Schizophrenia spectrum disorders are a heterogeneous group defined by positive (e.g., delusions or hallucinations) and negative symptoms (e.g., affective flattening, avolition, and/or apathy) as well as significant deficits in psychosocial functioning. Recently, depressive symptoms have been increasingly recognized as a common experience for those with schizophrenia spectrum disorders (
1,
2). Antipsychotic pharmacotherapy, which is often the first-line treatment for such patients, can be beneficial, although reductions in symptoms tend to be small to moderate, greatest for positive symptoms, and absent for some patients (
3). Additionally, even with adequate symptom management, people with schizophrenia spectrum disorders often continue to experience functional challenges. Despite these challenges, it is understood in the field that people with these disorders are able to work toward recovery (
4–
6). As such, a resurgence of interest in adjunctive treatments and facilitators for recovery has occurred in recent decades, including group-based interventions, family psychoeducation, skills training, and psychotherapy (
7).
Our understanding of recovery, coupled with a vast research literature, indicates that psychotherapy can be effective for individuals with schizophrenia spectrum disorders and should be made available to them (
8). However, a gap in treatment options remains for people in this group who experience depressive symptoms. In this vein, our aim is to introduce interpersonal and social rhythm therapy (IPSRT), a psychosocial treatment originally developed to target the affective symptoms and psychosocial impairment associated with bipolar disorder (
9), as one potential psychotherapy option for people with schizophrenia spectrum disorders who experience depressive symptomatology. We propose that IPSRT has potential to provide symptom and functional benefits to these patients and may be, in fact, uniquely suited as a model to work well for these individuals. Indeed, IPSRT was developed for treatment of bipolar disorder, but there is significant evidence of overlap between bipolar and schizophrenia spectrum disorders in etiological processes, candidate endophenotypes, and clinical presentation (
10,
11). Of note, those who initially receive diagnoses of bipolar disorders are at heightened risk for a later diagnosis of schizoaffective disorder or schizophrenia (
12). Additionally, recent work (
13) has extended the evidence suggesting that physiological alterations are similar across these disorders, although these alterations may be on a continuum of severity, with those manifesting in schizophrenia appearing most severe.
Taken together, past research indicates that people with schizophrenia spectrum disorders benefit from psychotherapy (
14) and experience prevalent mood symptoms (
1,
2). Furthermore, extensive clinical and pathophysiological overlap between schizophrenia spectrum and bipolar disorders suggests that psychosocial treatments may provide benefits across disorders for these patients. This article will provide a brief overview of IPSRT, highlight some research suggesting the potential utility of IPSRT for people with schizophrenia spectrum disorders and depressive symptoms, and present a case example of IPSRT with a man diagnosed as having schizophrenia.
Overview of IPSRT
Like schizophrenia spectrum disorders, bipolar disorders were once viewed as best treated with pharmacotherapy, and, against the backdrop of disappointingly low remission and recovery rates, the need for novel adjunctive modalities was clear (
15). IPSRT was originally developed by Frank and colleagues (
16) as an adaptation of interpersonal psychotherapy (IPT) (
17) for bipolar I disorder (
18) and has since been adapted for bipolar II disorder (
19) and adolescents with bipolar spectrum disorders (
20). IPSRT rests on an instability model that defines three interconnected pathways to affective recurrences: social rhythm disruption, stressful life events, and medication nonadherence (
16,
18). At its core, IPSRT is a hybrid treatment that combines the elements of IPT for unipolar depression with a behavioral intervention (social rhythm therapy) to target disrupted social rhythms. Social rhythms are activities, such as the time one gets out of bed or has contact with another person, that are thought to exert some effect on underlying biological rhythms and serve as social anchors (
18). They are environmental “zeitgebers” (time givers). In IPSRT, the clinician helps the patient improve and stabilize their mood by resolving interpersonal problems and regulating social rhythms (
9,
16).
