Anxiety disorders are among the most common and costly mental health problems (
1,
2,
3,
4,
5). Treatment is commonly sought for anxiety disorders in primary care settings (
6), especially for panic disorder, because it often masquerades as physical illness (
7,
8). Unfortunately, anxiety disorders, including panic disorder, are often undetected in primary care settings (
9). Even when these disorders are detected, patients often do not receive guideline-concordant care (
10,
11,
12). This finding is not surprising given short primary care visits and competing demands of other illnesses and because many patients with anxiety disorders present primarily with somatic symptoms.
Unfortunately, there is no standard measure of "need" for mental health services, and hence there is no standard for "unmet need" (
13,
14,
15). One way to measure need is with instruments—such as the Structured Clinical Interview for DSM-IV (SCID) (
16) or the Composite International Diagnostic Interview (CIDI) (
17)—and this approach is the one taken in clinical trials, health services interventions, and community epidemiologic studies. However, although there is no consensus on what constitutes need, it is generally agreed that a CIDI or SCID diagnosis of a
DSM-IV disorder is not always tantamount to need for mental health services. An alternative method is to ask individuals whether they perceive a need for mental health treatment or whether they have unmet need for mental health services. Unfortunately, there has been little investigation of the overlap between these two methods. Perhaps the best example is from the National Comorbidity Survey. In that survey, Mojtabai and colleagues (
18) found that a minority of individuals with CIDI disorders perceived a need for mental health treatment, suggesting that many individuals who would benefit from mental health treatment do not perceive a need.
To our knowledge no studies have investigated the relationship between CIDI diagnosis and perceived or unmet need for mental health treatment among patients from primary care settings. Our first aim was to evaluate perceived unmet need for mental health problems among individuals in the primary care setting who were given a diagnosis of panic disorder according to the CIDI. Second, we assessed the extent to which predisposing, enabling, and need factors were associated with perceived unmet need (
19,
20,
21). Parslow and Jorm (
20) extended this framework, adding the degree of contact with health services, because such contact is likely to affect the extent to which individuals perceive their needs as being met. Unexpectedly, their Australian data showed that contact with a general health practitioner positively predicted endorsement of unmet need for information about mental health. The degree of contact with health services was included in the study presented here.
We hypothesized that the greater the need for mental health care, the more likely it would be that some needs would be reported as unmet. Also, we hypothesized that individuals with fewer enabling factors would be more likely to endorse unmet need. The role of predisposing factors of age, gender, racial status, and disability status (as a proxy for "plaintive set") was examined in a more exploratory fashion. Finally, despite the findings from Parslow and Jorm's study (
20), we hypothesized that greater contact with health care services would be associated with less unmet need.
In addition, we investigated barriers to care from the patient's perspective. Barriers to treatment are multifactorial and likely include poor understanding of the disorder and its treatment among the general public, individuals with panic disorder, and health care providers; mental health stigma; and poorly organized and inadequately funded health care systems (
21). Information about barriers from the patient's perspective may assist us in developing effective policies to decrease unmet need. In previous studies, financial reasons and social stigma are commonly cited barriers (
22), with financial reasons especially prominent among persons who are uninsured (
23). Thus we hypothesized that cost and social stigma would be cited as primary reasons for unmet need.
Methods
Participants
Participants were from a clinical trial that investigated the treatment of panic disorder in primary care settings. Data presented here are from the baseline interview. Recruitment was from March 2000 to March 2002. Participants were recruited from two university-affiliated primary care clinics in each of three cities: Seattle, San Diego, and Los Angeles. The internal medicine and family medicine clinics were staffed by board-certified attending physicians, with some care delivered by residents in training. Participants were included for our study if they were 18 to 70 years old, had current panic disorder with or without agoraphobia according to DSM-IV criteria, had at least one panic attack in the past week, were willing to accept treatment involving a combination of pharmacotherapy and cognitive behavioral therapy, were able to speak English, and had a telephone. Participants were excluded if they received psychiatric disability benefits and if they were already seeing a psychiatrist or a cognitive-behavioral therapist.
Participants were recruited in clinic waiting rooms by using a two-question panic disorder screen (
24) and physician referrals. All patients who screened positive for panic disorder and those who were referred were given a telephone diagnostic interview, the CIDI (
17), to determine diagnostic eligibility. Before patients were randomly assigned to active treatment (cognitive-behavioral therapy plus medication recommendations) or treatment as usual, they completed a telephone baseline assessment that included questions about distress factors, perceived barriers to mental health care, mental and health care use, and other indices listed below.
