In this era of accountability and managed care, there is growing emphasis on predicting the allocation and outcomes of mental health services. Assessment and evaluation systems that have been developed to make such predictions focus on characterizing patients in terms of both their symptoms and their level of functional impairment, assessing patients' need for treatment and providing guidelines for the allocation of services, and monitoring progress and outcomes (
1,
2).
The Global Assessment of Functioning (GAF) is the standard method for representing a clinician's judgment of a patient's overall level of psychosocial functioning. As such, it is probably the single most widely used method for assessing impairment among patients with psychiatric or substance use disorders or both (
3,
4). The GAF requires a clinician to make an overall judgment about a patient's current psychological, social, and occupational functioning. In
DSM-III-R, this rating is made on a scale from 1 to 90, with ratings of 1 to 10 indicating severe impairment and ratings of 81 to 90 indicating superior functioning (
5); in
DSM-IV, the rating is made on a scale from 1 to 100 (
6).
The rationale behind the multiaxial psychiatric diagnostic system is that each axis should reflect a different piece of information about the patient. Axis V, which reflects global functioning and is assessed with the GAF, thus should supplement existing information about the patient's symptoms and diagnoses, which are covered by axis I and axis II. In addition, ratings of the patient's current level of functioning should be of value in predicting the allocation of mental health services and treatment outcomes (
6,
7,
8). Both clinicians and researchers consider the GAF to be a key part of any outcomes assessment program (
9,
10). Moreover, according to
DSM-IV (
6), the information obtained through the GAF "is useful in planning treatment and measuring its impact and in predicting outcome."
As part of its participation in the Government Performance and Results Act, the Department of Veterans Affairs (VA) implemented a nationwide system for evaluating the allocation and effectiveness of psychiatric and substance abuse services. Under this system, the VA mandated that clinicians use the GAF in the diagnostic assessment of all mental health patients. We report on the use of the GAF in a sample of patients who participated in this monitoring program.
Symptoms and functioning as predictors of GAF scores
Diagnoses and the severity of symptoms are predictably associated with clinicians' ratings of patients' global impairment. For example, patients who have more severe psychiatric disorders, especially psychoses and posttraumatic stress disorder, are rated as having a greater level of impairment than those who have less severe disorders (
8,
11,
12,
13,
14,
15,
16,
17). In addition, GAF ratings have been associated with clinician- and self-rated depression, suicidal ideation, and lack of self-esteem (
18,
19,
20,
21,
22) as well as self-rated global distress (
2,
20), cognitive disorganization (
3,
23), schizophrenic symptoms (
24), and suspiciousness and paranoid ideation (
3).
GAF ratings of impairment are modestly associated with some indexes of social functioning, such as the extent of social networks and the need for support (
8,
25,
26), and with residential instability, lack of employment, and poor work adjustment (
14,
27). In general, however, these relationships are relatively weak; GAF ratings tend to be more closely associated with diagnoses and psychiatric symptoms than with social and occupational functioning (
16,
19).
GAF scores as predictors of service allocation and outcomes
Patients with higher levels of global impairment have a higher likelihood of receiving inpatient or residential care and a longer duration of such care (
28,
29,
30,
31,
32,
33.) However, with the exception of Bogenschutz and Siegfried (
34), who found no relationship between GAF scores and the use of outpatient mental health services, researchers have not focused on the association between GAF-rated impairment and the duration of mental health treatment or the allocation of services.
Several studies have identified associations between clinicians' ratings of patients' global functioning and improvement in patients' psychiatric and substance use problems during and after treatment (
2,
4,
24,
35,
36,
37,
38,
39). In general, these associations have been stronger than those between GAF ratings and social or occupational outcomes (
14,
21,
33,
40,
41,
42).
In an earlier study that used a different sample of patients with substance abuse, we found that GAF ratings obtained during treatment were only minimally associated with self-reported symptom outcomes and social or occupational outcomes (
14). We sought to replicate and extend these findings by addressing three questions. First, when clinicians use the GAF to rate patients' global impairment, do they consider social and occupational functioning in addition to diagnoses and clinical symptoms? Second, how closely are GAF ratings associated with patients' receipt of mental health services—that is, do patients with greater levels of impairment receive more care? Third, how well does the GAF predict patients' symptom outcomes and outcomes related to social or occupational functioning? We also examined whether GAF ratings were more strongly associated with interview-based outcome measures than with self-reported outcome measures.