According to Frank and colleagues’ work (
9,
16,
18,
21), changes in social rhythms may be caused by temporary circumstances, such as travel to a different time zone or a conflict with an important source of social support, or may be altered in more sustained ways, such as through shift work or the death of a loved one. These changes in daily rhythms lead to changes in biological rhythms and the subsequent development of physiological symptoms. This chain of events ends with a mood episode. One’s progression through this cycle depends on additional psychosocial factors as well as the inherent flexibility of one’s internal biological rhythms (i.e., one’s clock). People with bipolar disorder are believed to be vulnerable to progression through this cycle because of relative inflexibility in their biological clocks (i.e., reduced ability to sustain change in rhythms without physiological consequences) coupled with psychosocial factors that may be compromised, such as social support and/or coping skills. Individuals without these vulnerabilities may experience some adverse effects but are not expected to progress to the stage of a mood episode (
9,
16,
18,
21).
IPSRT is a manualized treatment (
9) that has initial, intermediate, and maintenance or continuation phases. In IPSRT, the clinician helps the patient link mood and life events, identify and manage symptoms, mourn the loss of the healthy self, resolve a primary problem area, maintain regular daily rhythms, and predict and troubleshoot potential precipitants of rhythm dysregulation.
Table 1 provides a description of IPSRT therapeutic tasks by treatment phase. During the initial sessions, the IPSRT clinician provides psychoeducation and introduces the Social Rhythm Metric (SRM) (
21), a tool to help gather data about patients’ existing rhythms, set targets for social anchors, and then track and maintain rhythms over time. Intermediate sessions continue to track and support stability of social rhythms and work to address the interpersonal problem area. The original IPT protocol defines four potential interpersonal problem areas: role transitions, role disputes, interpersonal deficits and/or sensitivities, and grief (
22). IPSRT adds an additional interpersonal problem area: grief for loss of the healthy self. This interpersonal problem area allows the patient an opportunity to process the perception of having lost the person they might have been without the disorder and the transition they may experience in being diagnosed as having a serious mental illness (
9). IPSRT ends with the continuation or maintenance phase, which is structured around continued stability of social rhythms, even when the patient is faced with significant life events or other stressors. Patients in the maintenance phase reduce session frequency from weekly to every 2 weeks and, eventually, to monthly. Sessions may then continue at a reduced rate, or patients may conclude therapy.
There is a high level of support for IPSRT as an acute and maintenance treatment for mood symptoms. Results from randomized controlled trials have demonstrated that IPSRT can extend the time between episodes for those with bipolar I disorder (
16), reduce time to recovery from a depressive episode (