Written informed consent was obtained from study participants. This study was approved by institutional review boards at the University of Washington, the University of California, Los Angeles, and the University of California, San Diego.
Outcome variables
We investigated unmet need with questions developed for Healthcare for Communities (
23). Items were scored 1, for yes, or 0, for no. Participants were asked, "During the past three months, was there any time you did not get as much care for emotional or personal problems as you needed or had delays in getting care?" Patients answering affirmatively were coded as having unmet need and were asked whether 13 perceived barriers to adequate mental health treatment applied to them. Specifically, they were asked "What were the main reasons you did not get as much help as you needed or had delays in getting care? Was it because…."
Predictor variables
A broad range of physical and mental health measures of patient need were assessed, including comorbid diagnosis of social phobia; comorbid diagnosis of posttraumatic stress disorder; the mental health score from the Short-Form Health Survey (SF-12) (
25); the global physical health score from the SF-12; the Anxiety Sensitivity Index scores to measure the tendency of the patient to be concerned about anxiety symptoms (
26); the total sum of avoidance items on the Marks and Matthews's Fear Questionnaire (
27); any full panic attacks in the past week; worry about panic over the past month (rated from 0, no worry, to 4, extreme worry); scores on the Center for Epidemiological Studies-Depression Scale (CES-D) (
28); any work days missed during the past three months; any late arrivals at or early departures from work in the past three months because of illness or doctor's visits; the neuroticism subscale score of the NEO Personality Inventory (
29); and disability, ascertained from five items selected from the World Health Organization Disability Scale (WHODAS) (
30). The five WHO items possessed high internal consistency in our sample (alpha=.78).
Enabling factors were assessed by using income (the lower third, the middle third, and the top third of our distribution), insurance status (Medicare, Medicaid, other public or private insurance, and uninsured), sick pay available for days off when ill (yes or no), education (less than 12 years or 12 or more years), and employment (less than 40 hours per week or 40 or more hours per week).
Proxies for predisposing factors included gender, age, and racial status (white or nonwhite). The degree of contact with health services included hospitalization for physical or emotional reasons during the past three months, an emergency department visit during the past three months, more than one physician visit during the past three months, and any mental health visits during the past three months.
Statistical approach
After descriptive statistics of endorsement of unmet need, multiple logistic regression analyses were used to investigate predictors of patient-perceived unmet need, with predictor variables measuring predisposing, enabling and need factors and the factor that described the degree of contact with health services. Because many of the predictor variables were highly correlated, a forward stepwise selection method was used; the strongest predictors of unmet need among our ensemble of need—predisposing, enabling, and contact with health services—were selected. All variables for which p≤.05 were included. The final stepwise model was further investigated for interaction effects. After descriptive analyses of perceived barriers to mental health needs, a factor analysis was conducted to group the 13 perceived barriers into meaningful domains. Estimates were calculated by using SAS Version 9.1. Given the exploratory nature of this investigation, a Bonferroni correction was not deemed necessary.
Results
Participants
A total of 11,364 patients were contacted about the study, and 7,477 (66 percent) were given the two-question panic disorder screen. Among those screened, 2,546 (34 percent) screened positive for panic disorder, and 618 (24 percent) of these were eligible for the study. Major reasons for exclusion included unwillingness to take medication (839 participants, or 33 percent), unwillingness to meet with a behavioral health specialist (749 participants, or 29 percent), no recent panic spell (337 participants, or 13 percent), current treatment by a psychiatrist (279 participants, or 11 percent), or refusal to participate in the study (256 participants, or 10 percent). Participants could have more than one reason for exclusion. We were able to reestablish contact with 416 patients who agreed to be interviewed. The various screening variables did not differ between eligible participants who were interviewed and the 202 eligible participants who were not interviewed. Among those interviewed, 231 (56 percent) tested positive for panic disorder and were eligible for our study.
Unmet need
Among the 231 individuals with panic disorder who were eligible for our study, 88 (38 percent) endorsed unmet need (defined as a patient report of insufficient or delayed treatment) for emotional or mental health problems.
