Childhood posttraumatic stress disorder (PTSD) and its related suicidality are major public health problems causing severe health consequences to the child and financial burden to society, with an estimated cost of $103 billion annually (
1,
2). Suicide is the second-leading cause of death among youths ages 10–19 years, especially among those with PTSD (
3,
4). Youth visits to psychiatric emergency rooms (PERs) for suicidality are rising across the United States, especially among those with traumatic stress exposure and self-harm behavior (
5–
12).
The focus of positive psychiatry is to reverse the imbalance created by conceiving of mental health through the deficit model as an additive to traditional psychiatry (
13,
14). Positive psychiatry is defined by interventions designed to foster well-being by promoting positive emotions, thoughts, and behaviors under voluntary control (
12,
15,
16). Reminder-focused positive psychiatry (RFPP) is an acceptable and feasible evidence-based group treatment for youths with PTSD and their families that focuses on trauma reminders. RFPP is associated with improved core PTSD symptoms, decreased severity of RTLR, increased vascular function, reduced inflammation, and favorable long-term clinical outcomes (
17).
This study investigated the effect of the brief RFPP and suicide prevention intervention (RFPP-S) on core PTSD symptoms, the severity of RTLR, suicidality, mental well-being, parent-child interactions, and clinical outcomes of youths with PTSD who received treatment at the Olive View–University of California, Los Angeles (UCLA) PER (OV-PER).
Methods
Using a nested, matched case-control design, this retrospective cohort study included 50 youths with PTSD and suicidality receiving RFPP-S and 150 youths with PTSD and suicidality receiving treatment as usual (without RFPP-S; control group) during their OV-PER visit. All youths were admitted to the PER because of danger to self; all showed symptoms of suicidal ideation, defined as a score of ≥3 on the Columbia Suicide Severity Rating Scale (C-SSRS); and 19% (N=38) exhibited suicidal behavior. PER clinicians administered the C-SSRS, the Patient Health Questionnaire–9 (PHQ-9), and PTSD screenings. PTSD diagnoses were based on ICD-10-CM and DSM-5 codes.
All participants received Medi-Cal insurance coverage and were screened, neuropsychiatrically assessed, and followed by one provider. Participants were youths (ages 9–18) with comorbid PTSD and suicidality (i.e., C-SSRS score ≥3) who were admitted to the OV-PER on a Monday or Wednesday, who did not have other major psychiatric disorders or prior suicide attempts, and who received developmental age–appropriate, clinically indicated RFPP-S. Eligible youths with comorbid PTSD and suicidality who did not receive RFPP-S were matched with participants from the RFPP-S group in terms of age, gender, and enrollment time. These youths received treatment as usual at the OV-PER and were randomly selected to form the control group. Demographic and clinical characteristics and long-term clinical outcomes of participants were obtained by using Los Angeles County Department of Health Services (DHS; Online Realtime Centralized Health Information Database) and mental health clinic (myAvatar) electronic medical records, DHS administrative records (I2B2 data portal), and chart review. All participants were followed for a mean of 6 months between 2018 and 2020. This study was approved and overseen by the institutional review board committee of the Olive View–UCLA Education and Research Institute in Sylmar, California.
Control Group
Using a nested, case-control design, participants matched for age, gender, and enrollment time were randomly selected from a pool of 315 eligible youths with PTSD and suicidality who did not receive RFPP-S. These youths were admitted to a PER on a Tuesday or Thursday, received treatment as usual at the OV-PER, and were screened, neuropsychiatrically assessed, and followed by one provider as part of a large, ongoing clinical initiative of adapting trauma-informed screening tools (i.e., strength-based characteristics; traumatic stress symptoms; mood and suicide symptoms) and interventions at PERs, which started in 2018.
RFPP-S
In this study, RFPP, which has high fidelity and acceptability, focused on enhancing contextual discrimination and emotional regulation and on promoting adaptive coping strategies in response to trauma reminders, including by recognizing reminders and shifting attention during exposure to reminders from intrusive memories to positive feelings, thoughts, goals, and choices. (A table describing RFPP-S skills is available as an
online supplement to this article.) The treatment also included exercises to mitigate avoidance and reduce psychological and physiological reactivity associated with trauma reminders. RFPP-S, a developmental age–appropriate, trauma-informed safety prevention intervention, consists of two components of RFPP (i.e., trauma reminders and avoidance and negative cognitions) as well as safety planning and distress tolerance skill sets for youths with PTSD and their families. RFPP-S includes components for youths as well as for parents. All youths and parents in the RFPP-S group participated in the RFPP-S intervention.