Methods
In addition to mandating that clinicians use the GAF to assess mental health patients, the VA mandated the use of the Addiction Severity Index (ASI) (
43) for assessing all patients with a substance use disorder, including those with a comorbid psychiatric disorder, at entry into treatment and at a follow-up assessment six to 12 months later (
44). The primary data were obtained between 1997 and 1999.
During the first phase of the outcomes monitoring program, clinicians at 148 VA facilities used the GAF to rate 9,854 patients who also received baseline and follow-up ASI assessments. The clinicians were experienced mental health professionals—primarily psychiatrists, psychologists, and social workers—who made the GAF ratings in the context of regular clinical diagnostic interviews. The mean±SD interval between assessment with the GAF and follow-up administration of the ASI was 8.1±6.2 months.
Measures
Experienced clinicians administered the ASI during clinical interviews at baseline. We used items from the ASI to assess three symptom-related outcome criteria: psychiatric symptoms, based on the presence of any of six symptoms, such as depression, anxiety, suicidal thoughts, and hallucinations; substance use, based on whether the patient used alcohol or any of eight drugs, such as heroin, cocaine, marijuana, and barbiturates; and substance use problems, based on whether the patient experienced any problems as a result of using alcohol or drugs.
We also used the ASI to assess four social and occupational functioning variables: family or social problems, based on the presence of serious problems in getting along with family members; whether the patient had at least one close friend; legal problems, based on whether the patient was awaiting trial or was in jail; and whether the patient was employed (yes or no).
Of the 9,854 patients who were rated with the GAF and who received an ASI assessment from a clinician at baseline, 6,515 completed an ASI interview at follow-up, and 3,339 completed a self-reported ASI. The psychometric characteristics (Cronbach's alpha and corrected item-subscale correlations) of the interviewer-based and self-reported ASI scores were closely comparable (
45).
Service episodes
To examine the association between GAF ratings and receipt of services, we identified an index episode of mental health care for each patient. Specifically, we used information from the VA inpatient and outpatient databases—the Patient Treatment File and the Outpatient Clinic File, respectively—to determine receipt of mental health and medical services during the index episode.
The beginning of the episode was defined as the first day of treatment after an interval of at least 30 days without treatment. The end of the episode was defined as the last day of treatment before an interval of at least 30 days without any treatment, or, for outpatients, by a new episode of inpatient care (
46). The mean±SD duration of the index episode was 6.6±7 months.
We obtained information about specific services provided during the index episode: whether the patient received inpatient or residential care, and, if so, the number of days of care; whether the patient received outpatient mental health or medical care, and, if so, the number of visits for psychiatric, substance abuse, and medical services.
Analysis
Although GAF ratings are typically made on a 90-point scale, the rating criteria are described in nine broad categories (
5), and many researchers have combined GAF scores into fewer categories (
14,
20,
22,
31,
47,
48,
49). Accordingly, we classified patients by using five categories of GAF scores: 1 to 40, pervasive impairment; 41 to 50, serious impairment; 51 to 60, moderate impairment; 61 to 70, mild impairment; and 71 to 90, minimal impairment.
To examine whether the five groups of patients were differentiated by baseline diagnoses and clinical symptoms as well as social and occupational functioning, we used analysis of variance (ANOVA) for continuous variables and the chi square test for dichotomous variables. We then conducted multiple regression analyses to identify the extent to which patients' baseline diagnoses and symptoms were associated with clinicians' GAF ratings and whether patients' social or occupational functioning contributed independently to these ratings. Next, we used ANOVA for continuous variables and the chi square test for dichotomous variables to examine differences in the allocation of services between the five groups of patients. Finally, we calculated correlations between GAF ratings and outcomes. Subsequent analyses focused on the baseline values of the outcome variables as predictors of outcome and the additional contributions of GAF ratings to outcome predictions.
Results
For 1,175 patients, clinicians made two separate GAF ratings within seven days. Pearson's correlation was .80 between the two continuous 90-point GAF ratings and .79 between the two ratings examined by GAF category (p<.001 for both).