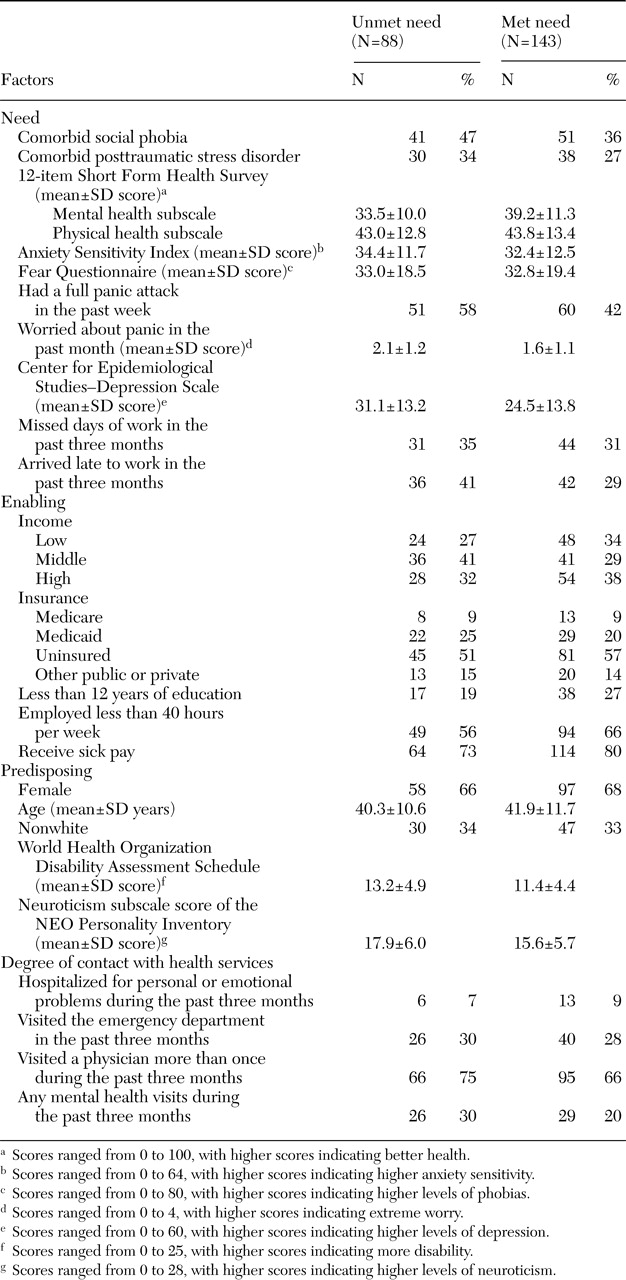
Table 1 presents descriptive statistics for patients who endorsed unmet need and those who did not. Among persons who endorsed unmet need, only 11 (12 percent) reported that over the past three months they had not received any treatment for emotional problems (that is, any antipanic medication, hospitalization for personal or emotional problems, a medical provider visit in which they asked about personal or emotional problems, or a mental health provider visit); the corresponding number among those who did not endorse unmet need was 46 patients (32 percent). Among patients with unmet need, 46 (52 percent) had received adequate antipanic medication, five (6 percent) had received adequate cognitive-behavioral therapy for panic disorder (defined as four or more cognitive-behavioral therapy sessions), and three (3 percent) had received both adequate antipanic medication and adequate cognitive-behavioral therapy in the past three months. The proportion of patients who were uninsured did not differ between those who endorsed unmet need and those who did not (12 patients who reported unmet need, or 14 percent, compared with 21 patients who did not report unmet need, or 15 percent).
Predictors of unmet need
The logistic regression analysis was conducted for the 226 individuals with no missing data (85 with unmet need, 141 without). With the predictors taken one at a time, several measures of mental and physical health were significantly associated with reported unmet need. These included full panic attacks during the past week (odds ratio [OR]=1.91, 95 percent confidence interval [CI]=1.11 to 3.27, p=.02), worry about panic attacks (OR=1.55, CI=1.22 to 1.97, p<.001), and level of depressed mood, as measured by the CES-D (OR=1.04, CI=1.02 to 1.06, p=.001). The neuroticism subscale of the NEO Personality Inventory (OR=1.07, CI=1.02 to 1.13, p=.003) and the WHODAS (OR=1.09, CI=1.03 to 1.15, p=.005) were also significantly associated with unmet need. Additionally, higher mental health scores from the SF-12 were significantly associated with fewer reports of unmet need (OR=.95, CI=.93 to .98, p<.001).
