During the 1980s, outreach services to homeless people with mental illness were identified as a unique component of the continuum of care for this growing population (
1). The literature on outreach identified various strategies for engagement in street and shelter locations, including mobile units, intensive case management, shelter-based contact, and drop-in centers (
2). Over the past decade, mental health programs gradually have expanded their outreach to people with mental illness to include jailed populations (
3).
Other than preliminary descriptive data reported by Stovall and colleagues (
7) and cost savings data for a small number of inmates in a Chicago jail linkage program (
8), no empirical evaluations of jail outreach programs have been conducted. Because outreach is designed to enroll difficult-to-engage clients in a continuum of care, its primary objective should be to link clients with the health and social welfare service systems (
9). However, because of the scope of the challenges to reentry noted by O'Flaherty (
4), there is concern that, if effective, follow-up health care services may substantially increase costs to the agencies with which these clients are linked.
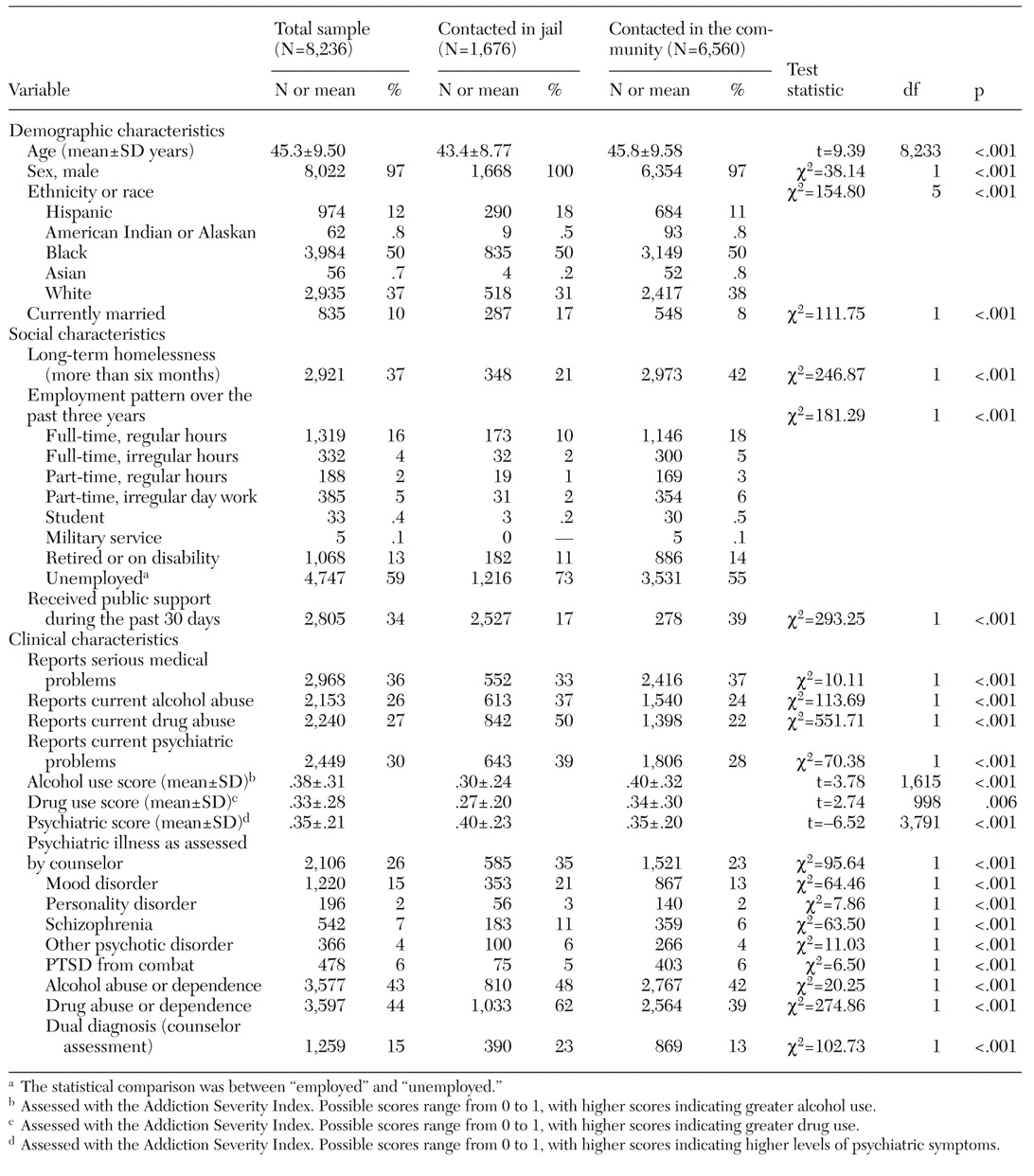
To examine these issues, we used national administrative databases maintained by the Department of Veterans Affairs (VA) to describe and evaluate outreach efforts by a large VA facility located near the Los Angeles County Jail. We compared the sociodemographic and clinical characteristics of 1,676 veterans who received outreach contact in jail and 6,560 homeless veterans who were contacted through community outreach and compared their patterns of service use and costs in the following year. We hypothesized that the veterans who were contacted in jail would have higher rates of service use and higher costs.
Methods
Sample
Since 1987, the VA has provided outreach services to homeless veterans nationally through the Healthcare for Homeless Veterans (HCHV) program. HCHV is focused on delivering three kinds of service: outreach and case management in community locations, linkage with medical and psychiatric services available at VA medical centers, and community contract residential rehabilitation treatment services (
10).
We identified all veterans who were contacted through the HCHV program at the VA Greater Los Angeles Healthcare System between May 1, 1997, and October 1, 1999. HCHV outreach staff assessed veterans in both community settings and in the Los Angeles County Jail. A structured intake instrument was used to assess sociodemographic and clinical characteristics of all veterans who were contacted and who appeared to be clinically appropriate for further involvement.