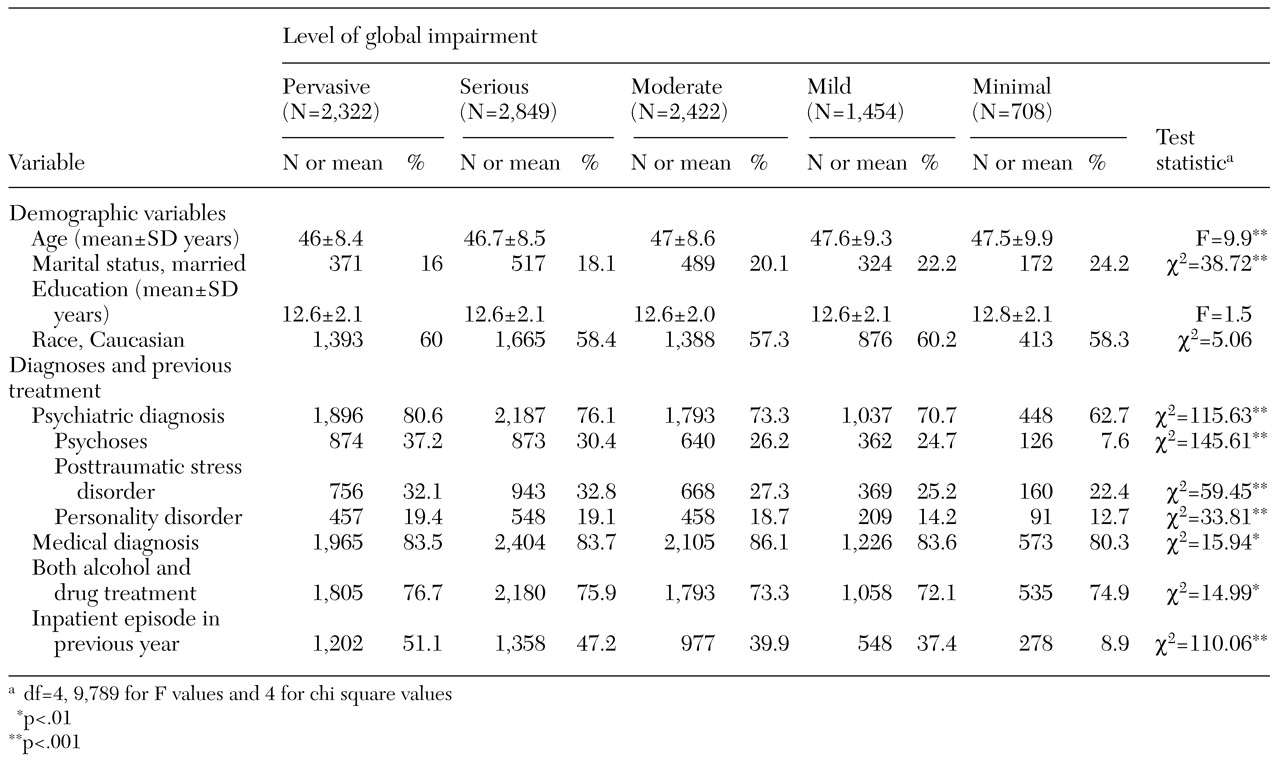
Diagnostic and basic demographic characteristics of patients in the five GAF-rated functioning categories are summarized in
Table 1. No significant differences in educational level or race were noted between the five groups. However, patients who were more impaired were slightly younger, were less likely to be married, and were more likely to have psychiatric diagnoses and to have received inpatient mental health care in the previous year.
The mean±SD age of the 9,854 patients was 46.8±8.7 years, and they had a mean of 12.6±2.1 years of education. Most patients (9,526, or 96.7 percent) were men. A total of 5,735 patients (58.8 percent) were Caucasian, 3,297 (33.8 percent) were African American, 499 (5.1 percent) were Hispanic, and 224 (2.3 percent) were from other racial or ethnic groups. Only 2,061 patients (21.1 percent) were currently married; 5,417 (55.4 percent) were separated or divorced, 341 (3.5 percent) were widowed, and 1,957 (20 percent) were single. (Information about race was not available for 99 patients, and information about marital status was not available for 78.)