Of more interest is the multivariate effect of these variables. Because of a strong correlation between scores on the mental health subscale of the SF-12 and WHODAS scores, presence of panic attacks, CES-D score, and score on the neuroticism subscale of the NEO Personality Inventory, these variables were not significant in the multivariate models that included the mental health subscale of the SF-12. Instead, as shown in
Table 2, two need variables and one enabling variable predicted unmet need. Specifically, individuals with worse mental health on the mental health subscale of the SF-12, those who were more worried about panic, and those who did not have sick pay were all significantly more likely to report unmet need. There is no clear reason why receipt of sick pay was not significant in the bivariate analyses, except that the data sets were slightly different because of different numbers of missing cases compared to the multivariate analyses.
Perceived barriers
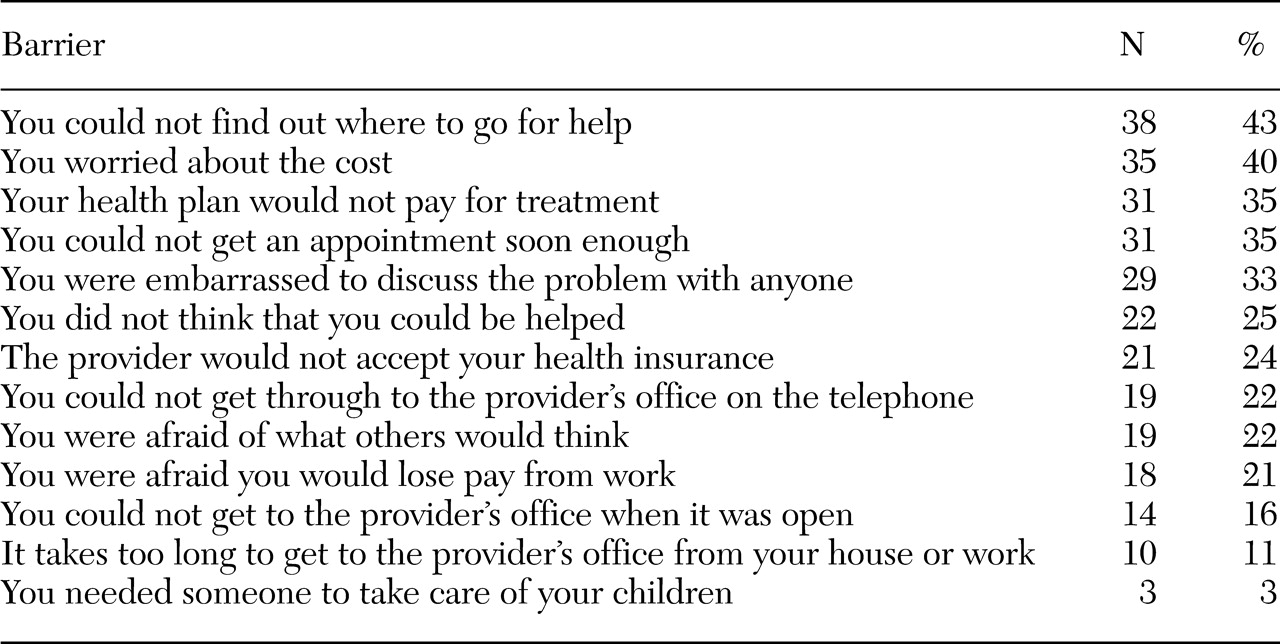
As shown in
Table 3, the most commonly reported barriers were inability to find out where to go for help, cost, lack of coverage by the health plan, and waiting time for an appointment. Among the 38 patients who did not know where to get help, 35 had visited a medical provider in the past three months. Patients for whom cost was a barrier to treatment were more likely to be uninsured (12 patients, or 34 percent) than those not who did not endorse cost as a barrier (one patient, or 2 percent) (χ
2=19.0, df=3, p<.001).