Assessments were based on face-to-face interviews in community locations and in the Los Angeles County Jail. VA outreach workers have developed a collaborative relationship with jail leadership and staff over the past 15 years. As required by VA policy, contacts with incarcerated veterans were limited to assessment and planning for postrelease community treatment. No formal VA medical services were delivered in the jail setting.
To ensure that the assessments represented new outreach contacts, we included only veterans who had two or fewer contacts with the HCHV program in the year before assessment. Service use and costs were assessed for one year after the assessment. Because the study involved secondary analysis of administrative data with no client identifiers, the institutional review board did not require informed consent.
Measures
Veterans' characteristics. The outreach workers collected demographic, clinical, and social adjustment information by using a standard assessment form. This intake form records sociodemographic characteristics; homelessness status; financial and employment status; medical, psychiatric, and substance dependence problems; and assessment and referral information provided by the outreach worker. Veterans who spent the previous night in a shelter or on the streets or who had no residence and were staying with family or friends were considered to be homeless.
Summary scores for alcohol and drug use and for psychiatric problems were based on the Addiction Severity Index (ASI) (
11). The alcohol score comprised two items that measured recent alcohol use, the drug score comprised two items that measured recent drug use, and a psychiatric score comprised eight items measuring recent psychiatric symptoms.
The outreach workers who completed the assessments were master's-level social work staff, paraprofessional social work staff, and nursing staff. The outreach workers recorded veterans' responses to questions about their psychiatric symptoms. The clinical assessments of the outreach workers were reviewed by licensed social workers, who determined whether the veterans had any psychiatric diagnoses. Clients were considered to have serious mental illness if a mood disorder, posttraumatic stress disorder, or schizophrenia or other psychotic disorder was documented. The presence of alcohol or drug abuse or dependence and any of the serious psychiatric disorders indicated dual diagnosis.
