The literature on potential racial differences and disparities in rates of trauma exposure and posttraumatic stress disorder (PTSD) among veterans has focused on prevalence, clinical manifestation, and outcomes. The National Vietnam Veterans Readjustment Survey showed that African-American and other minority combat veterans have higher rates of PTSD than Caucasians but that these differences disappear when factors such as level of combat and preexisting trauma are controlled for (
1). Other studies have explored racial differences among combat veterans with PTSD on clinical symptom patterns by using psychometric instruments, psychiatric interviews, or retrospective chart reviews.
Together, these studies suggest that African-American and Caucasian veterans with combat PTSD do not differ much in manifestation or severity of psychopathology (
2,
3). However, most previous studies relied on symptomatic clinical samples, which limited the generalizability of findings. Furthermore, few studies have examined racial differences in use of medical and mental health services among combat veterans, and the limited available data are inconclusive. Some studies did not show differences in medical and mental health use (
3), whereas others presented evidence that African-American veterans are more likely to underutilize mental health services (
4) and more likely to use medical services compared with other ethnic groups (
5).
Thus it is not clear whether there are meaningful racial differences in trauma exposure, PTSD prevalence, psychiatric comorbidity, functional status, or use of VA services and benefits among general veteran populations served by the VA. The study reported here aimed to compare African-American and Caucasian veterans across these variables, with particular emphasis on racial differences in psychopathology and service use. Comparisons were made within a large primary care sample of veterans as well as a subsample of veterans with PTSD.
Methods
Study participants were randomly selected from a master list of patients from four southeastern VA medical centers (
6) during fiscal year 1999. After providing written informed consent, participants completed a semistructured clinic assessment and within two months were administered a structured telephone interview. We also conducted a blind 12-month retrospective review of participants' VA treatment, including psychiatric diagnoses and service use. This study was conducted with institutional review board approval.
A total of 1,198 randomly identified veterans were approached for study participation in one of four VA primary care clinics. Of this sample, 885 (74 percent) consented to participate. Follow-up phone interviews were obtained for 747 (84 percent) of the 885. Because of missing data on primary instruments or exclusions based on race (six veterans were excluded because they identified as Hispanic, American Indian, or other), the sample was further reduced to 713 (81 percent). The primary care sample included all 713 veterans, and the PTSD sample included 84 veterans (12 percent).
The Short-Form Health Survey (SF-36) (
7) is a 36-item self-report measure of several health domains that yields two composite scores reflecting global physical and mental health functioning. According to scoring guidelines, raw scores were converted for placement on a scale of 1 to 100, with higher scores reflecting greater health or functional status. The SF-36 has been shown to be a valid and reliable instrument for use with veteran populations.
The self-report version of the Trauma Assessment for Adults (TAA) (
8) assesses the lifetime incidence of trauma and has been widely used to screen community and medical populations for trauma history.
To obtain current PTSD diagnoses, the Clinician Administered PTSD Scale (CAPS) (
9) was administered to participants who endorsed a traumatic event on the TAA. Possible CAPS scores range from 0 to 136, with higher scores reflecting more severe symptoms. The CAPS is one of the most widely used structured interviews for assessing
DSM-IV PTSD.
The Mini International Neuropsychiatric Interview (MINI) (
10) is a brief structured interview that assesses the criteria for
DSM-IV axis I diagnoses. The MINI exhibits similar sensitivity and specificity to more time-intensive structured psychiatric interviews and was used to obtain current psychiatric diagnoses.
Chi square or Fisher's exact tests were used to compare African Americans and Caucasians on categorical demographic variables (gender, education, and employment status). An independent-samples t test was used to examine racial differences in age. For both the primary care and PTSD samples, racial differences in trauma variables were examined by using unadjusted and age-adjusted logistic regression analyses for dichotomous outcomes (for example, trauma exposure and PTSD diagnoses from the CAPS and chart review) and analyses of variance or age-adjusted analyses of covariance for continuous outcomes (for example, PTSD severity). The presence of other psychiatric diagnoses, functional status, service use, and disability benefits was analyzed by using a similar strategy. An alpha value of .05 (two-tailed) was used for all analyses.
Results
Comparisons between the final sample (N=713) and participants who could not be reached for follow-up interviews (N=138) on sociodemographic variables yielded a significant difference only for age, with older veterans (mean±SD age of 61.17±11.88 years) more likely to complete the follow-up than younger veterans (58.85±3.20) (F=4.23, df=1, 845, p=.04).
