Borderline personality disorder is a serious mental disorder characterized by a pattern of chaotic relationships, identity disturbance, difficulties in emotion regulation, and impulsivity. Although there are significant questions about the validity of categorically defined borderline personality disorder (
1), the borderline construct can also be understood as a proxy for a tendency toward general and severe personality pathology (
2–
5). Borderline personality disorder is highly prevalent, especially among individuals receiving services for general medical and mental health. Whereas the prevalence of this condition in the general population has been recorded at 1.4%–5.9% (
6,
7), prevalence among clinical populations is much higher. These prevalence rates range from >20% in psychiatric outpatient samples (
8) to >40% among high users of inpatient services (
9) and >60% among patients in forensic services (
10,
11). Additionally, people with borderline personality disorder are at a greatly increased risk for suicide—approximately 50 times that of the general population (
12).
Impairment in interpersonal functioning is a key characteristic of borderline personality disorder. These interpersonal difficulties manifest as conflict throughout the social networks of individuals with the condition, which contain more terminated relationships, such as former romantic partners and cut-off friendships, than the social networks of individuals without the condition (
13). In existing romantic relationships, symptoms of borderline personality disorder predict greater levels of dysfunction, including stress, conflict, partner dissatisfaction, and abuse (
14). These interpersonal deficits translate to increased frequency of conflict with parents, siblings, and friends (
15). The centrality of interpersonal problems to the disorder is demonstrated through the nine criteria for the condition in the
DSM-5, two of which explicitly relate to interpersonal difficulties: frantic efforts to avoid real or imagined abandonment and a pattern of unstable and intense interpersonal relationships characterized by alternating between extreme idealization and devaluation. However, most of the remaining criteria have implicit implications for interpersonal relationships (
16,
17). For example, suicidal behavior, gestures, and threats (criterion 5) of individuals with the disorder often have interpersonal triggers (
18). Because of the centrality, and frequent lethality, of these interpersonal problems for individuals with this disorder, social cognition—the process of thinking about others’ thoughts, intentions, feelings, attitudes, and perspectives—has been identified as a potentially important factor for understanding the disorder (
19).
Mentalizing and Borderline Personality Disorder
Research supports the idea that social-cognitive deficits may underlie the interpersonal problems associated with the disorder, but mixed results suggest that such deficits are apparent only when the social-cognitive task is complicated or highly emotionally arousing. For example, meta-analytic studies of emotion recognition in borderline personality disorder indicate that individuals with the condition do not show impairment compared with healthy control participants in recognizing emotions for negative or positive faces; however, when uncertainty is introduced via neutral or ambiguous faces, individuals with this condition are less accurate than control participants without the condition (
20–
22). Individuals with borderline personality disorder also demonstrate less accurate emotion recognition than control participants when complexity is introduced, such as when faces are merged with prosodic information, but show no impairment when the stimulus is simplified by presenting the faces and prosodic information separately (
23). This same pattern emerges in other social-cognitive constructs, including empathy and trust, indicating that the social-cognitive impairment associated with borderline personality disorder is apparent only in the face of highly complicated or emotionally charged tasks (
24). In addition to being triggered by complex tasks, the social-cognitive impairment characteristic of individuals with the disorder seems to be marked by an overattribution of intentions and thoughts to others (
25). Although an overattribution of mental states is not the only type of social-cognitive impairment experienced by individuals with borderline personality disorder, it appears to be the most replicated finding associated with the condition.
Inaccurate social cognition by individuals with borderline personality disorder tends to be characterized by going beyond the evidence and making inaccurate assumptions (24). In emotion recognition tasks with neutral or ambiguous faces, individuals with the disorder demonstrate a negative response bias (
21). A similar negative bias was found in impressions of characters in movies; individuals with borderline personality disorder ascribed more negative qualities to the characters than did control participants without the disorder (
26). This negative bias seems to generalize to mental representations; studies using projective assessment techniques have demonstrated that individuals with borderline personality disorder have more malevolent object worlds than healthy control participants and tend to attribute motivation to others in illogical ways (
27). In summary, the social-cognitive deficits associated with borderline personality disorder seem to manifest only in the face of complex and emotionally arousing stimuli and are characterized by an overattribution of mental states beyond what the evidence provides. In the interest of having a coherent theoretical framework by which to understand these findings, Sharp and colleagues (
17,
24) have suggested that the construct of hypermentalizing may be helpful.