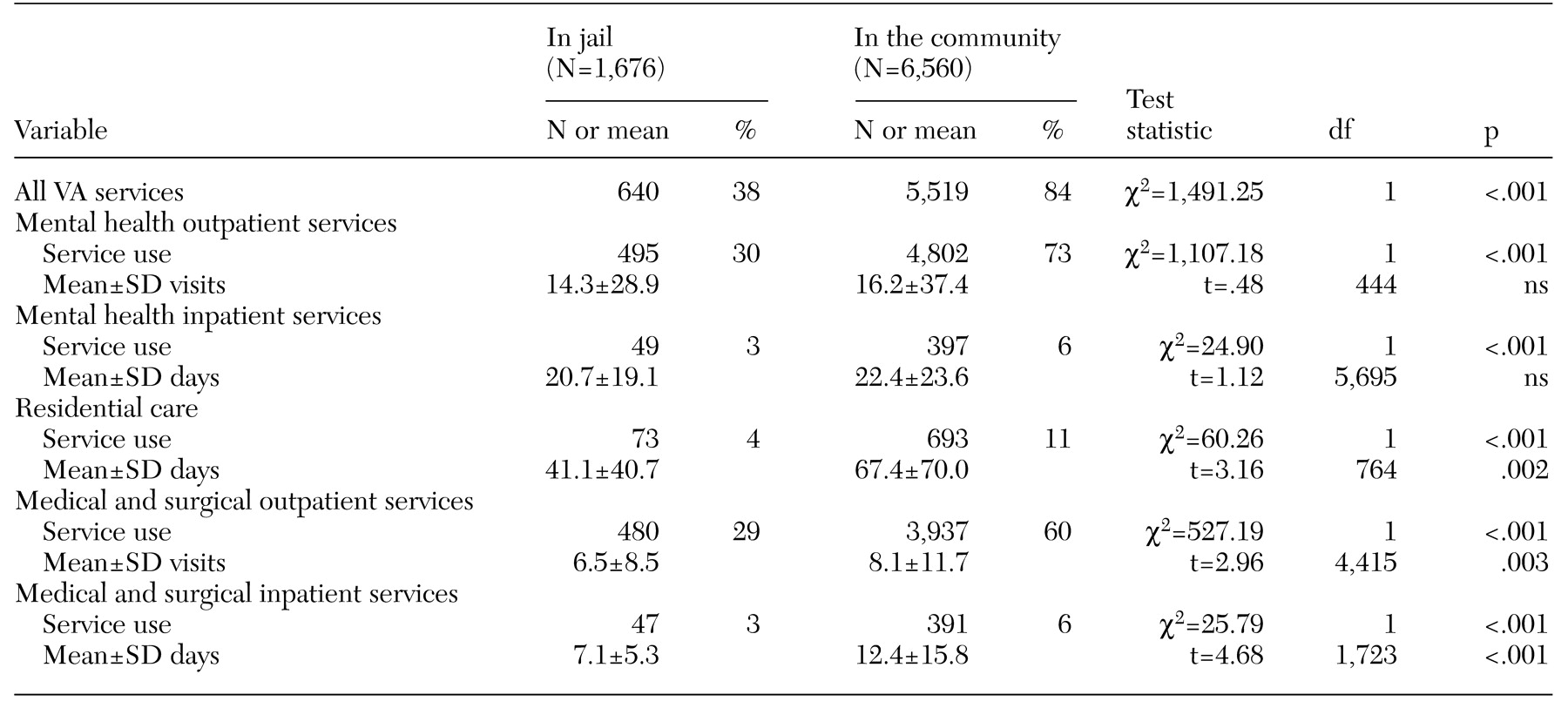
Service use. Data on service use during the year after the outreach contact were obtained from the VA's national computerized workload files, which document services provided at all VA facilities nationwide, not just at the VA Greater Los Angeles Healthcare System. These files include bed section codes, which identify each type of inpatient service and residential care, as well as admission and discharge dates of each episode of treatment. Outpatient codes are available that identify the date and type of clinic at which each outpatient service was provided. Using these codes, we clustered service use data into five categories: mental health outpatient care, mental health inpatient care, residential care, medical and surgical outpatient care, and medical and surgical inpatient care.
