There is growing support for the efficacy and cost-effectiveness of community-based mental health care (
1). For example, assertive community treatment has been associated with better client outcomes at no greater cost than brokered case management (
2), an effect that may be partly mediated by improvements in medication compliance (
3). Long-term family psychoeducation, a form of intensified case management, has been shown to be effective in the management of schizophrenia (
4,
5,
6,
7,
8). However, because study subjects typically have been recruited as inpatients during an acute phase of the illness, it is not known whether family psychoeducation is relatively effective and cost-efficient when participants are recruited from and treated in a community mental health setting. Investigation of this issue is important because family education and support services have been reported to occur in less than 10 percent of outpatient settings (
9).
Common elements in psychoeducational approaches include the engagement of the family as an ally in treatment; presentation of detailed information about mental illnesses such as schizophrenia and their management, including techniques for improving communication, problem solving, medication compliance, and appropriate use of crisis intervention; and development of social support networks and coping skills (
10,
11). The multiple-family group approach developed by McFarlane and colleagues (
12,
13) borrows from the work of Falloon and associates (
4) and Anderson and associates (
14). The groups consist of six to eight families, including the identified patients, and are directed by two clinicians.
In the study reported here, we present one-year hospitalization and outpatient service utilization outcomes of participants with schizophrenia or schizoaffective disorder (and their family members) randomly assigned to receive multiple-family group treatment or standard care in a community mental health center. Several features of the study are noteworthy. First, most of the outpatients were enrolled in the study while they were relatively stable and living in the community. Second, the community mental health center provided services under a capitated managed care contract with the local administrative agency for outpatient services—the regional support network. The regional support network assumes full risk for outpatient mental health services and community hospitalizations but only partial risk for the use of the state hospital in its contract with the state mental health authority. Although this arrangement is complex, it approximates a common financial and service context for the outpatient management of schizophrenia within the state and nationally. A concern with managed care is undertreatment, which may further reduce the already low adherence to the treatment recommendations for family services (
15) or reduce the richness of the service background (
16,
17).
Third, about half of the study participants met DSM-IV criteria for substance abuse, and about three-quarters were receiving atypical antipsychotic medications when they entered the study. Previous tests of multiple-family psychoeducational interventions have typically compared participants receiving conventional antipsychotics and have excluded participants with severe substance abuse or dependence. Finally, family psychoeducation was provided not by the originators of the treatment, but mostly by mental health center clinicians; this may be seen as an intermediate step between the development and delivery of a novel intervention and its dissemination into routine treatment.
We compared inpatient, outpatient, and crisis service utilization data for 106 participants who had been randomly assigned to receive either multiple-family group treatment (N=55) or standard care (N=51) during the first year of the two-year multiple-family group intervention. The comparisons controlled statistically for inpatient service utilization. Other variables previously shown to be associated with hospitalization, including use of atypical antipsychotics, psychiatric symptom severity, and substance abuse at the time of random assignment to study groups, were also examined. The main hypothesis we tested was that the multiple-family group intervention would be associated with a lower hospitalization rate without an increase in outpatient service use.
Methods
Participants
The study participants were outpatients at Spokane Mental Health in Spokane, Washington. Patients were eligible if they met DSM-IV criteria for a diagnosis of schizophrenia or schizoaffective disorder, their age was between 18 and 45 years, they were enrolled in mental health services in the study community outpatient facility, they resided with family or had regular contact with family, and both the family members and the patient provided informed consent. Eligibility was not affected by a history of substance abuse or dependence or current substance abuse or dependence.
A total of 106 outpatients and all their available family members were recruited into one of seven cohorts ranging in size from nine to 17 families. Cohort start dates were spread from February 1996 through September 1999. Participants in each cohort were referred to the study by case managers. After providing informed consent and receiving diagnostic and baseline assessments, they were randomly assigned to standard care or standard care plus multiple-family group treatment. Randomization was done within each cohort. Medication status, including whether the patient was taking an atypical antipsychotic medication such as risperidone, clozapine, olanzapine, or quetiapine, was determined at baseline before random assignment to the study groups.