23), and reduce time to recovery of functional capacities after a mood episode (
24). In bipolar II, IPSRT has been shown to improve symptoms among both medicated and unmedicated patients (
25,
26).
IPSRT for Schizophrenia Spectrum Disorders and Depressive Symptoms
Some research in the field suggests that the IPSRT model may be applicable for those with schizophrenia spectrum disorders who experience mood symptoms. Indeed, some clinical applications of IPSRT have already been suggested (
27) or undertaken in settings focused on affective psychosis, specifically for those early in the course of their illness. Early results (
28) have suggested the intervention is feasible and may reduce mood symptoms and improve functioning for such individuals.
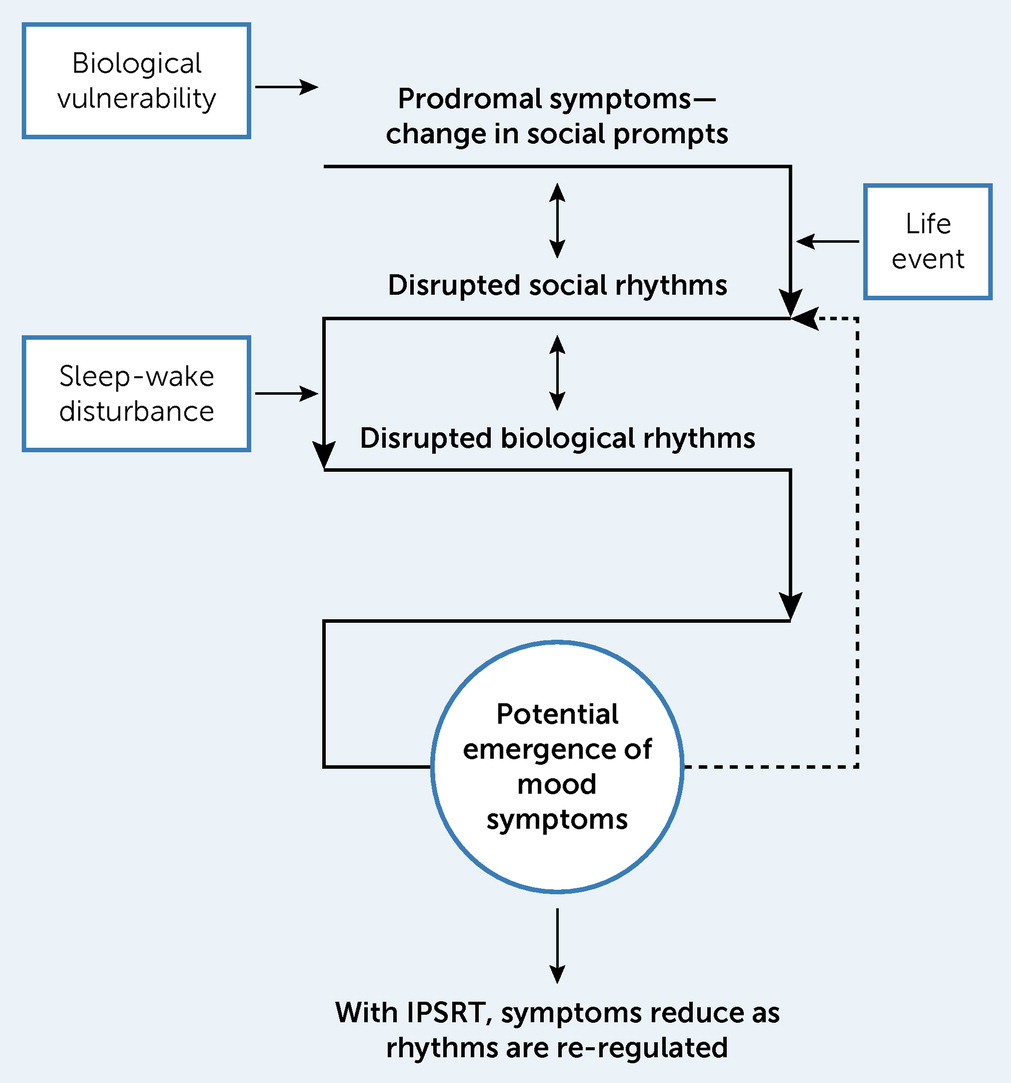
Figure 1 shows one potential way in which the IPSRT model may be applied for therapeutic work with people with schizophrenia spectrum disorders who experience mood symptoms. Below, we highlight some findings from the literature supporting the potential theoretical utility of the IPSRT model for people in this group.
Depressive Symptomatology in Schizophrenia Spectrum Disorders
Although depressive symptomatology is not part of the diagnostic criteria for schizophrenia spectrum disorders, with the exception of schizoaffective disorder, studies (
1,
2) suggest an extremely high rate of these symptoms among people diagnosed across the spectrum of psychotic disorders (up to 80% prevalence of clinically significant lifetime depressive symptoms, with particular risk for depression during the early phase of the disorder, soon after diagnosis). Depressive symptoms in this group are associated with poor long-term outcomes, including substance-related problems, reduced life satisfaction and quality of life, and reduced psychosocial functioning (
29). Depressive symptoms are also associated with lower medication adherence and greater need for psychiatric intervention (
29). Depression and hopelessness also strongly predict suicidal ideation, suicide attempt, and suicide among people with these diagnoses (
30). Despite high prevalence and associated negative outcomes, depressive symptomatology is often not adequately treated for those with schizophrenia spectrum disorders, and few psychotherapeutic trials have included depression as a primary treatment target.
Circadian and Sleep Disruption
People with schizophrenia spectrum disorders frequently experience sleep disturbance (
31), similar to that seen among those with bipolar disorder (
32) and indicative of disrupted daily rhythms. Indeed, in addition to their role in relation to mood symptoms, sleep abnormalities may have a key role in triggering heightened dopaminergic activity, which increases risk for a psychotic episode. Psychotic symptoms then can aggravate sleep and potentially maintain a maladaptive physiological cycle of sleep irregularities, heightened dopaminergic activity, and increased mood and psychotic symptoms (
33). Although sleep disturbance is highly prevalent among individuals with schizophrenia spectrum disorders, it often goes unaddressed during treatment, and, problematically, antipsychotic medications may play some role in contributing to reduced stability of circadian rhythms (
34–
36).