Youth component.
The two components of RFPP-S are trauma reminders and avoidance and negative cognitions. The trauma reminders component consists of exercises in self-compassion; treatment engagement; tolerance of trauma reminders related to negative emotions; and ability to manage reactivity to trauma reminders and related suicidality by improving distress tolerance, including through self-talk and parental support to improve contextual differentiation between the current reminders and the original trauma. This component aims to enhance recognition of trauma reminders, promote enhanced adaptive coping strategies through treatment engagement and shifting attention, help patients tolerate distress and diminish their suffering while experiencing trauma reminders and related suicidality by experiencing feelings of caring and kindness toward themselves, promote behavioral interventions to bounce back from distress by enhancing emotion regulation and the ability to introspect, and help patients develop positive emotion by expressing gratitude to self and others and through social connectedness.
The avoidance and negative cognitions component consists of exercises to increase flexible thinking and express and label negative thoughts, emotions, and physical reactions. It also includes strategies to promote posttraumatic constructive progression and adherence to treatment; increase purposeful interactions with parents by improving positive attention toward self; increase positive feeling and enhance interpersonal relationships; and manage common problems, possible solutions, and safety skills.
Using the UCLA Trauma Reminder Inventory, we identified the two most prevalent traumatic reminders related to recent suicidal ideation. RFPP-S modules were practiced for 10 minutes twice daily for 2 consecutive days for youths with PTSD and suicidality.
Parent component.
Parents received one 10-minute psychoeducation session with RFPP-S modules. RFPP-S groups received two text messages or telephone calls each week after discharge reminding them of postdischarge mental health visits.
Treatment as Usual
As part of treatment as usual, youths were evaluated for suicidal ideation or behaviors at PERs and were protected from self-harm through placement in a supervised private room without access to potentially dangerous objects (e.g., belts, shoelaces, sharp medical instruments). They were engaged in a respectful, collaborative milieu and in conversations with the mental health team to keep them calm and received suicide risk assessment, screening to determine the level of care, and interventions to help them develop skills to recognize and cope with suicidal thoughts and PTSD, including action plans for making their environment safer and for identifying sources of help. Psychiatric hospitalization was the typical disposition for individuals in acute crisis with PTSD and with moderate-to-high suicide risk. Standard treatment as usual included a follow-up session for primary outpatient mental health care within 2 weeks of PER discharge.
Psychiatric Measurements
As part of clinical practice, the C-SSRS, Clinician-Administered PTSD Scale for children and adolescents (CAPS-CA), UCLA Trauma Reminder Inventory, PHQ-9, Parent-Child Interaction Questionnaire–Revised (PACHIQ-R), Positive Emotion, Engagement, Relationships, Meaning, and Accomplishment (PERMA) Scale, and positive psychiatry batteries were assessed at baseline, day 2, and 1 month after discharge in both the RFPP-S and the matched control group. For the RFPP-S group, the above measures were assessed 1 week after discharge, and the C-SSRS and CAPS-CA were assessed at 6 months after discharge. For the 6-month follow-up, the Los Angeles County Department of Mental Health used the clinician-rated C-SSRS and CAPS-CA for both groups.
Outcome Measures
The primary aim of this study was to assess change in PTSD score and suicidality among youths with PTSD and suicidality after receiving RFPP-S, compared with baseline scores. The secondary aims were to examine the effectiveness of RFPP-S, compared with treatment as usual, in improving core PTSD symptoms, suicidality, well-being, and clinical outcomes (i.e., mental health follow-up 1 week after discharge, psychiatric rehospitalization at 1 month, suicidality at 6 months, and severity of PTSD symptoms and psychiatric rehospitalization at 6 months).