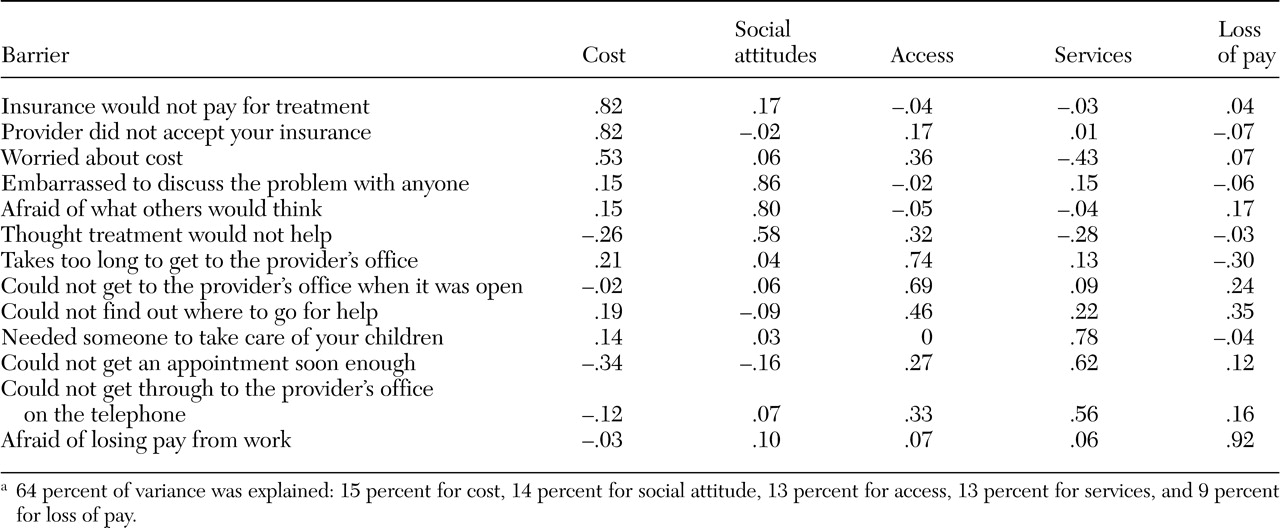
To investigate whether subgroups or factors of reasons existed, a principal components analysis was used to extract five components with eigenvalues greater than 1.0 followed by a varimax rotation. The analysis used the correlation matrix with 1s (items scored as yes) on the diagonal. One respondent for whom an item was missing was excluded. As shown in
Table 4, on the basis of factor analysis, perceived barriers fell into five groups: cost, social attitudes, access, services, and loss of pay. The factor analytic approach was chosen over a previous scale construction that was based on conceptual domains of cost (lack of coverage by health plan, provider's refusal to accept patient's health insurance, worry about cost, and fear of loss of pay from work), social concerns (embarrassment about discussing the problem, fear of what others would think, and belief that one could not be helped), and practical concerns (unable to find out where to go for help, unable to get an appointment soon enough, unable to get to the provider's office when it was open, distance to the provider's office, and inability to get through to the provider's office by telephone). The factor analytic approach was chosen because the cost factor scale yielded a higher Cronbach's alpha (.70) than the a priori cost scale (.55), even though the access and services factor scales yielded somewhat lower Cronbach's alphas (.52 and .56) than the a priori scale on practical concerns (.62).
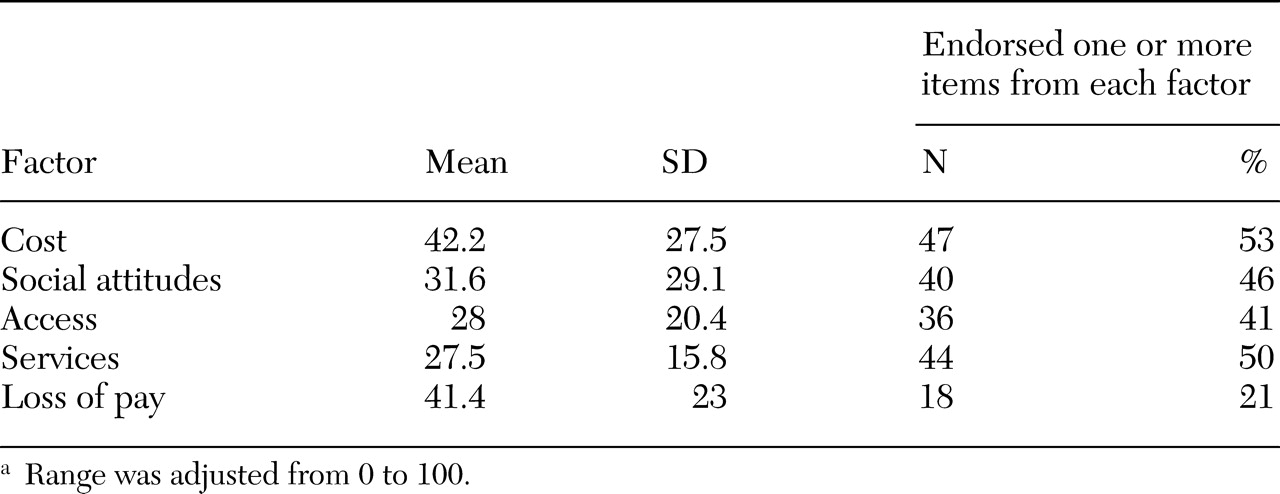
Table 5 presents the weighted sum for each factor score (weighted from 0 to 100) and the percentage of respondents who endorsed at least one barrier item from each factor. The factor most often endorsed was cost.