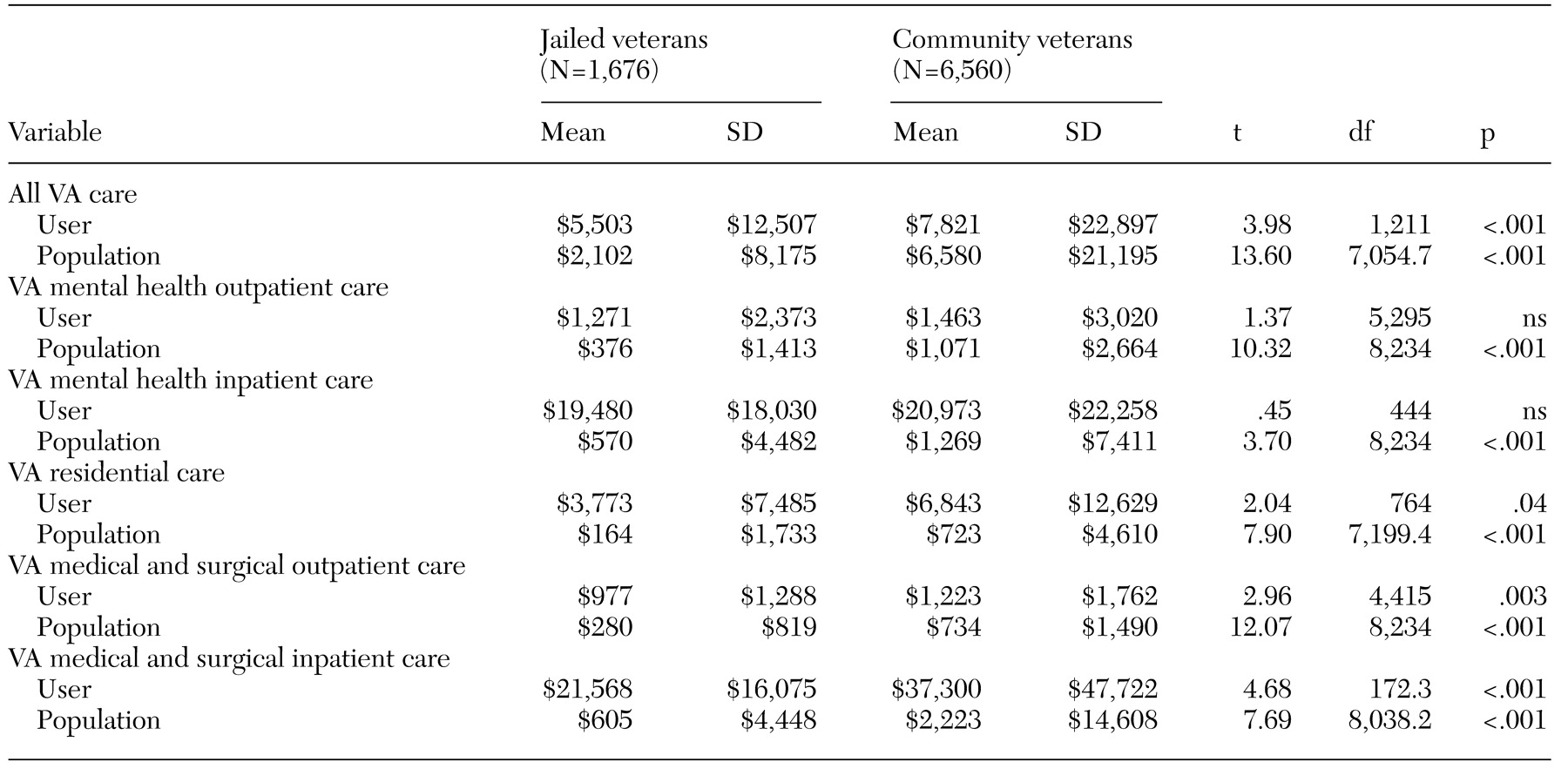
Service costs. Costs for inpatient, residential, and outpatient services were estimated by using the VA's fiscal year 2000 cost distribution report. The cost distribution report uses standardized accounting procedures to assign direct costs, such as clinical salaries and supplies, and indirect costs, such as administration, building maintenance, engineering services, equipment, and depreciation, to each health care program at each facility (
12). With two exceptions, local unit costs from the VA Greater Los Angeles Healthcare System's cost distribution report were used. National costs were used for services provided exclusively at other sites.