Statistical Analysis
Means with standard deviations and proportions were used to summarize the study group’s characteristics. Continuous variables were compared by using analysis of variance (ANOVA), and Cochran-Mantel-Haenszel statistics were used to compare categorical variables. Mixed-regression analyses were used to assess change in PTSD symptoms and psychiatric measures in the RFPP-S group compared with the control group. Using multivariate mixed-regression analyses, we assessed risk factor–adjusted PTSD symptoms, PHQ-9 scores, and positive biopsychosocial traits in both groups, and confidence intervals were calculated by using a bootstrapping technique, with a bias of less than 2.5%. All statistical analyses were performed with SAS, version 9.2, and SPSS, version 24. The level of significance was set at p<0.05 (two-tailed). Although records of assessments, interventions, and follow-ups at OV-PER were readily available and included in this study, data on psychiatric hospitalization after participants were transferred to the youth inpatient psychiatric unit were not available. About 40% of data on second-day assessment, discharge, and follow-up were missing in the matched control group. Missing data were imputed by using statistical approaches. Cross-validation bootstrapping analysis was performed with and without missing data imputations, revealing less than 2.5% bias in measurements.
Results
Demographic and clinical characteristics are presented in
Table 1. At baseline, there were no significant differences between the RFPP-S and control groups in terms of age, gender, PTSD symptoms (CAPS-CA score >38, with moderate-to-severe symptoms in both groups), suicidality (C-SSRS score ≥3, with moderate-to-severe suicidal ideation), PHQ-9 score, selective serotonin reuptake inhibitor (SSRI) treatment, positive biopsychosocial traits, or emergency and psychiatric hospitalization.