Recruitment began with a caseload review by case managers to identify patients who met diagnostic and family involvement criteria. Case managers then contacted eligible patients to determine their willingness to be contacted by the project coordinator. The coordinator explained the study and asked for permission to talk to other family members. Consent was obtained from both the family members and the patient. Over the course of the study, about half of the patients and families who met eligibility criteria consented to participate. The most frequent reasons for declining to participate were that patients did not want their families to be contacted, family members felt that things were going well or did not wish to commit the time, patients or family members did not wish to be randomly assigned to a treatment condition, or patients or family members did not want their sessions to be videotaped. Most patients were chronically ill; the mean time since onset of illness was about ten years. Patients and families in crisis or early in the course of the illness appeared more willing to participate.
Treatment conditions
Patients assigned to standard care received usual services, including medication management, case management, and, for some patients, therapeutic and rehabilitation services. A treatment team consisting of a case manager, a nurse, a psychiatrist, and a social worker delivered the mental health services. The team provided clinical case management services and out-of-facility services as needed.
Patients assigned to multiple-family group treatment received standard care plus the group treatment. Because the clinicians who provided the group treatment typically were not the case managers for the patients in the group, it was necessary to ensure that they communicated regularly with the case managers about changes in patients' functional status, medication problems, or service needs.
Multiple-family group treatment was intended to improve illness management, social support, and coping skills for the patient and family members. The approach was based on previous research reported by McFarlane and colleagues (
12,
13). Treatment interventions were designed to educate the family and patients about the biological underpinnings of schizophrenia and engage them in the treatment process by using a standardized protocol of videotapes, lectures, and written guidelines. Treatment components included ongoing support, formal clinical problem solving, and expansion of social support networks. Two family clinicians led the multiple-family group sessions. The clinicians were trained and supervised according to a stringent protocol that included specification of the multiple-family group intervention in a treatment manual. The clinicians acted as group leaders, family educators, and liaisons to the patient's treatment team.
The treatment protocol began with three weekly sessions that included the multiple-family group clinicians and each family separately, without the patients present. The two clinicians, along with the principal investigator (the first author) and the project psychiatrist, then provided an educational workshop for several families together, without the patients present. The workshop was modeled on Anderson and colleagues' survival skills workshop (
14).
Two weeks later, the families in each cohort met with the patients present. Weekly meetings were organized around formal problem-solving procedures to develop individualized goals and coping methods. The multiple-family group model has been described in more detail elsewhere (
12,
13). All multiple-family group sessions were videotaped for ongoing training and supervision.
Measures
Each patient was followed prospectively to determine service use for one year after the cohort start date. Service use for the year before the cohort start date was studied retrospectively. The data on service use were obtained from the existing utilization records maintained by the community mental health center.
Outpatient service was measured in minutes of staff time for the year before and the year after the cohort start date. Outpatient services included individual and group therapy sessions, medication management, and other in-person case management services provided to the patient. The multiple-family group service time was also included in the summing of outpatient service time. Use of the urgent care and crisis care services available at the mental health center were tracked separately for each group.
Use of inpatient services was measured by determining whether or not the patient was hospitalized for psychiatric treatment. State psychiatric hospitalizations and community hospitalizations were combined for analysis. Diagnosis was ascertained with the Structured Clinical Interview for DSM-IV (SCID) (
18), administered by an experienced psychiatric interviewer before the patient was assigned to a treatment condition. SCID assessments of current co-occurring substance abuse were also made at this time. Five items from the Brief Psychiatric Rating Scale (
19) were used to assess severity of positive symptoms at baseline. Baseline negative symptoms were measured with the global ratings of the Modified Scale for the Assessment of Negative Symptoms (
20).