Analyses
The analyses proceeded in several steps. First, bivariate analyses were used to compare veterans who were contacted in the community with those who were contacted in the Los Angeles County Jail. Categorical data were compared by using chi square tests, and continuous variables were compared by using t tests.
Next, differences in service use were evaluated by using a two-stage procedure. Receipt of any VA services and receipt of each type of service were compared between the two groups by using chi square tests; t tests were then used to examine differences in the level of use among veterans with any service use for each type of service. We also used multiple logistic regression to control for potentially confounding sociodemographic and clinical characteristics.
Finally, we examined differences in the costs of services. We used t tests to determine the significance of differences in costs for any VA service and for each type of VA service between veterans in the two groups who used services. Similarly, to summarize the cost impact of the outreach, t tests were used to test for differences in average costs for all VA services and for each type of service across all clients in each group, including those who had not used services. The significance level for all analyses was set at .05.
Discussion and conclusions
This study sought to identify distinctive sociodemographic and clinical characteristics of veterans who received outreach contact in jail or in community settings and to test the hypothesis that veterans contacted through a jail outreach program would have higher service use and costs than homeless veterans who were contacted through outreach in community settings. At the time of the intake assessment, the veterans who were contacted in jail were more likely to have been unemployed over the previous three years and to have higher levels of both substance abuse and mental illness. Our hypothesis that service use and costs would be higher for these veterans was not supported—the jailed veterans used fewer VA services and had lower costs during the year after outreach contact than the homeless veterans who were contacted in community settings.
Although the veterans who were contacted in jail were better off as a group in terms of marital status and homelessness, they had very high rates of unemployment over the previous three years, even compared with a group of veterans who would be expected to have much higher unemployment rates than those in the general population. When veterans who were not available for work—for example, those who were disabled or retired—were removed from both samples, the unemployment rates were even higher: 83 percent for veterans contacted in jail and 64 percent for homeless veterans contacted in the community.
There are several possible explanations for these findings. First, in the case of veterans who had been incarcerated previously, stigma associated with having been in jail may have prevented employment, an explanation consistent with O'Flaherty's (
4) hypothesis on attenuation of community ties. Alternatively, these very high unemployment rates may have been due in part to substance abuse or individual skill deficits. Still another possibility is that the jailed veterans had a high rate of long-term incarceration that would explain their high unemployment rate. However, data on the duration of incarceration were not available to enable this possibility to be evaluated.
The high levels of psychiatric and substance use problems among the jailed outreach clients were as serious as the high unemployment levels. One in three had a diagnosis of a serious mental illness, and one in two reported current drug abuse. Although these levels are not dramatically higher than rates found in other studies of homeless populations (
5,
14), these findings—coupled with the three-year unemployment pattern—demonstrate the seriousness of the challenges faced by jailed outreach clients as they reenter the community as well as by the community providers who attempt to assist them.
One area of hope is the fact that the rate of current alcohol and drug use was lower in the jailed group, which suggests that jailed veterans may be more open to engagement in treatment at the time of outreach contact. Even though the jailed veterans in this study had had shorter periods of homelessness than the veterans from the community, it has been shown that jailed veterans with substance use problems frequently lack stable housing (
15) and are likely to require substance abuse services with a residential component.
The lower use of medical services in the incarcerated group is consistent with this group's lower level of self-reported medical problems. However, given the high levels of need for mental health services among the jailed veterans, it might be expected that access to and use of VA services by this group would be higher than in the community homeless group. But this was not the case. The jailed group was only a quarter as likely to obtain services, even after adjustment for many other potentially confounding variables.