On OV-PER day 2, more robust reductions of baseline PTSD symptoms (55%) and RTLR (80%) were observed in the RFPP-S group, compared with the control group (10% for both) (p=0.001). Similarly, a significantly larger reduction in baseline C-SSRS score (1 or 2, with no or mild suicidal wishes and no intent) was noted in the RFPP-S group (80%), compared with the control group (15%) (p=0.001). More rapid stabilization (mean±SD=2.0±0.5 days) and enhanced postdischarge follow-up (100%) were observed in the RFPP-S group compared with the control group (5.0±2.0 days, 50% [N=75], respectively) (p<0.05). Furthermore, RFPP-S, but not treatment as usual, was associated with a significant increase in well-being, resilience, flexible thinking, enhanced coping skills, and improved parent-child interactions (p<0.05). The rate of psychiatric readmission due to suicidality at 1 month was 0% in the RFPP-S group and 20% in the control group (p<0.05). At the 6-month follow-up, no psychiatric hospitalization or suicidal ideation was noted in the RFPP-S group, and sustained reductions in PTSD symptoms (lower CAPS-CA score) were seen (
Tables 1 and
2). In contrast, higher CAPS-CA scores were observed in the control group, and 32% of these youths had a psychiatric hospitalization at 6 months (
Table 1).
Table 1 shows that all RFPP-S recipients had a follow-up with their primary outpatient mental health provider within 1 week following discharge, and none had a PER visit or psychiatric hospitalization within 6 months following discharge.
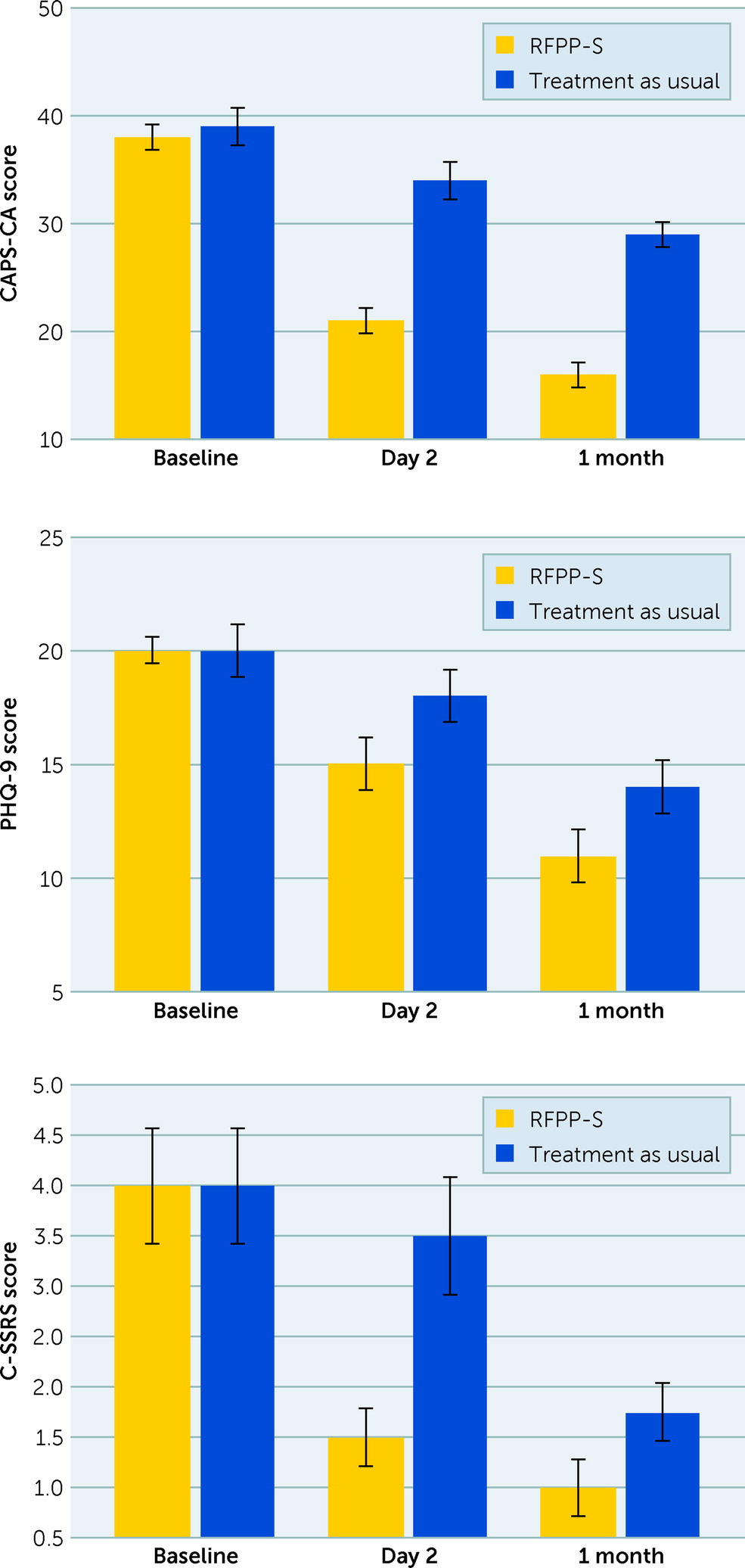
Figure 1 shows significant improvements in C-SSRS (score ≤2, with low risk for suicidal ideation; effect size=1.8, p=0.001), CAPS-CA (score reduction >15, effect size=2.7, p=0.001), and PHQ-9 (reduction of 25%, effect size=2.1, p=0.001) scores in response to RFPP-S, but not to treatment as usual, at day 2. These improvements were sustained in the RFPP-S group, but not in the control group, 1 month after discharge from the PER (
Table 2 and
Figure 1).
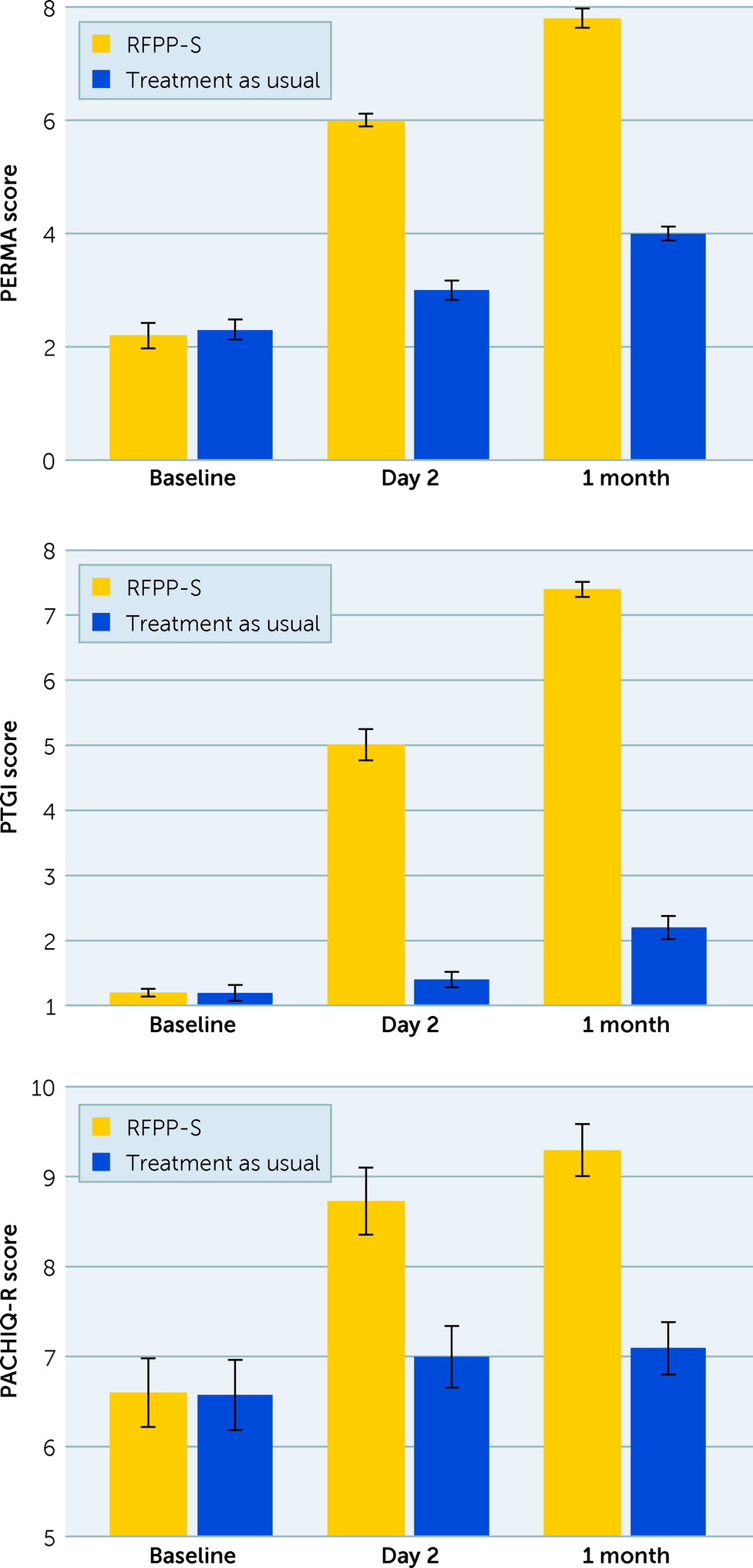