Most patients (7,183, or 72.9 percent) had both a psychiatric and a substance use diagnosis; 4,847 patients (50.2 percent) had two or more psychiatric diagnoses. A total of 2,875 patients (29.2 percent) had a psychotic disorder, 2,896 (29.4 percent) had posttraumatic stress disorder, 5,445 (55.3 percent) had a depressive or anxiety disorder, 1,763 (17.9 percent) had a personality disorder, and 1,601 (16.3 percent) had other psychiatric disorders.
Determinants of GAF ratings
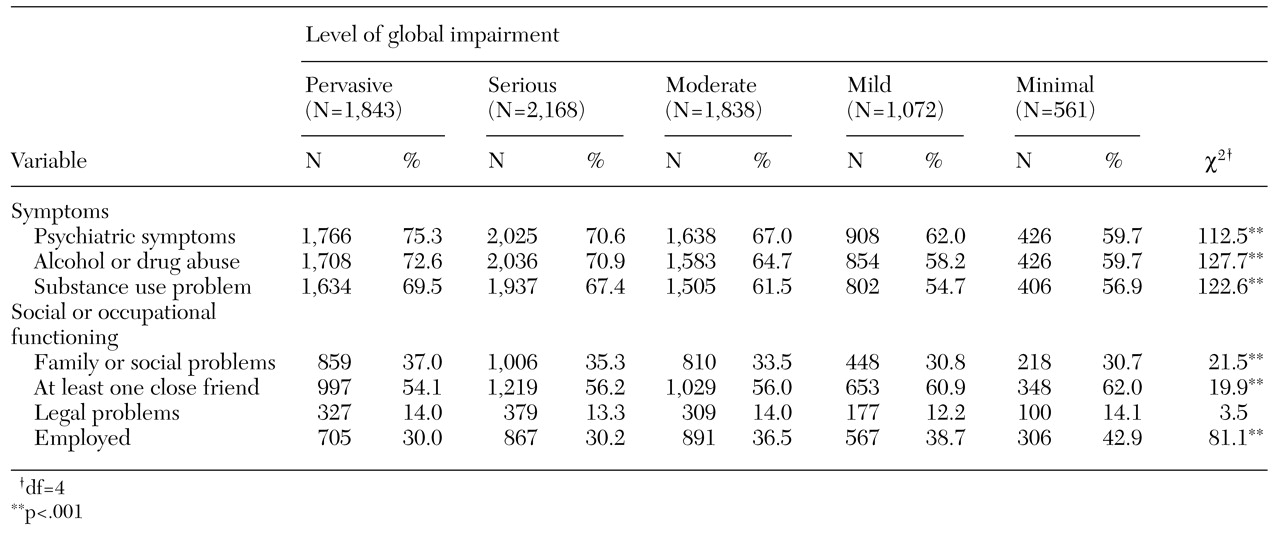
Data on the patients' symptoms and social and occupational functioning at baseline are presented in
Table 2. Patients with greater levels of impairment were more likely to have severe psychiatric symptoms, to consume alcohol or drugs, and to have substance use problems, a finding that is consistent with the differences in diagnoses between patients in the five GAF categories. Differences between groups were also found in indexes of social and occupational functioning: patients with higher levels of impairment were more likely to have family or social problems and less likely to have at least one close friend or to be employed.
We conducted multiple regression analysis to identify the best independent predictors of GAF ratings. When entered first in the regressions, the social or occupational functioning indexes accounted for only 1 percent of the variance in GAF ratings. Patients' psychiatric diagnoses, previous inpatient care, psychiatric symptoms, and substance use and substance-related problems were each significantly associated with higher levels of global impairment. After these variables were entered, employment status was the only social or occupational index that independently predicted global functioning, and it accounted for less than 1 percent of the variance in clinicians' GAF ratings. The findings were essentially the same for the prediction of continuous as opposed to categorized GAF ratings.