Analysis
The analysis used an intent-to-treat design, in which data for all participants—55 patients receiving multiple-family group treatment and 51 receiving standard care—were retained regardless of their level of participation or whether they dropped out of the study. Twenty-six participants dropped out during the first year—11 from the multiple-family group treatment condition and 15 from the standard care condition. Use of atypical antipsychotics was also analyzed with an intent-to-treat approach—that is, defined at baseline. Variable distributions were examined and transformed when necessary (
21). All analyses were conducted with SPSS version 10 (
22), and directional tests of significance were used for all outcome variables.
Because the distributions of annual minutes of outpatient mental health service time were positively skewed, with means substantially higher than medians, a log transformation of these data was conducted before analysis. To test whether type of care—multiple-family group treatment versus standard care—was associated with the amount of outpatient time after random assignment to study groups, we conducted a repeated-measures analysis of variance (ANOVA) on the log of outpatient minutes for the year before and the year after random assignment. To test for the effects of multiple-family group treatment on the dichotomous hospitalization variable, we conducted a Cochran-Mantel-Haenszel analysis (
23,
24) in which the association between hospitalization in the year after random assignment and group membership (multiple-family group treatment versus standard care) was examined by controlling for the effects of hospitalization in the prior year. Because data on use of crisis care or urgent care services were not available for the year before the intervention, only an endpoint analysis could be conducted. We used a chi square test for the association between group membership and events.
We used Kendall's tau b to examine correlations between hospitalization in the first year of intervention and other variables that have previously been shown to be predictors of inpatient service use (
25,
26). Olfson and colleagues (
25) found that early readmission was associated with a history of multiple previous hospitalizations, comorbid substance use disorder, and prescription of a conventional rather than an atypical antipsychotic medication. Other studies have found that symptoms may predict later use of inpatient services (
26). On the basis of these studies, the variables we selected for testing included whether or not the patient was taking atypical antipsychotics at the time of random assignment to study groups, whether or not the patient had substance abuse at baseline, severity of positive and negative psychiatric symptoms, and number of hospitalizations in the year before the study.
Results
Demographic and diagnostic characteristics
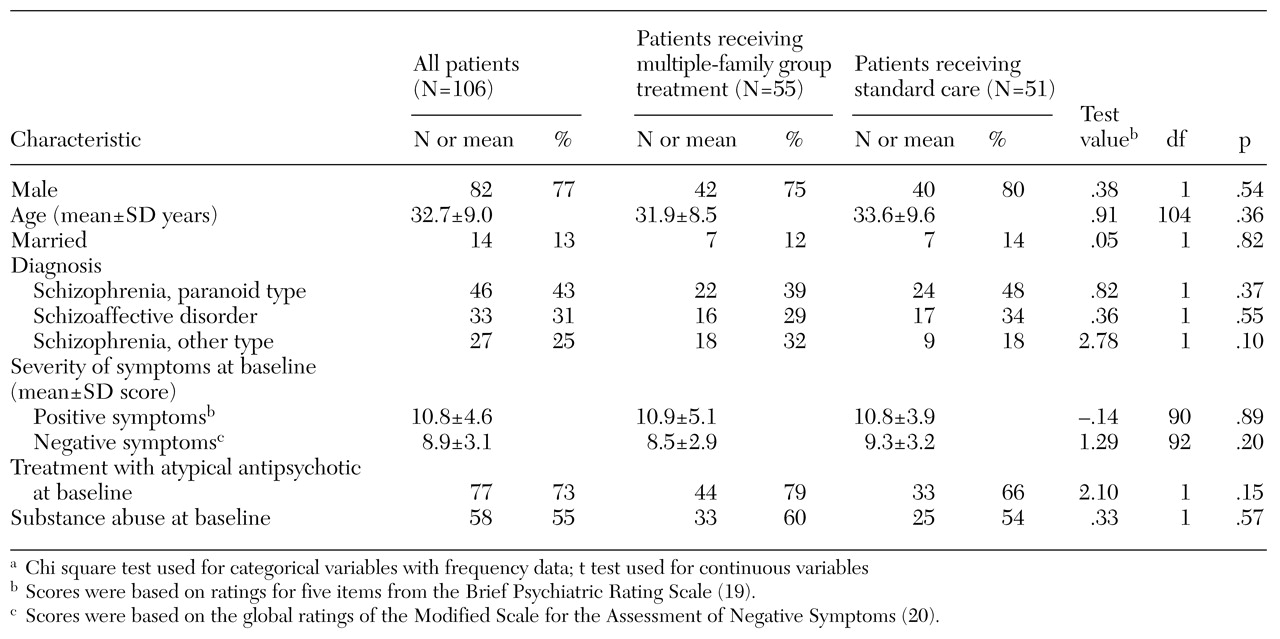
Table 1 summarizes the participants' demographic and clinical characteristics. These variables did not differ between the patients who received multiple-family group treatment and those who received standard care. There were no statistically significant differences between the groups on frequency of substance abuse, use of atypical antipsychotics, or the severity of positive and negative symptoms at baseline.