Figure 2 shows significant increases in PERMA (increased to >5, effect size=3.4, p=0.001), PACHIQ-R (increased to >7, effect size=2.1, p=0.001), and Posttraumatic Growth Inventory (increased to >4, effect size=6.5, p=0.001) scores in response to RFPP-S, but not to treatment as usual, which were maintained at 1 month after discharge (p<0.05).
Table 3 shows that RFPP-S was more likely to reduce the severity of RTLR, CAPS-CA score, and C-SSRS at day 2 than treatment as usual (OR=0.36, 0.38, and 0.43, respectively; p<0.05). Similarly, RFPP-S, but not treatment as usual, was associated with a sustained increase in positive biopsychosocial traits and parent-child interactions (p<0.05).
As
Table 3 shows, at the 6-month follow-up, the severity of core PTSD symptoms, RTLR, and suicidality risk remained reduced from baseline in the RFPP-S group, but not in the control group (p<0.05). CAPS-CA and C-SRSS scores—measures of PTSD severity and suicide risk, respectively—were 75% and 81% lower in the RFPP-S group compared with the control group (p<0.05).
Discussion
This study revealed several novel findings: RFPP-S—a brief trauma-informed, reminder-focused intervention in an emergency room setting that provides two reminder text messages or telephone calls for postdischarge mental health visits—was associated with reductions in core PTSD symptoms, RTLR, and C-SSRS score; successful adoption of safety skills; and rapid stabilization of acute crises. RFPP-S was linked to increases in well-being, resilience, posttraumatic growth, and parent-child interactions. Fifty youths with PTSD and suicidality in this study received RFPP-S at a PER and attended a mental health visit 1 week after discharge, and none had suicidality, a PER visit, or psychiatric hospitalization within 6 months following discharge.
More than half of the youths sought care in a PER as their first contact with mental health care services, and the PER served as an entryway to the mental health system for both youths and their families (
11).