Social Deficits
People with schizophrenia spectrum disorders experience significant social impairment that can be considered core to the illness (
37,
38), including reduced social skills and difficulty maintaining typical social roles (
39). Social deficits in schizophrenia spectrum disorders are thought to be mediated by impairments in social cognitive abilities (
37), including deficits in theory of mind, social perception, social knowledge, emotion perception, emotion processing, and empathy (
40,
41). Research indicates that people with schizophrenia spectrum disorders tend to be socially isolated (
42), which has a negative impact on symptoms and functional outcomes (
43,
44). Notably, people with these disorders also report a desire for more or better social relationships and endorse loneliness in the context of social isolation (
45), suggesting that an interpersonally oriented intervention may be particularly useful. Furthermore, depressive symptoms and measures of social relationships or cognition have been found to be correlated in studies of schizophrenia spectrum disorders (
29,
46), suggesting that social outcomes may be linked in part to depressive symptomatology.
In summary, the research reviewed here suggests that the IPSRT model may have utility in organizing thought about schizophrenia spectrum disorders. Patients with these disorders show evidence of prominent mood symptomatology, experience circadian and sleep disruption, and show interpersonal dysfunction as a core facet of psychopathology. As such, the IPSRT model may benefit patients with schizophrenia spectrum disorders with depressive symptoms who participate in psychotherapy. We expect that IPSRT may provide primary symptomatic improvement for depression, and it may also have indirect positive effects on psychotic symptoms through interventions targeting social rhythms, sleep, and interpersonal engagement. In addition, IPSRT may benefit people with schizophrenia spectrum disorders in other areas, summarized below.
Grief Related to Diagnosis
A highly relevant interpersonal problem area for people with schizophrenia spectrum disorders is grief for the loss of the healthy self (
9), especially for those with early psychosis. Much qualitative work has explored the unique experience of adjusting to life after an episode of psychosis and subsequent diagnosis. Patients report feeling as though having a schizophrenia spectrum disorder makes it difficult to lead a normal life, and dreams for the future may no longer feel realistic or attainable (
47). People with early psychosis have reported feelings of estrangement from the self and a need to reconstruct the self in light of changes in identity resulting from psychosis and a diagnosis of schizophrenia spectrum disorder (
48). Furthermore, people with early psychosis report feelings of loss and isolation, often leading to depressive symptomatology (
49). These patients have cited the value of supportive social relationships in promoting recovery (
48,
50,
51). These findings emphasize the importance of interventions for this group that target maintenance of interpersonal connection and allow for patients to process their sense of loss and make meaning of their experiences.
Functional Deficits
People with schizophrenia spectrum disorders experience functional deficits in many areas, including social relationships, employment, ability to attend school, self-care, and health behaviors (
52,
53). Schizophrenia spectrum diagnoses are also associated with increased risk of homelessness (
54). As such, the structured approach of IPSRT (through use of the SRM) may provide some immediate benefit to people with these disorders in functional domains that may be tied to routine. For example, people who are maintaining a schedule may be more able to obtain and maintain employment. Self-care may also be tied to a routine, with hygiene and health behaviors linked to specific times or anchors throughout the day.
Medication Adherence
People with schizophrenia spectrum disorders are often prescribed antipsychotic medications. Medication regimens can be complex, and medications may not be taken as prescribed (i.e., nonadherence). Rates of nonadherence are relatively high, estimated as ranging from 20% to 60% (
55). Nonadherence to antipsychotic medications among those who need them may lead to exacerbation or return of psychotic symptoms and decreased likelihood of return to prior levels of functioning, whereas adherence among those with early psychosis is related to improved long-term course of illness (
56). Establishment of social anchors may provide environmental support to assist in management of complex medication regimens, thereby promoting medication adherence. Furthermore, psychoeducation regarding the importance of medications is regularly incorporated into therapy sessions.
Case Vignette
Considering the evidence for IPSRT as one potentially therapeutic option for people with schizophrenia spectrum disorders and depressive symptoms, we chose to offer IPSRT to a patient with a schizophrenia spectrum disorder who was seeking therapy. Details about the case and outcome are provided below, with identifying information altered to protect confidentiality. The patient provided consent to the authors to include a deidentified description of his case in written works.