Another possibility is that the observed differences in use were due to differences in VA service eligibility between the two groups (
16). To evaluate this possibility, we assessed eligibility in a random sample of 100 veterans from each of the two groups. No significant differences in eligibility rates were found (78 percent in the community group and 80 percent the incarcerated group). In addition, there were no significant differences in whether the veterans had service-connected disabilities, which is an indicator of service access priority; 8.3 percent in the community homeless group and 7.5 percent in the incarcerated group had service-connected disabilities.
A third possible explanation for differences in service use is that the jailed veterans had a higher rate of drug abuse or dependence and were more treatment resistant. As noted above, differences in service use remained after adjustment for this clinical difference.
Still another possibility is that outreach workers planned more frequently to refer jailed veterans to non-VA community treatment providers. When such plans were included in regression models predicting service use and costs, there was no change in the service use odds ratio and only a small decrease in total costs explained by outreach group (R2 change=.002, p<.001). Outreach workers' intentions to refer veterans to non-VA services thus did not explain differences in VA service use or costs.
Several other service and institutional variables could also explain lower levels of access to postrelease services. Services that inmates receive while incarcerated may reduce their need for community services. Jail staff may be unwilling or unable to inform case managers of when inmates are to be released from jail, thus preventing linkages with community services (
7). Transportation may not be available. Community service providers may not be enthusiastic about serving former inmates (
5). Data were not available to assess differences in rates of access that might arise from these factors.
A final important variable is that some veterans might have had lower levels of service use and cost a year after assessment because they were still incarcerated. We did not have access to jail release dates, so it is unclear how large a role this factor may play.
Cost differences between the two groups of veterans are more likely to be explained by differences in access to services than by differences in need. Although intake data suggest that the veterans who were contacted in jail had lower levels of need for medical services—corresponding to lower medical and surgical costs—these veterans had higher levels of need for mental health services yet lower mental health costs. Lower population costs for the jailed group across all cost categories could reflect indifference or fear on the part of the receiving programs or service providers.
Our findings on employment and service use, as well as the generalizability of the results, have several limitations. First, incarceration and release dates in criminal justice records are necessary for determining more clearly the relationship of long-term incarceration to both the long-term unemployment and the lower levels of service use observed in our sample.
A second limitation is that we studied male veterans—many of whom were homeless—who were receiving VA outreach services in one large city. This limits the generalizability of the study findings to the larger population of homeless or incarcerated people, although previous studies have shown few differences between homeless veterans and other homeless men (
17,
18).
The results of this study do suggest that much is yet to be learned about outreach interventions for incarcerated people who are soon to be released into the community. Given the clinical and rehabilitation needs we have identified, the lower rate of access to services might be responsive to the use of the motivational interviewing intervention (
19,
20) now being tested for engaging inmates with substance use problems in treatment. Given the complexity of institutional and service access problems that may interfere with linkage, jail outreach that emphasizes an extended duration of involvement by outreach workers for as long as it takes to get the clients linked to services has been shown to increase effectiveness (
8).
Outreach can provide social bridging or support that O'Flaherty (
4) suggests may be especially lacking for inmates who are reentering community life. From a policy perspective, the findings of this study are a mixture of "good news and bad news." From one perspective, providing outreach services seems to connect some members of the jail population with needed services, and the resulting service use and increased cost burden are not likely to overwhelm health care system resources. Medical center administrators could thus comfortably support this kind of initiative.
From another perspective, among veterans who received outreach services in jail, a relatively small proportion actually followed through with VA services. In the absence of an experimental design, we cannot confidently attribute their use of services to the outreach effort. From this perspective, the gains from this outreach effort remain uncertain. Developing more effective methods of service linkage and more thorough evaluation of the impact of these services on clinical, functional, and criminal justice outcomes are important next steps in enhancing community treatment for offenders with mental illness.