Final Budget for Fiscal Year 2006 Changes Medicaid and Medicare Rules, Cuts Funds for Mental Health Programs
The 2006 budget reconciliation bill, which was signed into law in early February, includes changes across a broad array of domestic programs, with a particular focus on health care entitlement programs. Provisions in the bill are projected to reduce overall federal spending by just under $40 billion over the next five years, which includes $11 billion in Medicaid expenditures. Of most concern to mental health advocates are changes to Medicaid rules that will allow states to impose premiums and higher cost-sharing on beneficiaries, which would drive many with the lowest incomes from the Medicaid program.
Congressional negotiators who worked behind closed doors to reconcile the House- and Senate-passed versions of the budget elected to cater to special interests, such as managed care and pharmaceutical companies, according to a report by the Center on Budget and Policy Priorities (CBPP) that analyzed data from the nonpartisan Congressional Budget Office (CBO). Negotiators rejected Senate-passed provisions that would have significantly reduced Medicare and Medicaid expenditures while avoiding harm to large numbers of beneficiaries with low incomes. These provisions would have saved nearly $12 billion over five years and more than $36 billion over ten years by curtailing excessive payments to Medicare managed care plans. Instead, the final budget will save $6.5 billion in Medicare managed care payments over five years and $4.1 billion over ten years—$32 billion less in savings over ten years than in the Senate's proposal.
In addition, the Senate-passed provisions would have secured better prescription drug prices for Medicaid by increasing the rebates that drug manufacturers pay to the program, saving $4 billion over five years and $10.5 billion over ten years. However, the final budget contains only two minor rebate provisions that will lead to savings of about $220 million over five years and $720 million over ten years—$9.8 billion less in savings over ten years than in the Senate's proposed budget.
Provisions in the 2006 budget will allow states to substantially increase Medicaid copayments for services and medications. Until the rule changes were made, copayments could not exceed $3 for each service or medication, with some populations—including children—fully exempt from copayments. The new rules will extend copayments to nearly six million children, according to CBO estimates. For beneficiaries with incomes between 100 and 150 percent of the poverty line (between $16,000 and $24,000 for a family of three), states could charge copayments of up to 10 percent of the cost of the needed service or medication. Individuals above 150 percent of the poverty line could be charged as much as 20 percent.
For the first time, providers (including pharmacies) will be able to deny services to beneficiaries who cannot afford copayments. Previously, Medicaid beneficiaries who could not pay remained financially responsible to the provider but were not denied services or medications.
A new provision specifically allows higher cost-sharing for medications that are not on a state's preferred drug list (PDL). Advocacy groups are concerned that medications to treat severe mental illness will be vulnerable to being designated as nonpreferred. In recent years some states have moved to limit antipsychotic and antidepressant medications on PDLs, and more limitations are expected in the wake of this provision.
Eighty percent of the savings that result from copayment increases will come from decreased use of services rather than from collection of higher copayments, according to CBO estimates. The estimate is in line with research showing that even small increases (less than 5 percent) lead many low-income beneficiaries to forgo needed services and medications.
Another cost-sharing feature in the new Medicaid structure will be the imposition of premiums for coverage for some groups for the first time in the program's history. The CBO estimates that 65,000 individuals will lose Medicaid coverage over the next ten years because they will not be able to afford premiums. Children will account for 60 percent of this group.
Savings will also be realized by allowing states to substitute substantially scaled-back Medicaid benefit packages for various groups of beneficiaries, including working-poor parents. The alternative packages exclude some services that states were previously required to provide. During final budget negotiations, provisions that would have retained benefit protections for children below the poverty line were rejected.
The CBO estimates that a vast majority of children enrolled in Medicaid, including those below the poverty line, could effectively lose access to the comprehensive health care coverage that they now are guaranteed through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) component of Medicaid. States will be permitted to provide scaled-back benefits to children, as long as states "wrap around" the packages so that overall coverage remains available for the same health care services that previously were required to be available under EPSDT. This approach is unlikely to work well in practice, according to the CBO. Evaluations of wraparound coverage for children in Medicaid managed care plans show that it can be ineffective and that children often go without some care.
