within a fixed research treatment protocol (
41). The criteria for remission that we used are very conservative (global scores of 1 or less on all SAPS items).
Here we have reported results from a naturalistic community sample of patients who were treated within a clinical protocol, including patients who had concurrent substance abuse or who may not have been compliant with their medication regimens all of the time. It is unlikely that our findings were biased as a result of the exclusion of 32 patients for whom we did not have complete data. No significant differences between the two groups were found on several demographic and clinical measures likely to influence outcome.
Eleven of the 16 patients who were not in complete remission at one year were treated with clozapine toward the end of the first year, and nine of them showed excellent response in the subsequent three months. These patients did not necessarily have to meet criteria for treatment refractoriness, and clozapine was deliberately introduced as a strategy for reducing chronicity. It is possible that introducing clozapine earlier would be beneficial to a substantial number of patients who show a slow recovery. Although the nonsignificant differences we found in the median duration of untreated psychosis between patients who were and were not in remission and the higher remission rates for those who had had untreated psychosis for less than six months may support this suggestion, it was not the purpose of this study to draw any causal inferences about the effects of duration of untreated psychosis. The relationship between duration of untreated psychosis and outcome is likely to be complex and influenced by possible confounding relationships between duration of untreated psychosis and other prognostic indicators (
15).
Improvement in negative symptoms in our sample, although modest, was independent of change in positive symptoms and may have been related to the almost exclusive use of novel antipsychotic medications and intensive psychosocial interventions. Delay in treatment beyond six months appeared to have a negative effect on the magnitude of change—or improvement—achieved in each of the positive symptom dimensions (reality distortion and disorganization) but did not significantly influence change in negative symptoms. Changes in negative symptoms may be influenced by longer-term patient characteristics, such as premorbid adjustment (
41,
42).
Conclusions
An epidemiological cohort of patients with a first episode of schizophrenia or a related disorder, when treated in a population-based treatment program in the community and given a comprehensive array of novel antipsychotics in low dosages and phase-specific psychosocial treatments, appeared to show a relatively high level of improvement on clinical measures and retention in the treatment program. Patients who received treatment within six months of the onset of psychosis were more likely to achieve remission and to have greater improvement in positive symptoms at one year than patients who entered treatment after six months. Whether these differences are related to duration of untreated psychosis or other variables requires closer examination.
Acknowledgments
The work reported here is part of a long-term evaluation of early intervention in psychosis supported by grants from the Medical Research Council of Canada. Additional support has been received from Janssen Research Foundation, Canada. Dr. Malla is partially supported through a senior research fellowship from the Ontario Mental Health Foundation.