Sharp and colleagues put forward a model to understand the unique social-cognitive problems encountered by those with borderline personality disorder. This model combines mentalizing and social-information processing theory to understand the nature of the social-cognitive deficits characteristic of this disorder. Mentalization refers to one’s imaginative capacity to reflect on the mental states of oneself and others and is a central mechanism behind much of social cognition and interpersonal interactions (
28). Optimal mentalizing is a balance between several polarities: between automatic and controlled, cognitive and affective, self and other, and internal and external. Automatic mentalizing happens quickly and without attention and is often emotional, whereas controlled mentalizing is slow and requires intention, drawing on top-down cognitive control (
29). Cognitive mentalizing uses thoughts, such as perspective-taking, whereas affective mentalizing uses emotions, such as empathy. Self-mentalizing is mentalizing of one’s own mind, whereas other-mentalizing is mentalizing the minds of others. Finally, external mentalizing is based on observable cues (e.g., a facial expression), and internal mentalizing is based on internal experience (e.g., thoughts and feelings). Optimal mentalizing requires flexibility and balance across all four poles and changes depending on the demands of the situation.
Sharp’s hypermentalizing model, which builds on the original mentalizing theory developed by Fonagy and Bateman (
30), posits that individuals with borderline personality disorder struggle to move flexibly across the four poles of mentalizing and instead rely solely on one or another extreme. This lack of flexibility and balance is exacerbated in situations that are emotionally taxing; when individuals with borderline personality disorder experience emotional and attachment hyperactivation, their ability to self-monitor and mentalize flexibly is reduced. As a result, in complicated or emotionally arousing situations, individuals with this disorder demonstrate mentalizing that is not context appropriate. In other words, there is an imbalance among automatic versus controlled, self versus other, cognitive versus affective, and internal versus external mentalizing. For example, when an individual fails to integrate between self- and other-mentalizing, they project what is in their own minds onto the minds of others (
17,
24). In this state, mentalizing is not reduced, but rather increased; an overattribution of mental states far beyond what there is evidence for, or hypermentalizing, dominates (
24,
31). Accordingly, hypermentalizing is described as “making excessively convoluted inferences on the basis of others’ social cues” (
32). For example, if a friend appears to be sad, an individual who is hypermentalizing may think “she hates spending time with me.” These mental state attributions lead to a further increase in emotional and attachment hyperactivation, which in turn further increase hypermentalizing. As such, addressing hypermentalizing directly during treatment is important to reduce symptoms of personality pathology (
31,
33).
A common approach to the assessment of hypermentalizing is to use the Movie for the Assessment of Social Cognition (MASC) (
34). The MASC is a widely used and ecologically valid measure of mentalizing that classifies errors in mentalizing into categories indicating no mentalizing, reduced mentalizing (or hypomentalizing), and excessive mentalizing (hypermentalizing) (
25). Although our review of the literature revealed three additional measures used to assess hypermentalizing—the Reflective Functioning Questionnaire (
35), the Hypermentalizing Questionnaire (Sharp C, Barr C, Vanwoerden S, and Long T, 2019), and the Self-Referential Hinting Task (
36)—there are problems with each of these that precluded their inclusion in the current review; evidence for the validity of the Reflective Functioning Questionnaire as a measure of hypermentalizing has been called into question (
37), and the Hypermentalizing Questionnaire and Self-Referential Hinting Task have been used only in one study each, making them inappropriate for meta-analytic review. We therefore included in our review only studies that used the MASC as a measure of hypermentalizing.
Studies using the MASC have provided strong evidence for the association of an impairment in mentalizing (i.e., hypermentalizing) with borderline personality disorder. In support of the association of this impairment and borderline personality disorder, many studies that used the MASC have found that individuals with the borderline personality disorder demonstrate higher levels of hypermentalizing than do healthy control participants (
38–
41) and control participants with psychiatric conditions (
33,
40). Furthermore, hypermentalizing has been shown to be positively associated with borderline personality disorder traits (
41–
44). Only one study failed to demonstrate an increase in hypermentalizing among individuals with borderline personality disorder compared with control participants with other psychiatric conditions (
45) and healthy control participants (
46), and two studies (
47,
48) failed to demonstrate a significant positive association between traits of hypermentalizing and borderline personality disorder. Importantly, no study has demonstrated relationships between hypomentalizing (reduced mentalizing) and borderline pathology nor differences between those with borderline personality disorder and healthy control participants in hypomentalizing.