David was a 58-year-old, single White man diagnosed as having schizophrenia who was referred for psychotherapy after the death of his mother, 1 month prior to the initiation of IPSRT. At the time of treatment, David had been experiencing symptoms of schizophrenia for nearly 40 years. He had engaged consistently in medication and group therapy treatments for the past 5 years and had completed a full course of cognitive-behavioral therapy for psychosis, resulting in increased ability to understand and cope with psychotic symptoms. David reported good adherence to psychotropic medications, including antipsychotic and antidepressant medications.
David’s chief complaint at the start of therapy was that “everything [had] changed” since his mother died. David’s relationship with his mother had been mixed. He felt she could be unkind to him, but for several years prior to her death, David had played a big role in her care. He routinely visited her, took her out for meals, took her and her friends on outings, and drove her to appointments. David had effectively structured his life around his mother’s schedule. For the month prior to her death, David’s mother was moved into a hospital, then back home, then to hospice care, all with David as her primary caregiver. This period was particularly chaotic for David. He chose to discontinue his psychotropic medications in the week prior to his mother’s death so that he could be more alert during the evenings to assist in her care, which led to increased psychotic symptoms, primarily in the form of auditory hallucinations.
At the time of the initial evaluation, David had resumed his medication, and his psychotic symptoms had returned to baseline. David reported clinically significant depressive symptoms at the start of treatment. He also endorsed auditory hallucinations, infrequent command hallucinations, and paranoid delusions in social contexts. Regarding negative symptoms, David expressed difficulty with motivation and initiation of tasks, reduced interest in recreational activities, and physical anergia that was evidenced by increased time in bed and reduced activity at home. David also displayed cognitive symptoms, primarily in his attentional and working memory abilities. At the time of the initial evaluation, David completed the Patient Health Questionnaire–9 (PHQ-9) with a score of 17, representing moderately severe depression. He was rated on the Clinical Global Impressions (CGI)–Severity scale by the therapist as “markedly ill.”
In session 1 of IPSRT, David completed the interpersonal inventory with the therapist, revealing that he had many social connections with relatives, although he reported feeling close to no one. David gave some context regarding his relationship with his mother and the changes in his life since her passing; the therapist encouraged David to discuss his relationship with his mother and to express his thoughts and emotions regarding her death throughout the course of therapy. The therapist also provided psychoeducation regarding the model and structure of IPSRT and the link between symptoms of depression and social relationships. During session 2 of IPSRT, David showed increased emotion related to his mother’s death, which he linked to the upcoming Mother’s Day holiday. He was tearful in session, and the therapist encouraged him to express and sit with the affect and provided psychoeducation regarding the process of grief.
In session 3, David provided his illness timeline to the therapist. This revealed that David had previously experienced two major depressive episodes, both with psychotic symptoms and resulting in his only two psychiatric hospitalizations. Both episodes had been immediately preceded by significant life events and subsequent disruption of daily rhythms: one when David left the military and another when David left regular employment. The therapist highlighted these instances in the context of the IPSRT model. David was surprised by this connection and agreed that the pattern was clear. The timeline and IPSRT model were both reviewed during session 4, and the therapist provided psychoeducation regarding how David’s mother’s death had also disrupted his rhythms. This review reinforced the need for preventive psychotherapy and set up the introduction of the SRM.
In session 5, the therapist introduced the SRM and invited David to begin tracking his rhythms. David was instructed not to change any of his rhythms—only to track them over the next week. David brought his completed SRM to session 6, which revealed areas of inconsistency in his rhythms. Additional SRM data were collected between sessions 6 and 7, prior to setting targets for SRM items (e.g., out of bed at 9 a.m.). David worked with the therapist to determine regular activities that could serve as new social anchors for him, now that he no longer had regular activities with his mother, in order to flesh out his daily routine.
Throughout the intermediate sessions, David was encouraged to discuss his relationship with his mother—both the positive and negative aspects—and the ways his life had changed as a result of her death. The therapist also encouraged continued activity outside his home, the addition and maintenance of regular social anchors, and consistency through tracking with the SRM. David did well with the tracking and vastly increased his daily activities outside the home. By the time David entered the maintenance phase of treatment, he was consistently leaving his home at least 6 of every 7 days. He had also increased engagement with his family members and his neighbors, and he had reached out to reconnect with an old friend whom he had met several years prior but had not seen in some time. David was also better able by this time to reflect on his mother’s death and what she had meant to him in life. He had a balanced view of their relationship and felt he had been able to mourn the loss of his mother and reengage with other parts of his life.