PERs play a pivotal role in the early identification of youths at high risk for suicide, especially among those with PTSD, and present unique opportunities to provide early intervention to trauma-exposed youths and to prevent suicidal intent and behavior (
15,
16,
18–
22). Prior studies have shown that suicide screening in PERs establishes a safe context to discuss suicide risk with at-risk youths and their families, identify risk levels, engage youths and families in prevention efforts, and initiate early prevention strategies, such as linking youths to treatment (
15,
16,
18–
22).
Prior studies have revealed the effectiveness of brief suicide risk screening and intervention to prevent suicide attempt and have shown that adherence to postdischarge follow-up appointments, which can be incorporated into the daily standard of care for treating this population, can reduce suicide risk and the admission rate for psychiatric hospitalization (
15,
16,
18–
24). The current study confirmed prior studies and provided evidence that scalable trauma-informed screening tools can accurately stratify treatment approaches and monitor responses to therapy of youths at risk of PTSD.
We recently reported that RFPP tailored to core clinical features of PTSD is highly acceptable and feasible, is associated with a more robust reduction of core PTSD symptoms compared with trauma-focused cognitive-behavioral therapy, and is linked with more noticeable improvement of vascular function and inflammation and an increase in well-being and positive biopsychosocial traits (
17). RFPP-S consists of two extracted components of RFPP—trauma reminders and avoidance and negative cognitions—as well as safety planning and distress tolerance skill sets for youths with PTSD and their families and two reminder text messages or telephone calls for postdischarge mental health visits. RFPP-S focuses on enhancing recognition of trauma reminders, promoting enhanced adaptive coping strategies through shifting attention and treatment engagement, tolerating and bouncing back from distress, enhancing emotion regulation with flexible thinking, adhering to treatment, and increasing positive parent-child interactions and safety skills. This study confirmed prior studies and showed a direct association between RFPP-S and improved RTLR and core PTSD symptoms, reduced risk of suicide, and increased adherence to postdischarge follow-up appointments. Furthermore, RFPP-S was associated with improved well-being, enhanced contextual differentiation, improved coping skills while experiencing trauma reminders, improved parent-child interactions and distress tolerance, positive engagement, and adoption of safety skills with rapid acute crisis stabilization. These salutary effects have been associated with evidence of concomitant improvement of vascular function, decreased inflammation that correlated with hypothalamic-pituitary-adrenal axis normalization, reduced RTLR and core PTSD symptoms, and reduced major adverse events (
10,
17,
25,
26).
Clinical Perspective
The increase in prevalence of PER visits for at-risk youths, especially those with PTSD and suicidality, highlights the important role of PERs as a gateway for early identification of suicidality, for management of at-risk youths, and for referral of at-risk youths and their families to the mental health system (
5–
12,
15,
16,
18–
24). To the authors’ knowledge, the current study was the first to provide evidence that RFPP-S is a brief, feasible, and effective trauma-informed reminder-focused intervention for rapid stabilization of acute crisis that can reduce core PTSD symptoms and RTLR and promote safety skills among youths with comorbid PTSD and suicidality. It was also the first study to show that RFPP-S is associated with improved well-being; positive coping skills; and enhanced parent-child interaction, engagement, and adoption of safety skill sets. Finally, it provided evidence that the RFPP-S is linked to enhanced treatment engagement with postdischarge mental health visits, sustained remission of PTSD, reduced RTLR severity, adoption of safety skills, sustained reduced risk of suicide, and favorable clinical outcomes.
Limitations
This study had several limitations. This was a single-center, retrospective, nonrandomized, observational analysis of a large cohort of youths with comorbid PTSD and suicidality treated by one provider with either RFPP-S or treatment as usual. Thus, data acquisition for this study was unblinded. There was no placebo treatment group. A significant number of youths with comorbid PTSD and suicidality in both groups had received an age-appropriate therapeutic dose of an SSRI before PER admission and were kept on the same dose that they received at home prior to admission, without change in the first 48 hours of the PER visit. Information on any change in SSRI and/or dosage after day 2 at the OV-PER was not available for this study. Youths with PTSD and suicidality usually have more severe illness than those without both conditions. Using a nested, matched case-control design, we randomly selected comparable youths with equal severity of PTSD for inclusion in the control group receiving treatment as usual, and we used bootstrapping analyses to address possible rater measurement bias. Additional prospective studies and randomized controlled clinical-efficacy trials are warranted to further evaluate the effects of RFPP-S on early detection and optimal treatment of youths with PTSD and suicidality and on change in biopsychosocial traits.