Mentalizing and Other Psychopathology
Although the association between hypermentalizing and borderline personality disorder is well supported, research has demonstrated associations of other disorders with hypermentalizing on the MASC as well. Individuals with autism spectrum disorder (
49–
51), schizophrenia (
51–
53), attention-deficit hyperactivity disorder (
49), social anxiety disorder (
54,
55), psychogenic nonepileptic seizures (
56), and persistent somatoform pain disorder (
57) have also demonstrated increased hypermentalizing compared with healthy control participants. By contrast, several studies have failed to support the link between hypermentalizing and these other disorders. For instance, three studies (
38,
58,
59) failed to demonstrate differences in hypermentalizing among healthy control participants compared with individuals with schizophrenia, two (
60,
61) failed to demonstrate differences in hypermentalizing between healthy control participants and individuals with social anxiety, and one (
62) failed to demonstrate differences between healthy control participants and individuals with attention-deficit hyperactivity disorder. Additionally, although individuals with borderline personality disorder tend to show mentalizing impairment only with regard to increased hypermentalizing, people with other disorders tend to show both hypermentalizing and hypomentalizing (e.g., individuals with autism spectrum disorder [
49–
51] and schizophrenia [
38,
52,
53,
58,
59]). Furthermore, hypermentalizing on the MASC has been shown to be associated with affective components of psychopathy (
63), dimensionally assessed conduct disorder (
47), internalizing symptoms not specific to any disorder (
64), and suicidal ideation and attempts (
65). This evidence calls into question the specificity of the hypermentalizing impairment to borderline personality disorder.
Potential Moderators
To understand the differences in mentalizing ability across these studies, we also need to consider other factors that may affect mentalizing performance, specifically age, gender, and race. A previous meta-analysis of studies that used the MASC found that, among adults, age negatively predicts total mentalizing score and that women score significantly higher on correct mentalizing than men; however, the relationships between these variables and hypermentalizing score were not investigated (
66). Other studies have found that, among samples of adults with clinical conditions (
47) and samples of community adolescents (
67,
68), men make more hypermentalizing errors on the MASC than women do. The results for age have been mixed, with one study (
69) finding that younger adults made more hypermentalizing errors than older adults in a community sample, whereas others have found no relationship between hypermentalizing and age among samples of adults with clinical conditions (
47) or community adolescents (
67,
68).
No study has yet investigated the impact of race-ethnicity on MASC scores, but some studies (
70,
71) have found that neural response in social-cognitive networks decreases when the individual being mentalized is of a different race-ethnicity than the individual doing the mentalizing. Because all four characters in the MASC are White Europeans (the MASC depicts interactions in German. and the stimuli are dubbed for speakers of other languages), the race-ethnicity or cultural background of the participant may influence performance on the MASC. For example, White participants may perform better than non-White participants because of an in-group advantage in understanding subtle social cues. Because these participant characteristics may influence results on the MASC, it is important to account for the resultant variance in understanding differences among studies.
Current Study
With these considerations in mind, the goal of the current study was to use a meta-analytic approach to test the specificity of the hypermentalizing impairment to borderline personality disorder. Although meta-analyses have clarified the relationship between borderline personality disorder and specific social-cognitive abilities, such as emotion recognition (
21,
22) and theory of mind (
72), these meta-analyses did not fully investigate the hypermentalizing impairment associated with borderline personality disorder. Those investigating emotion recognition did not use tasks with sufficient complexity to elicit the social-cognitive deficits associated with borderline personality disorder, nor were they able to distinguish between hypermentalizing and hypomentalizing, because they included tasks that were not designed to differentiate between the two. Furthermore, although the specificity of hypermentalizing to borderline personality disorder has been tested in individual studies with control groups of patients with psychiatric conditions (
25,
33,
40), no meta-analyses have compared the performance of individuals with borderline personality disorder to that of individuals with other disorders. Thus, the specificity of hypermentalizing to borderline personality disorder has not yet been investigated meta-analytically.
To address the above gaps, we first conducted a literature review to identify studies that investigated the association of hypermentalizing with any form of psychopathology and that used the MASC. We selected the MASC because it is a widely used instrument that separates suboptimal mentalizing into hyper- and hypomentalizing and is relatively ecologically valid and emotionally salient, whereas other identified measures of hypermentalizing either have questionable validity or insufficient use to warrant inclusion in a meta-analysis. Additionally, because hypermentalizing has been theorized to distinguish individuals with borderline personality disorder from those with other psychopathology and to be associated with the severity of borderline personality disorder traits, we included studies that investigated the association of mentalizing performance with the severity of psychopathological traits as well as those that compared the mentalizing performance of a group with psychopathology to that of a healthy control group. The first aim of the current study was to conduct a meta-analysis to investigate the hypothesis that hypermentalizing is more strongly associated with borderline personality disorder than with any other disorder. We investigated this aim by conducting a meta-analysis to investigate the relationship between hypermentalizing and psychopathology and to examine borderline personality disorder as a moderator of that relationship. We hypothesized that borderline personality disorder would be more strongly associated with hypermentalizing than would other forms of psychopathology. The second aim was to understand the influence of potential sources of heterogeneity; specifically, the sample characteristics of age, gender, and race. To investigate this aim, we conducted moderator analyses on the full group of included studies for each of these characteristics. We had no a priori hypotheses for this aim because the previous literature is inconclusive.