Outpatient and inpatient service use
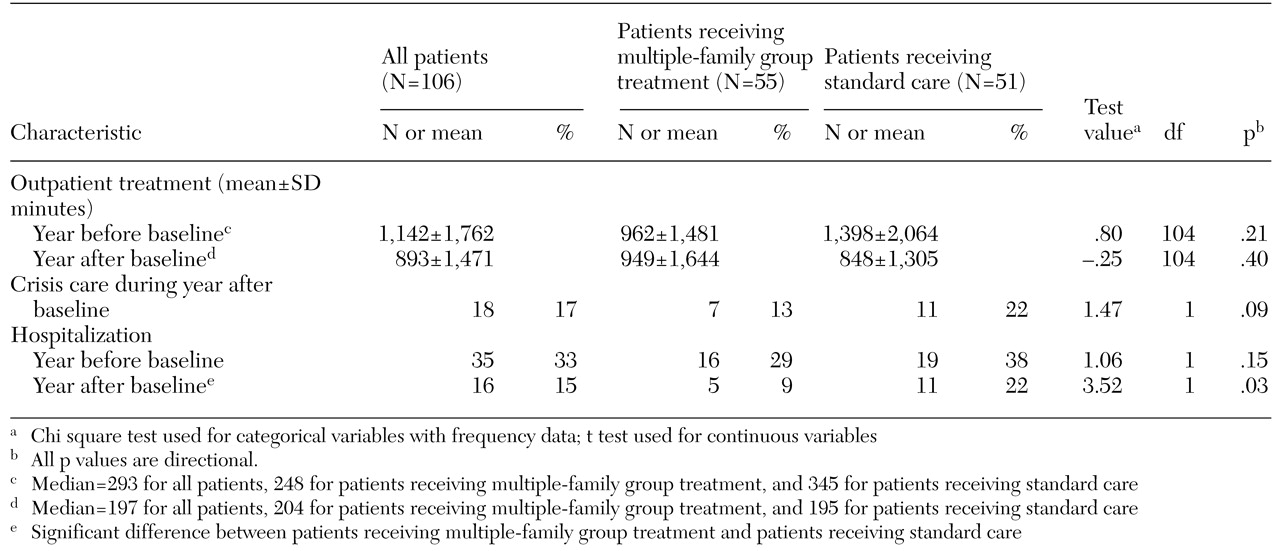
We conducted a two-by-two (group-by-occasion) mixed-design repeated-measures ANOVA on the log of the minutes of outpatient service in the year before and the year after random assignment to study groups. The amount of outpatient service use in the intervention year was lower than in the previous year (F=19.4, df=1, 102, p<.01), but neither the group main effect nor the group-by-occasion interaction was significant. Thus outpatient service use was not affected by group membership.
Table 2 summarizes the study participants' inpatient and outpatient outcomes. Eleven of the 51 patients in the standard care group (22 percent) received urgent or crisis care services during the year after random assignment to study groups, compared with seven of the 55 patients in the multiple-family treatment group (13 percent). This result favored the multiple-family group condition, but the effect was not significant.