Discussion
Thirty-eight percent of our primary care sample of patients with panic disorder reported unmet need for mental health or emotional problems. This percentage is surprisingly low because individuals in our sample had current panic disorder by
DSM-IV criteria, with at least one panic attack in the past week; they were willing to accept treatment for panic disorder; the process of enrollment in a clinical trial may have sensitized some of our clinic patients to their unmet need; and those most likely to be receiving high-quality care (those in mental health specialty treatment) were excluded from our study. Nevertheless, this relatively low level of patient-reported unmet need is consistent with Mojtabai and colleagues' (
18) analysis of National Comorbidity Survey data, in which a majority of patients with mental health disorders did not perceive a need for treatment. Both our study and the study of Mojtabai and colleagues demonstrate the discrepancy between
DSM-IV measures of mental illness and patient reports of need for treatment, and they highlight the need for more studies of the complex relationship between CIDI diagnosis, self-reported need, and use of services.
There are several possible reasons for the discrepancy between CIDI diagnosis and reports of unmet need. First, many individuals who entered our study had already been receiving some form of mental health treatment, and perhaps for this reason they reported no unmet need. However, many were not receiving adequate care, when a liberal definition of adequate care was used. Individuals with panic disorder who perceived no unmet need may not have realized that they had a mental health problem or that efficacious treatments were available, or they could have been in denial about their mental illness. Finally, a CIDI diagnosis of panic disorder is not necessarily tantamount to unmet need for services.
Our finding that fewer than four in ten individuals with current panic disorder who were enrolled in a clinical intervention perceived an unmet need for services suggests that failure to perceive a need for treatment may be an important barrier to care. Furthermore, although it is beyond the scope of this report, failure to perceive a need for treatment among patients in mental health treatment may lead to worse outcomes.
Reassuringly, patient-reported unmet need was consistently predicted by two measures of need—the mental health subscale of the SF-12 and worry about panic attacks—with more distressed individuals more likely to endorse unmet need. Only one enabling factor, paid sick time from work, was associated with decreased unmet need. None of our predisposing proxy variables or degree of contact with health services predicted unmet need. Although these findings are restricted to a sample with reasonable access to care by virtue of being in primary care, they replicate results from the Australian National Survey of Mental Health and Wellbeing (
20). That is, need variables most consistently predicted unmet need and enabling variables to a certain degree.
Our findings about barriers provide directions for interventions designed to decrease unmet need in primary care. Respondents reported substantial difficulty in making a mental health care appointment; 43 percent could not find where to go for help (the most commonly cited barrier, and possibly indicative that their primary care providers did not provide mental health treatment referral information), 22 percent could not get through to the provider's office on the telephone, and 35 percent could not get an appointment soon enough. In addition, two measures of stigma—whether the respondent would be embarrassed to discuss the problem with anyone and whether the respondent would be afraid of what others might think—were endorsed by 33 percent and 22 percent of the sample, respectively. Economic barriers also were commonly endorsed; 53 percent endorsed at least one reason related to cost as a barrier. This finding agrees with previous research that consistently cites access to services and stigma as important barriers to mental health care (
21).
Our results imply that increasing awareness of mental health resources, improving initial telephone access to services, and establishing more timely appointments may be as critical in diminishing unmet need as decreasing stigma or economic barriers. We believe that this finding is encouraging, because education about where to go for mental health treatment and improvements in appointment scheduling might be easier to implement than decreasing stigma or economic barriers to mental health treatment.
Conclusions
Our results highlight the relatively low level of patient-reported unmet need for mental health treatment among patients with panic disorder in the primary care setting. Our results suggest that efforts to improve primary care treatment of panic disorder should include patient education about mental illness and the effective treatment available. Furthermore, although discussion of barriers to care has traditionally centered on stigma and economic factors, our results suggest that simple logistic factors, such as not knowing whom to call for help and not being able to get through on the telephone, are also important barriers that can be more readily dismantled.
Acknowledgments
This study was supported by grants MH-58915, MH-57858, MH-065324, MH-57835, and MH-64122 from the National Institute of Mental Health.