At 1:57 a.m. on September 21, 1999, an earthquake measuring 7.3 on the Richter scale devastated Nantou county and the surrounding areas of middle Taiwan. The earthquake affected an area of at least 5,000 square kilometers and caused at least 2,349 deaths and more than 20,000 injuries. Although Taiwan is often subject to natural disasters, the psychiatric effects on disaster survivors have rarely been studied.
The estimation of psychiatric disorders shortly after the occurrence of a disaster is essential for implementing effective relief activities and establishing disaster epidemiology. However, few studies (
1,
2) have investigated the short-term psychiatric problems associated with disasters in the community. A recent community-based survey (
3) concluded that the sudden unexpected death of a loved one is the most important cause of posttraumatic stress disorder (PTSD). Among individuals who are exposed to traumatic stressors, several studies have examined risk factors for PTSD, including lower educational levels and feelings of numbness (
2) and stressful life events following a disaster (
2,
4). However, these effects have not been specifically investigated among bereaved survivors.
In this study we investigated the characteristics of a community-based group of bereaved survivors in the early stages after a disastrous earthquake. The aims of the study were to describe the postearthquake prevalence of acute psychiatric disorders cross-sectionally and to explore risk factors associated with the first and second most prevalent psychiatric disorders—PTSD and major depressive disorder.
Methods
Sampling was conducted in two townships: township A, located three kilometers from the earthquake's epicenter, and township B, located 25 kilometers from the epicenter. Each township had a population of around 20,000. In township A, there were 108 deaths related to the earthquake, and in township B, 137 deaths. The relatives of the dead belonged to 81 and 99 households, respectively. The study surveyed at least one immediate family member from each household if possible; a nonimmediate family member was surveyed if an immediate family member was unavailable. Several suitable study participants migrated outside the community after the earthquake. A total of 120 bereaved survivors belonging to 109 households were included in the final sample.
Psychiatric assessment of each study participant was conducted by a trained psychiatrist an average of two months (60±21 days) after the earthquake. The Chinese version of the Mini-International Neuropsychiatric Interview (MINI), originally designed as a short but accurate structured psychiatric interview (
5), was used to determine psychiatric diagnoses. The diagnostic criteria of the MINI are based on
DSM-IV. The Chinese version of the MINI has been tested and has good validity (
6). Eight board-certified psychiatrists, who together reviewed this instrument before the investigation, participated in the fieldwork. All the psychiatrists had completed the psychiatric training program at Taipei City Psychiatric Center. The study protocol was reviewed and approved by the local health care authority. Before a psychiatric interview was carried out, oral consent was obtained from each participant.
Demographic data collected included age, gender, educational level (at least primary school, or other), marital status (married or other), and the person's relationship to the victim (immediate family or other). Data on disaster-related circumstances, whether the study participant was present at the site of the earthquake, whether the participant had been injured, and initial emotional reactions after the earthquake were collected. Initial emotional reactions included feeling depressed or sad, anxious or frightened, guilty, and numb or "zombie-like" and experiencing disbelief or confusion (
2). A brief inventory (
7) was used to explore psychosocial stressors after the earthquake.
The risk factors for PTSD and major depressive disorder were examined on the basis of the demographic and earthquake-related variables with use of multivariate logistic regression analysis. This method was useful for estimating the presence or absence of a characteristic or outcome on the basis of values of a set of variables. The level of significance was set at .05.
Results
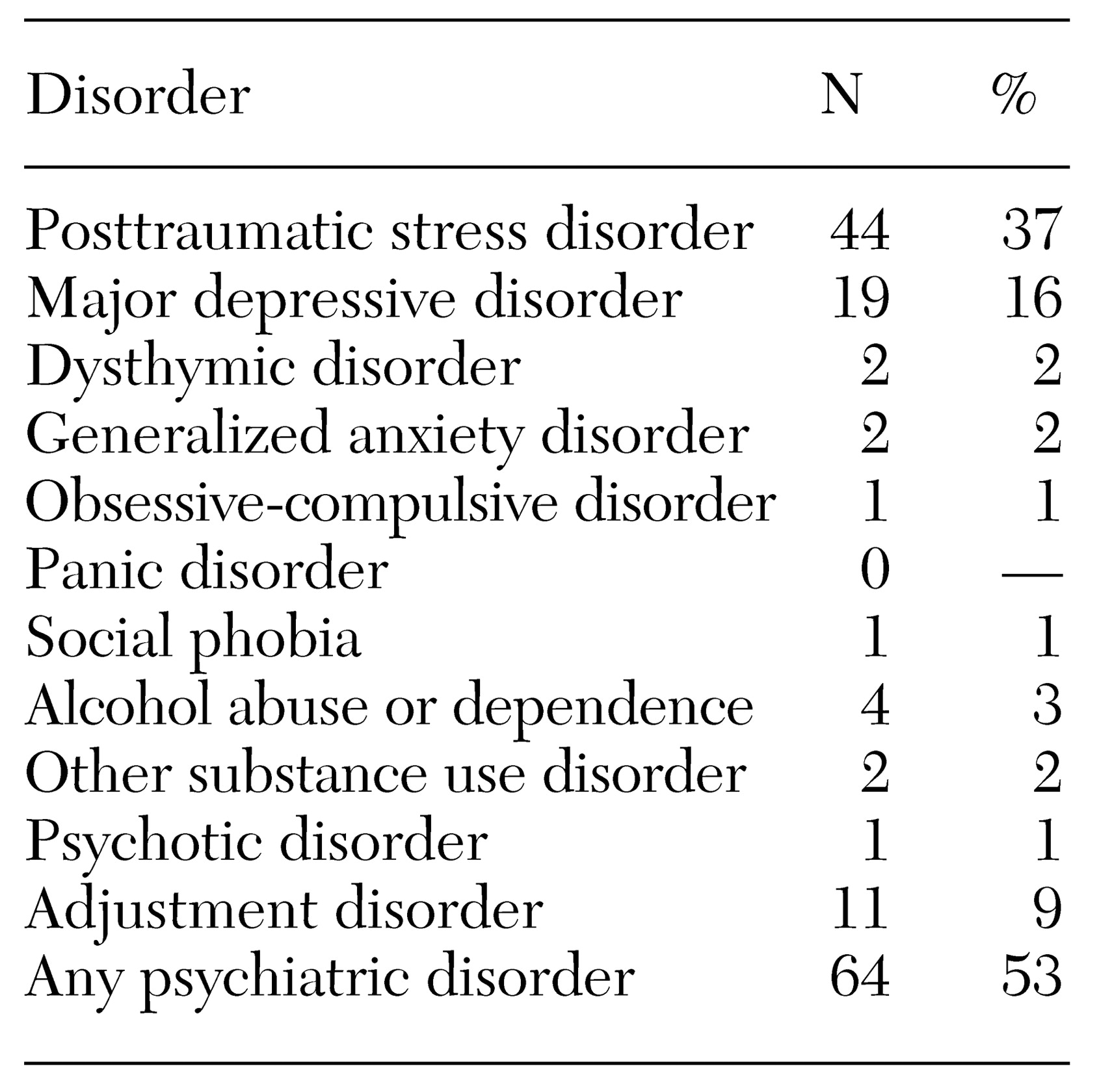
The mean±SD age of the 120 bereaved survivors was 54±17 years, with a range of 12 to 84 years. Seventy-three survivors (61 percent) were male. Sixty-four survivors (53 percent) met