To examine the effect of group membership on hospitalization, we used a Cochran-Mantel-Haenszel procedure that controlled for hospitalization in the previous year (
23,
24). This analysis yielded a significant association between group membership and hospitalization (χ
2=3.34, df=1, p=.04). We used Kendall's tau b to further examine the relationship between group membership and additional variables that had been identified in the literature as predictors of hospitalization. As
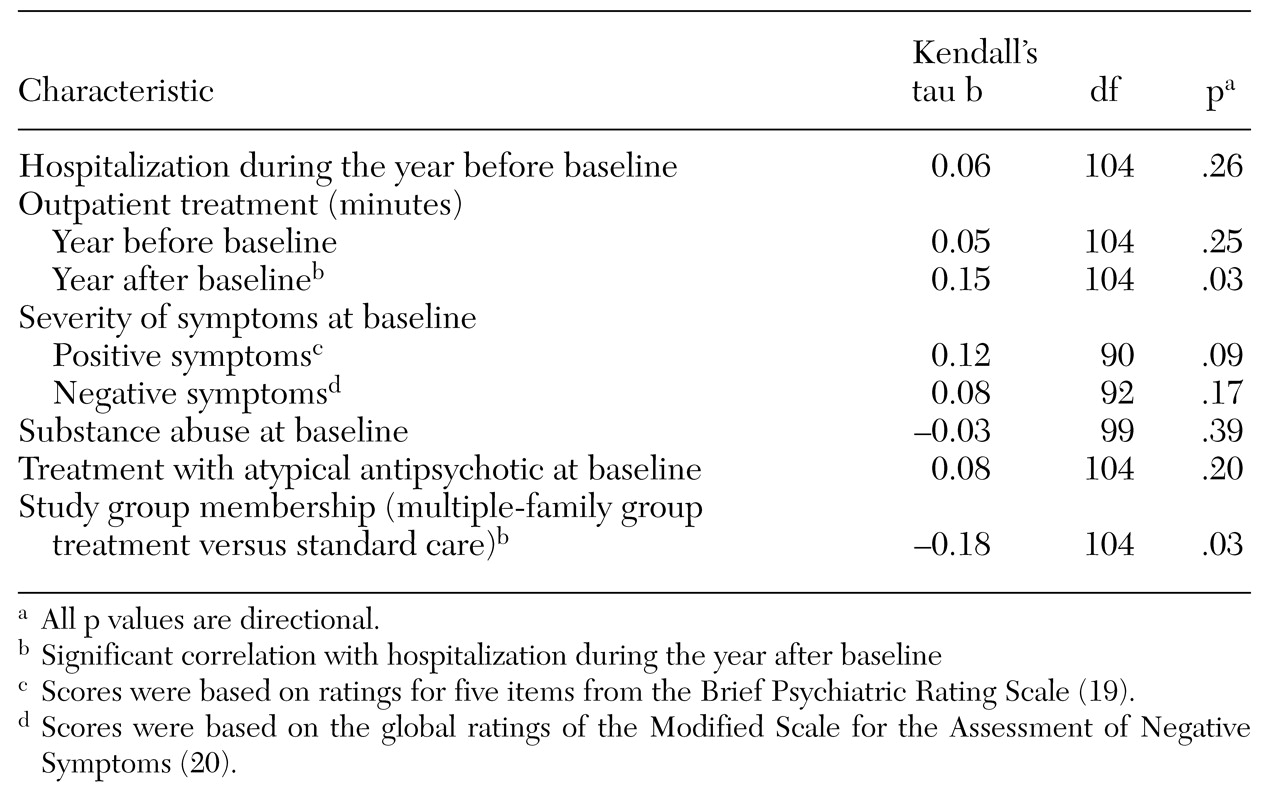
Table 3 shows, this analysis indicated that treatment with atypical antipsychotics, current substance abuse, severity of positive and negative symptoms, and whether or not a patient was hospitalized in the year before random assignment to study groups were not significantly associated with hospitalization in the year after random assignment. On the other hand, both the number of minutes of current outpatient service and group membership (multiple-family group treatment versus standard care) were significantly correlated with hospitalization in the year after random assignment to study groups.