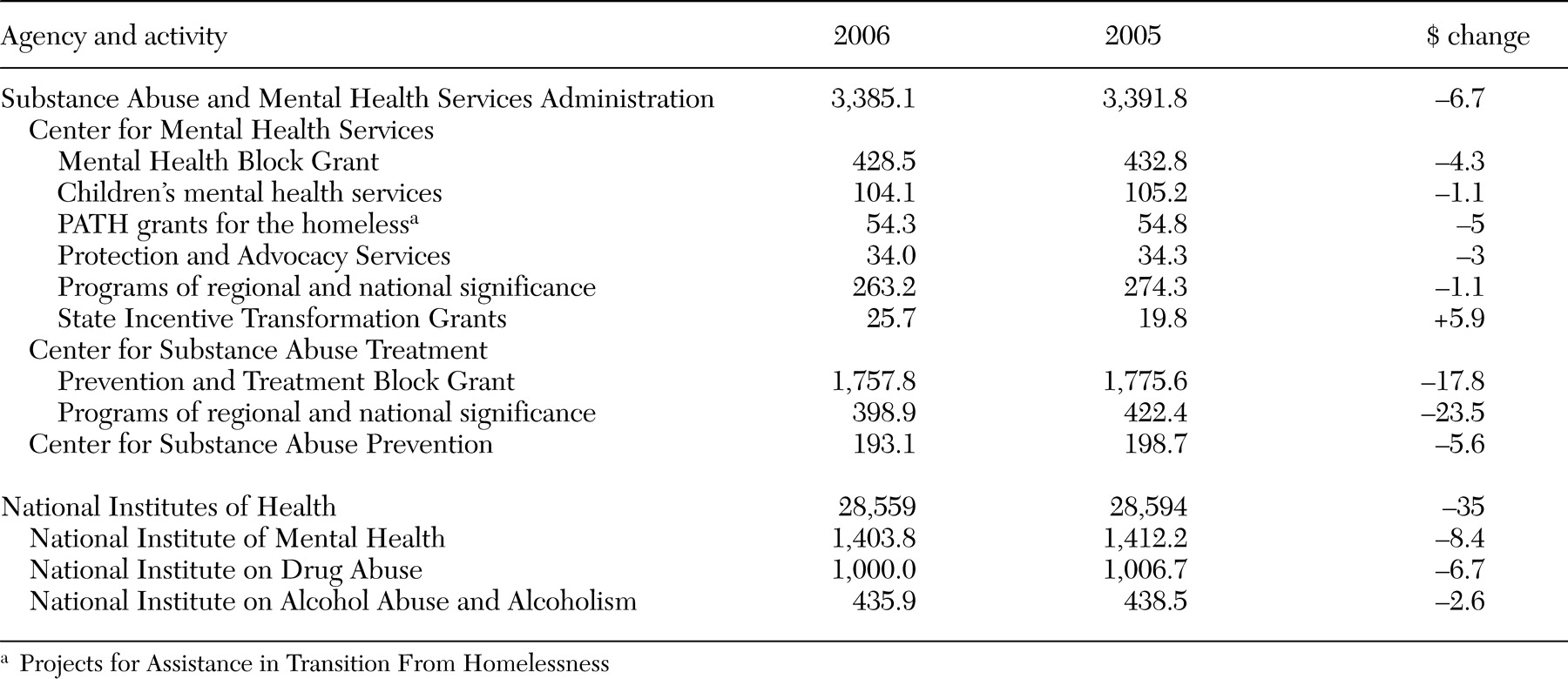
Appropriations for the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institutes of Health (NIH) were also finalized. As shown in
Table 1, overall funding was cut for both institutions; the cuts include an across-the-board reduction of 1 percent that was imposed during the final budget negotiations. The reduction in NIH funding was the first in three decades. The National Institute of Mental Health Mental (NIMH) will see its first cuts in funding in more than 20 years. The Senate-passed provisions that were not included in the final budget specified a $48.2 million increase for NIMH. At SAMHSA funds were cut for all programs except the State Incentive Transformation Grant program, which will allow states that successfully competed for transformation planning grants to obtain a continuation of funding in 2006 to implement plans.
The CBPP reports can be found on the center's Web site at www.cbpp.org. NIH has established policies for research grants that reflect the 1 percent cut (http://grants.nih.gov/grants/guide/notice-files/NOT-OD-06-025.html).
News Briefs
Kaiser forum on Medicare part D: In late January, six representatives of groups involved with the implementation of Medicare part D met at a forum sponsored by the Kaiser Family Foundation. The 62-page forum transcript provides a "report from the trenches" on the program's first month. An executive from Walgreen's describes what transpired for consumers at pharmacy counters and staff members' efforts to determine eligibility, copayments, and covered drugs. An administrator from the Center for Medicare and Medicaid Services discusses problems with automatic enrollment and timely provision of identity cards. The CEO of a large health insurance plan describes reimbursement strategies for enrollees who paid large deductibles and other costs to obtain medications immediately. A former state Medicaid director and two consumer advocates also contribute to this unique "debriefing." The forum is also available as a Webcast and a Podcast at www.kaisernetwork.org.
DBSA report on depression in America: A report released by the Depression and Bipolar Support Alliance (DBSA), The State of Depression in America, describes the impact of a disorder that drains more than $83 billion annually from the economy, affects 19 million people, and results in thousands of preventable suicides. The 10-page report, which is based on a literature review and interviews with stakeholders, was developed to inform legislators, policy makers, and other critical stakeholders. The report concludes that because the mental health system is "crisis-oriented and reactionary," it does not focus on prevention, proactive treatment, and long-term wellness." The report makes recommendations for "the five first steps" to address the problems. Congress must provide parity in Medicare coverage for patients who receive mental health services. Private insurers must provide greater incentives for primary care physicians to identify and treat depression. Loan forgiveness programs should be enacted to provide incentives for students to specialize in mental health care. Biologic and genetic research must be expedited to develop better treatments. The government and private sector must support and promote increased access to peer support services. The report is available on the DBDSA Web site at www.dbsalliance.org.