The mean±SD age of the primary care sample (N=713) was 61.19±11.88 years; 665 (93 percent) were male, 157 (22 percent) had less than a high school education, 204 (29 percent) had a high school diploma, and 352 (49 percent) had attended at least some college. A total of 237 veterans (33 percent) were employed, and 322 (45 percent) had a service-connected disability. The racial breakdown of the sample was 65 percent Caucasian (N=460) and 35 percent African American (N=253). No significant racial differences emerged on categorical demographic variables. However, significant group differences emerged on age, with Caucasians being older than African Americans (mean age of 63.86±11.05 compared with 56.35±11.81 years; t=-8.47, df=710, p<.001).
A total of 645 veterans (91 percent) had experienced at least one trauma, with no significant age-adjusted or unadjusted racial differences in the likelihood of endorsing a trauma. In unadjusted analyses, no significant racial differences in trauma exposure emerged. However, after adjustment for age, Caucasians were more likely to endorse childhood sexual abuse (32 of 433, or 7 percent, compared with nine of 233, or 4 percent; odds ratio [OR]=.33, 95 percent confidence interval [CI]=.15 to .73, p=.01). Caucasians also reported a greater number of traumatic events in their lifetime (2.63±1.73 compared with 2.51±1.87, F=4.18, df=1, 702, p=.04).
Eighty-four veterans (12 percent) met diagnostic criteria for PTSD on the CAPS, with no significant racial differences in rates of PTSD diagnoses or in PTSD severity. Fifty-one veterans (7 percent) had a chart notation of PTSD, with no significant age-adjusted or unadjusted racial differences in chart notation.
On the basis of unadjusted values, African Americans were more likely to have a diagnosis of dysthymia and substance abuse or dependence than Caucasians (for dysthymia, 42 of 253, or 17 percent, compared with 49 of 458, or 11 percent, OR=1.66, CI=1.07 to 2.59, p=.03; for substance use disorders, 16 of 253, or 6 percent, compared with nine of 458, or 2 percent, OR=3.37, CI=1.47 to 7.74, p<.01). After adjustment for age, racial differences in dysthymia were nonsignificant, whereas the significant differences in substance abuse or dependence remained (OR=2.48, CI=1.04 to 5.92, p=.04). No group differences emerged on either the mental or physical health composite scores on the SF-36.
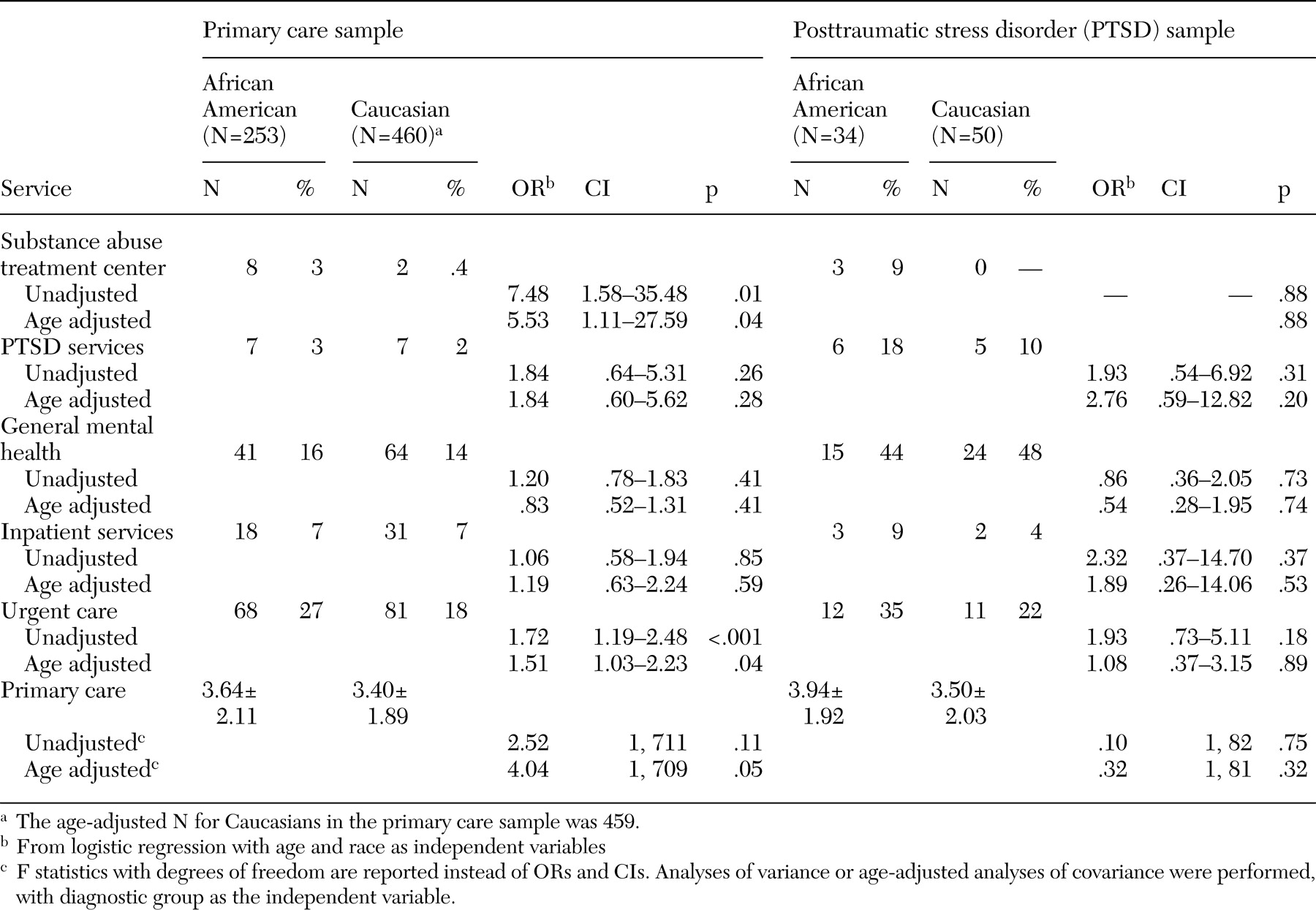
When unadjusted and age-adjusted scores were used, African-American veterans were more likely to have used a substance abuse treatment center and to have had an urgent care visit than Caucasian veterans (
Table 1). No significant age-adjusted or unadjusted racial differences emerged in the likelihood of receiving VA benefits.
The sample characteristics and the pattern of demographic differences between African Americans and Caucasians in the PTSD sample (N=84) were similar to those in the primary care sample. That is, Caucasians in the PTSD sample were significantly older than African Americans (61.09±11.41 compared with 51.61±6.86 years; t=-4.75, df=81, p<.001).
After adjustment for age, African Americans were more likely than Caucasians to have had combat exposure (31 of 34, or 91 percent, compared with 41 of 50, or 82 percent; OR=7.45, CI=1.33 to 41.80, p=.02). No other significant racial differences emerged in the prevalence of trauma or in PTSD diagnoses or severity. Only 30 veterans (4 percent) had a notation of PTSD in their chart, compared with the 84 veterans (12 percent) identified as having PTSD on the CAPS. Despite this discrepancy, no significant age-adjusted or unadjusted racial differences were observed in the likelihood of veterans having a PTSD notation in their chart. No significant racial differences emerged in the presence of additional psychiatric diagnoses or in service use and benefits. Service use is shown in