DSM-IV criteria for psychiatric diagnoses after the earthquake, including PTSD (37 percent) and major depressive disorder (16 percent) (
Table 1). Among persons with any psychiatric disorder, those who had PTSD or major depressive disorder did not have these conditions until after the earthquake.
Further analysis revealed that the significant risk factors for PTSD were a greater number of psychosocial stressors (odds ratio [OR]=3.03, p=.002) and initial feelings of guilt (OR=3.69, p=.05). The significant risk factor for major depressive disorder was female gender (odds ratio=3.23, p=.02). Sources to which the survivors turned for help included their families, spiritual sources, and medical professionals. Most of the survivors (95 percent) lived with their family after the earthquake, and 52 (43 percent) sought spiritual help—for example, by participating in religious ceremonies. Fewer survivors (19, or 16 percent) sought help at primary care clinics.
Discussion and conclusions
In this group of bereaved survivors, we found that the rate of all psychiatric disorders was two times higher than that found in a previous community-based epidemiological study in Taiwan (
7) (53 percent compared with 26 percent). Although different instruments were used in the two studies, the findings of this study suggest that the etiology of disaster is an important factor in the occurrence of psychiatric illness. Moreover, a study in Taiwan by Liao and colleagues (
6), who used the MINI to investigate acute psychiatric morbidity among nonbereaved survivors located near the epicenter one month after this earthquake, showed a much lower prevalence of PTSD than in our study (7 percent). It is clear that the sudden trauma of bereavement may provoke the development of PTSD.
The bereaved women in our sample had a risk of developing major depressive disorder that was about three times that of the men, while the number of psychosocial stressors was not associated with the development of major depressive disorder. These findings are consistent with the results of a population-based study (
8) showing that female gender was correlated with the development of severe depression and that psychosocial stressors were correlated with the development of mild depression.
The participants in our study who developed PTSD were more likely to report that they felt guilt shortly after the earthquake. Thus a person's feelings of guilt could reflect the degree of grief and could be a marker for early detection. The finding about postdisaster stressors relating to PTSD is consistent with the results of previous research (
2,
4). For example, Yehuda and associates (
4) studied Holocaust victims and found an additive effect of recent stressful events on the severity of PTSD symptoms.
The earthquake in Taiwan was a central disaster, defined as a disaster that causes change in the entire physical and organizational structure of the community (
9). The trauma associated with such a disaster may continue for a relatively long period after the event, especially if there are subsequent stressors. Information about long-term trauma would have important clinical ramifications, because it may be possible to shelter bereaved survivors and help them to stabilize their lives and avoid subsequent stressors. However, it should be noted that the help-seeking behavior of people who suffer from PTSD and major depressive disorder in Taiwan is different from Western help-seeking behavior.
For example, in a study by Samson and colleagues (
10), most people with PTSD sought treatment in primary care settings. After the earthquake in Taiwan, only a quarter of persons with PTSD—and a similar proportion of persons with major depressive disorder—visited primary care clinics for help. This low rate of help seeking might have been due to the survivors' related symptoms—for example, social withdrawal—or may reflect an environment in which the survivors were overwhelmed by having to attend to other demands.
Our findings indicate a need for the development of a more effective outreach strategy. Meanwhile, people who have more psychosocial stressors, those with initial feelings of guilt, and women should be targeted for early intervention.
Acknowledgments
The authors thank Chun-Tse Chen, M.D., Chih-Lung Chien, M.D., and Chiang-Dan Chiang, B.Sc., for their effective organization in the assigned relief program as well as Ming-Chyi Huang, M.D., Kuan-Yu Chen, M.D., and Shir-Kai Liu, M.D., for their fieldwork.