GAF ratings and receipt of services
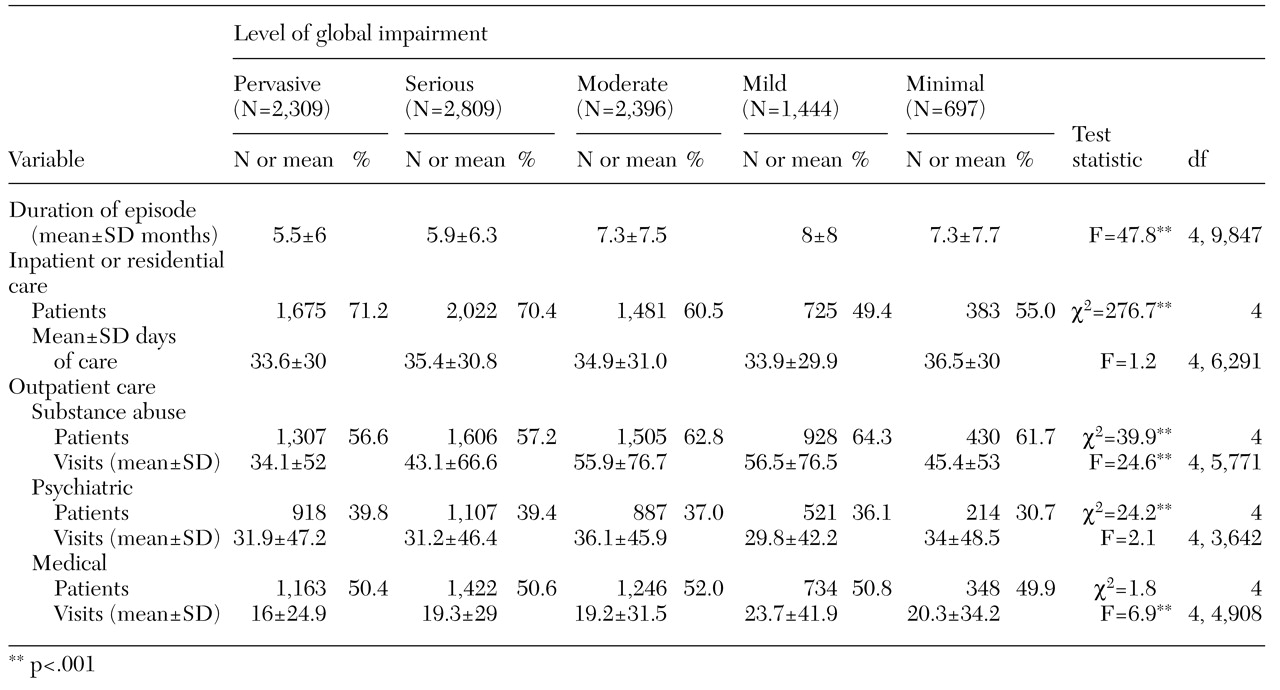
Data on receipt of services during the index episode by patients in the five GAF categories are presented in
Table 3. Patients who were rated as having more serious or pervasive impairment had shorter episodes of care than patients with less impairment. Patients with greater impairment were more likely to have received inpatient or residential care. However, more than 50 percent of the patients with mild or minimal impairment received such care. Moreover, patients with lower levels of impairment received as much inpatient or residential care as those with higher levels.
Many of the patients received intensive outpatient care during the follow-up period and thus had several visits during each week of treatment. Patients who were more impaired were less likely to have received outpatient substance abuse care, and they received somewhat less of this type of care than those who were less impaired. Patients with greater impairment were somewhat more likely to have received outpatient psychiatric care but not to have received more psychiatric care in general. Outpatient medical care did not substitute for mental health care: patients with greater levels of impairment were no more likely than less impaired patients to have received outpatient medical care—in fact, they received somewhat less medical care.