Table 1.
Discussion
Our analyses yielded only a few meaningful racial differences in trauma exposure, PTSD severity, psychiatric comorbidity, functional status, and service use and benefits. In the PTSD sample, the only significant racial difference to emerge was a higher rate of combat exposure among African-American veterans. All other significant racial differences emerged in the larger primary care sample. Specifically, Caucasians were significantly more likely to have a history of childhood sexual abuse; they also had a greater number of traumas. Furthermore, African-American veterans were more likely than their Caucasian counterparts to receive a substance-related diagnosis and to use VA substance use and urgent care services. Significant racial differences in dysthymia diagnoses disappeared after adjustment for age.
Differences in substance abuse or dependence diagnoses and service use are notable and warrant more attention. Concerns about overdiagnosis among African-American veterans in this study are minimized by the fact that rates of diagnoses and service use mirrored one another yet were derived from separate sources. However, base rates of substance abuse or dependence were low for all veterans compared with other psychiatric diagnoses, and future studies will be needed before any definitive conclusions can be made.
The finding that African Americans had more urgent care visits than Caucasians may reflect differences in perceptions about what difficulties warrant emergency care or differences in the timing of seeking needed services. It may be that African Americans wait until immediate care is needed before seeking services. However, generally speaking, African-American and Caucasian veterans appear to be using a majority of VA services at a similar rate. These data differ from the larger body of non-VA literature that suggests racial disparities in service use (
10). It is possible that qualities unique to the VA health care system, such as access to free care, or unique to veteran populations, such as homogeneity of veteran status, help minimize discrepancies in access to care.
This study had the limitations associated with any cross-sectional survey research. Largely, the causal impact between principal variables of interest cannot be determined. Second, with the exception of primary care visits, our service use variables were restricted to "yes" or "no" outcomes over 12 months. Examining service use over a longer period, as well as examining variables related to the content or process of these visits, may have yielded a more accurate picture of service use patterns among veterans.
Conclusions
Overall, the results of this study suggest that African-American and Caucasian veterans who are treated in VA primary care clinics are more similar than different in their symptom manifestation and service use, two constructs that logically should be heavily associated with one another. The most prominent racial differences were in rates of substance-related diagnoses and service use as well as in use of urgent care, which may warrant further investigation to ensure that all veterans are receiving needed care.