Discussion
Considerable evidence suggests that community-based treatment of serious and persistent mental illness is effective and efficient. Indeed, the inclusion of family education as a best practice in the recommendations of the Schizophrenia Patient Outcomes Research Team project (
9) is an indication of the empirical support for this intervention. Despite this recommendation, little formal testing has been conducted of the effectiveness of psychoeducational multiple-family group treatment in managed care community mental health service systems.
The main finding of this study is that the use of psychoeducational multiple-family group treatment in a community mental health setting was associated with a modestly lower use of inpatient services without an increase in use of outpatient services. It is noteworthy that multiple-family group time was included in the count of outpatient service minutes. Although multiple-family group treatment was not significantly associated with greater use of outpatient services, a positive correlation between outpatient service use and hospitalization was noted. The reduction in hospitalization without increasing outpatient service utilization is consistent with findings from previous work (
27) showing that savings in family psychoeducation relative to individual-based management are due largely to shorter inpatient stays.
Our study focused only on mental health services and did not include general health care, services provided through the legal system, treatment for chemical dependence, or informal caregiving from family members. We did, however, obtain the medical charts for the family caregivers. In a future paper we will report on the effect of multiple-family group treatment on use of medical services by family caregivers.
As noted earlier, the managed care setting for this study represents an increasingly common financial and service context for the outpatient management of schizophrenia. As providers increasingly enter full-risk contracts that include inpatient and outpatient services, developing the capacity to control inpatient care is a wise fiscal strategy. It is noteworthy that the effects of multiple-family group treatment were observed during a time in which the availability of outpatient services for participants was decreasing. This finding is significant in view of a recent study by Schooler and colleagues (
16) that did not find improved outcomes for more intensive compared with less intensive family support programs in a service-rich context. According to Hargreaves (
17), a service-rich context may reduce the need for and the impact of an intensive family education and support program such as multiple-family group treatment. In contrast, the service environment became progressively leaner as our study progressed. A speculative but testable hypothesis is that a fairly intensive family psychoeducation model such as multiple-family group treatment may be particularly appropriate for service-lean settings, such as managed care, in which the volume of outpatient services is being decreased.
In a future report we will provide a detailed examination of potential mechanisms of action for the observed effect of multiple-family groups on clinical outcomes, such as enriched case management services (
28), improved medication compliance (
29,
30,
31,
32,
33), and improved family supports and coping skills.
Several limitations of our study should be acknowledged. First, because the study is still in progress, we have reported outcomes only for the first of the two-year multiple-family group intervention. Second, as noted, the results do not include participants' involvement with the criminal justice system or treatment for chemical dependence. Over the course of the study, participants used both of these services with increasing frequency. Third, the participants' demographic characteristics and participant selection factors limit generalizations of our findings predominantly to patients who are male and Caucasian, to female family members, and to patients and family members willing to participate in the study. Because only about half of the eligible patients consented to participate, the generalizability of our findings to nonparticipants or to patients who do not have family contact is unclear. Fourth, because the comparison group received standard care, differences between multiple-family group treatment and standard care other than the content of the two interventions, such as intensity of treatment and expectancy, could have contributed to the group differences.
Conclusions
Despite the study's limitations, the results, along with the findings of other studies showing that multiple-family group treatment reduced negative symptoms (
34), suggest that family psychoeducation may reduce psychiatric hospitalization rates without increasing use of community mental health services. Additional research is needed to evaluate whether the reduction in hospitalizations can be maintained over two years in the face of further declining outpatient services and to determine the extent to which multiple-family group treatment is cost-effective in a full-risk managed care environment such as a health maintenance organization, where the potential for cost shifting is minimized. Given the high rate of comorbid physical illness among patients with schizophrenia, both mental and general health service use should be included in such an analysis.
Acknowledgments
This study was supported by grant MH-52259 from the National Institute of Mental Health. The authors thank William A. Hargreaves, Ph.D., for his critical reading of earlier drafts and Matt Layton for his assistance in procuring the services data from Spokane Mental Health.