By the time he entered the maintenance phase, David’s score on the PHQ-9 was reduced to 11, suggesting moderate depression, which had been sustained over several sessions. David reporting feeling as though his mood had improved as a result of therapy. His score on the CGI as rated by the therapist had dropped from “markedly ill” to “moderately ill.” David also endorsed less distress related to his hallucinatory and delusional symptoms.
Analysis and Modifications of IPSRT for Schizophrenia Spectrum Disorders
David’s case provides positive evidence for potential benefit of IPSRT in a number of areas. First and most important, David experienced reduction in depressive symptoms over the course of treatment and became much more active and engaged outside his home. Several elements of IPSRT were also particularly useful in David’s treatment. For example, David’s understanding of his illness timeline was meaningful to him and supported the rationale for IPSRT as a preventive exercise. This understanding promoted David’s engagement early in therapy, which was maintained throughout the treatment protocol. Encouragement of affect in discussion of David’s mother’s death was also particularly impactful. People with schizophrenia spectrum disorders who have negative symptoms may appear to express fewer emotions than someone without a diagnosis and to have reduced intensity and duration of emotional expression (
57). As a result, others may assume that they experience less emotion, although research shows that people with these disorders report experiencing emotions at similar intensity to psychiatrically healthy comparison subjects, even when not expressed (
57). In David’s case, although he did not readily express it, he was experiencing a mixture of complex emotions in the wake of his mother’s death. Allowing space in therapy for him to express and sit with these emotions was a powerful intervention for him.
Although this example was generally successful in the implementation of IPSRT and David experienced improvements in depressive symptoms and psychosocial functioning, there were also challenges. David had continuous delusions that were related to social relationships, which complicated the process of establishing social anchors. Because David’s psychosis was relatively well managed, the therapist was able to avoid having psychotic symptoms as the focus of the IPSRT sessions, which may be more difficult in the treatment of patients with more severe or pervasive symptomatology. Another challenge related to the SRM: although David excelled at tracking his social rhythms and daily mood, he declined to rate interpersonal contact. In processing this decision with the therapist, David reported that he felt adding another element to the SRM would make it too complicated. He also found the interpersonal contact rating system to be difficult to understand. Part of David’s experience with the SRM may have been related to the cognitive symptoms of schizophrenia that he exhibited. However, it is also likely that some IPSRT materials may be overly complex for usage with people with schizophrenia spectrum disorders.
In light of case evidence and in the context of research on schizophrenia spectrum disorders generally, some modifications to IPSRT may be appropriate for future research in this group. A primary modification relates to the course of treatment. In IPSRT for bipolar disorder, 20–24 weekly sessions are recommended (
9), followed by maintenance sessions, sometimes long term. For individuals with schizophrenia spectrum disorders, the course of weekly treatment may need to be longer, especially with respect to the initial phase. Additional time should be dedicated to ensuring patients’ understanding of the SRM and the rationale for its use. The SRM and other therapy materials may also be edited to reduce the complexity and reading level to be appropriate for use in this population. Furthermore, presentation of information related to depression as a common experience for those with schizophrenia spectrum disorders would be helpful in the initial phase of therapy to promote an integrated model of treatment. Finally, IPSRT generally may not be appropriate for patients with schizophrenia spectrum disorders who are acutely symptomatic because IPSRT is not directly oriented toward immediate management of psychotic symptoms.
Conclusions
For many people with a schizophrenia spectrum disorder and depressive symptoms, pharmacotherapy will be insufficient for adequate symptom management and functional recovery. Thus, there is a need for adjunctive modalities that target not only the psychotic symptoms of these disorders but also comorbid depression. Because of the similarities across schizophrenia spectrum and bipolar disorders, IPSRT is one potential psychotherapy option to consider for people with schizophrenia spectrum disorders (
Box 1). Future work should build on the case example presented here to design and implement a randomized controlled trial of IPSRT for schizophrenia spectrum disorders and depressive symptoms and to evaluate the need for modifications to this therapy.