GAF ratings and treatment outcomes
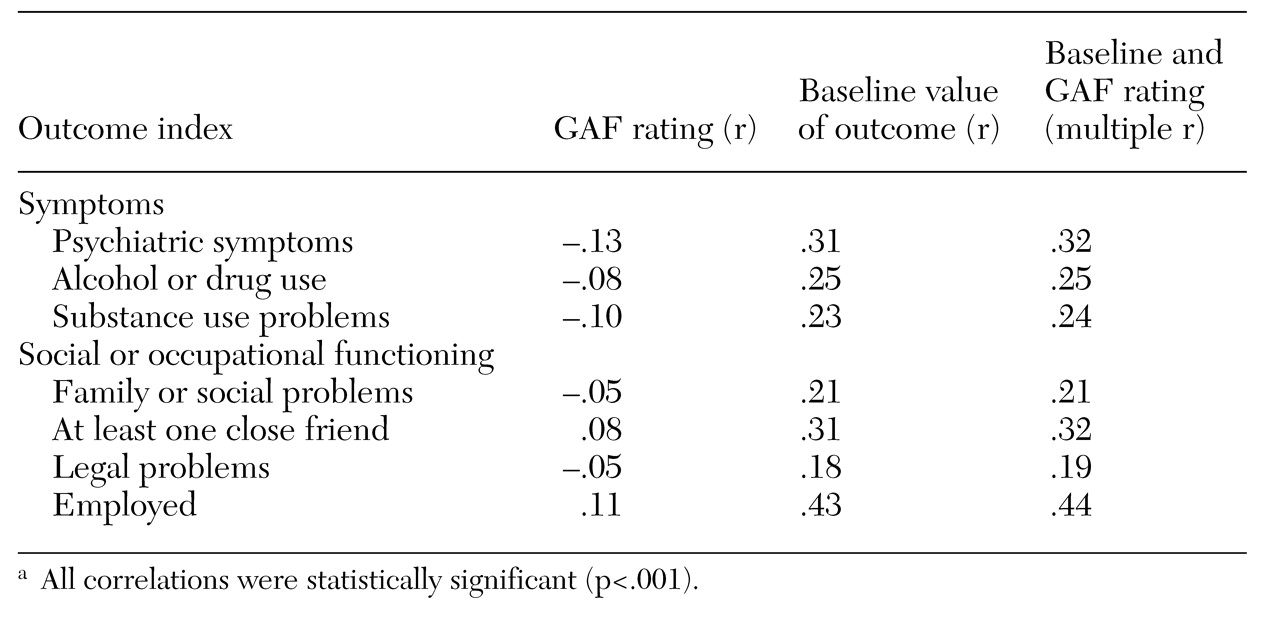
Next, we examined whether GAF ratings were associated with treatment outcomes. As the correlations in the first column of
Table 4 show, GAF ratings were modestly related to symptom outcomes: patients with lower levels of impairment had fewer psychiatric symptoms and were less likely to have used alcohol or drugs or to have substance use problems at follow-up. GAF ratings also were related to social or occupational outcomes. Patients with lower levels of impairment were more likely to have at least one close friend or to be employed and were slightly less likely to have family, social, or legal problems. However, on average these correlations accounted for only about 1 percent of the variance in outcomes.
Each of the seven baseline variables predicted the equivalent outcome criterion—that is, psychiatric symptoms at baseline predicted psychiatric symptoms at follow-up—better than the GAF rating did, as column 2 of
Table 4 shows. After the baseline value of the outcome variable was controlled for, GAF ratings made only a small contribution to each of the outcome criteria, as column 3 of
Table 4 shows. We obtained essentially identical findings when we used continuous GAF scores rather than the five categories of GAF scores.
We thought that the GAF ratings might be better predictors of outcomes as assessed by clinicians' interviews than outcomes as assessed by patients' self-reports. Accordingly, we calculated correlations and multiple correlations—again, controlling for the baseline value of the outcome criterion—between GAF ratings and the seven outcome variables for the 6,515 patients who were interviewed and separately for the 3,339 who responded to a self-report inventory at follow-up. Contrary to our hypothesis, the associations observed at follow-up between GAF scores and outcomes as assessed by interview (average r=.08, average increment in r=.01) were no stronger than the associations between GAF scores and outcomes as assessed by self-report (average r=.10, average increment in r=.01).
Discussion and conclusions
We found strong agreement between clinicians in their routine ratings of patients' global impairment. In fact, the level of agreement was somewhat higher than that found in other studies (
37,
50,
51). Nevertheless, the findings raise questions about the value of the GAF as an integral part of an outcomes monitoring system.
In DSM-IV, ratings of global functioning are included as a means of obtaining estimates of impairment to supplement existing information about a patient's diagnosis and severity of symptoms. However, in this study, clinicians' ratings of global impairment were more closely associated with patients' diagnoses, previous treatment, and severity of symptoms than with their social or occupational functioning. Patients with psychiatric diagnoses, psychoses, or a recent inpatient episode were rated as having greater impairment, as were patients who reported more psychiatric symptoms or substance use problems, or both. Once these clinical and symptom-related factors were considered, indexes of social and occupational functioning made only a negligible contribution to the GAF ratings.
These findings are consistent with the results of previous studies, which have shown moderately robust associations between symptoms and GAF ratings (
18,
20,
21,
22). Our findings and the results of these studies indicate that GAF ratings provide little or no information about social or occupational functioning that is independent of clinicians' judgments about diagnoses and the severity of symptoms (
12,
17,
27).
With the exception of the provision of inpatient or residential and outpatient psychiatric care, we found either that ratings of global impairment were not associated with the allocation of services or that patients with greater impairment received fewer services. Moreover, we found little or no relationship between GAF ratings and either symptom outcomes or social or occupational outcomes. This result was the same when we used continuous GAF scores or the five categories of GAF scores.
In a previous study (
14), we identified only minimal associations between clinicians' ratings of patients' current level of functioning and patients' self-rated symptoms and functioning at follow-up. We have replicated this finding and extended it to encompass treatment outcome as assessed by clinicians' interviews. In conjunction with the lack of previous positive findings that link GAF ratings to outcomes (
28,
52,
53,
54), these findings cast doubt on the value of including GAF ratings as predictors of treatment outcome in an outcomes monitoring system. Although intuitively appealing, a brief unidimensional rating of global functioning cannot capture changes in psychological, social, and occupational functioning that are only moderately interrelated at best (
14,
55,
56).
This study had strengths and limitations. The GAF ratings were highly reliable, and there was some evidence of their validity, because patients with psychiatric diagnoses, psychoses, recent inpatient care, current inpatient or residential care, and more psychiatric symptoms and substance use problems were likely to be rated as being more impaired. However, the findings must be interpreted in the context of a lack of more definitive information about the validity of the GAF ratings—for example, through a validity check on vignettes of patients with known levels of impairment or through experts' ratings of a subset of patients.
One potential threat to the validity of the findings is that clinicians may have underrated patients' impairment, as suggested by the fact that about 50 percent of patients who were rated as mildly or minimally impaired had received some inpatient or residential care. This apparently anomalous finding may partly reflect two aspects of the clinical care of substance abuse patients. First, a large percentage of these patients receive a brief course of inpatient detoxification at the beginning of an extended episode of care. Second, many of them, including those who are employed and do not have severe functional impairment, receive some care in a protected and substance-free residential milieu. In addition, many of the patients with dual diagnoses had axis II diagnoses (primarily personality disorders), which often are consistent with only mild or moderate impairment in global functioning as rated by the GAF. Finally, decisions about patient placement often are made on the basis of factors other than patients' global impairment, such as the availability of beds and the level of support available to the patient in the community and from family members.
Overall, the findings have ecological validity in that they reflect the use of the GAF in actual practice as part of a standard clinical diagnostic interview in one nationwide system of care. They show that when the GAF is used without regular training or validity checks—which is probably the typical application in most clinical settings—it is problematic as a predictor of service allocation or treatment outcome. The findings also are consistent with a substantive body of literature on the GAF that has been amassed over the past 25 years. Nevertheless, a definitive conclusion about whether the GAF can be more validly implemented under more controlled conditions in a naturalistic clinical situation must await further research.
Further studies are needed to determine whether more extensive training and use of experts' ratings as validity criteria can enhance the value of the GAF as a predictor of treatment allocation and outcome. Future studies could also examine whether the GAF helps clinicians communicate more effectively about patients' impairment and whether comparisons of initial and follow-up GAF scores could be used to index program effectiveness. Finally, comparative studies of the GAF and alternative assessment procedures (
6,
15,
57,
58,
59,
60) should help identify clinically valid measures that tap patients' psychosocial functioning in a way that builds on existing information about their diagnoses and symptoms.
Acknowledgments
Preparation of this article was supported by the Department of Veterans Affairs Mental Health Strategic Healthcare Group and Office of Research and Development (Health Services Research and Development Service) and by grant AA-12718 from the National Institute on Alcohol Abuse and Alcoholism. The work was conducted, in part, under the auspices of the Substance Abuse Module of the VA Quality Enhancement Research Initiative. Belle Federman, Ph.D., and Dori Lange, M.A., helped to obtain information from the VA utilization databases on patients' index episodes and prior care. The authors thank Penny Brennan, Ph.D., Ruth Cronkite, Ph.D., John Finney, Ph.D., Keith Humphreys, Ph.D., Paige Ouimette, Ph.D., Jeanne Schaefer, Ph.D., Kathleen Schutte, Ph.D., and Christine Timko, Ph.D., for their helpful comments on an earlier draft of the manuscript.