Methods
We referred to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (
73) as a guide in conducting the meta-analysis. The PRISMA statement was also used as a guide in reporting the methods and results of the meta-analysis.
Measurement of Mentalizing
The MASC (
34) is a video-based assessment that evaluates everyday use of mentalizing. Participants watch a 15-minute film about four people getting together for dinner. The film is stopped at 45 points, during which the participants answer a multiple-choice question regarding a character’s thoughts and feelings. Participants choose from four answer options: an accurate choice, a hypermentalizing choice that ascribes mental states with little-to-no evidence, a hypomentalizing choice that only partially matches the accurate mental states, and a no-mentalizing choice unrelated to internal states. The number of times each type of answer was selected is calculated, resulting in four mentalizing scores: one indicating the frequency of accurate mentalizing and three indicating the frequency of each type of error. Additionally, four control questions unrelated to mentalizing are asked. The control score can be calculated by adding together the number of control items answered correctly and indicates general comprehension and attention. The MASC has been found to be a reliable tool for assessing mentalizing deficits among healthy adults (
34) as well as among adults and adolescents with psychopathology (
48). Only studies using the MASC have been included in the present study for several reasons: as an experimental task, the MASC does not rely on self-report; it is a an ecologically valid task with sufficient complexity to require integration across the automatic versus controlled pole, and thus exposes the deficits expected to be associated with borderline personality disorder; and it uses the framework of mentalizing, which separates suboptimal mentalizing into hypo- and hypermentalizing, allowing for the differences between these two types of responses to be detected.
Literature Search Procedures
We conducted a comprehensive literature review by searching PsycINFO, Social Sciences Citation Index, PubMed, and the ProQuest Dissertations and Theses databases. The search was conducted for articles published from January 2006 to December 2019. The start point was selected by considering the year that the MASC was published. To find all potentially relevant articles, searches were conducted using the term “Movie for the Assessment of Social Cognition.” Works that were identified as having cited the MASC validation article were also reviewed. All articles generated by the literature search were then assessed to determine eligibility for inclusion in the meta-analysis. Additionally, reference lists of included studies were searched for further relevant studies.
Inclusion and Exclusion Criteria
Studies met the following inclusion criteria: the study used the MASC; the study reported either a group comparison of hypermentalizing scores between individuals with a psychiatric diagnosis and healthy control participants or an association between hypermentalizing scores and a continuous measure of a psychiatric disorder; the article was written in English; an effect size was reported or sufficient information was included to calculate an effect size; and the article presented data that were not reported by another study included in the review.
Coding Procedure
A coding form was created to systematically record relevant information from each article. Study characteristics included on the coding form were report information (full bibliographic reference) and publication type (peer-reviewed journal article, dissertation, or unpublished manuscript). Coded sample characteristics included total N, mean age, percent female, and percent White. Information related to psychopathology and its measurement included specific DSM-IV or DSM-5 disorder and type of comparison (correlation, group difference, or both). Finally, Pearson’s correlation (r) was used as the effect size for all statistical analyses. Effect size was recorded for the association between psychopathology and MASC hypermentalizing score. A second coder coded 20% of the sample for reliability analyses. Discrepant codes were recoded until agreement was reached.
Data Analysis
Analyses were conducted in Excel and in R by using the dmetar, meta, and metafor packages. Random-effects modeling was used for meta-analytic calculations, and mixed-effects modeling was used for moderator analyses. Pearson’s correlation was recorded for the association between hypermentalizing and psychopathology in each study as the measure of effect size. For studies in which an effect size was reported in another metric or an effect size was not reported, but sufficient information was provided to calculate an effect size, effect sizes were calculated or transformed to r by using standard procedures. Positive effect sizes represent a positive association between hypermentalizing and psychopathological symptoms or instances where a group with psychopathology had higher hypermentalizing scores than a healthy control group. Negative effect sizes represent a negative association between hypermentalizing and psychopathological symptoms or instances where a group with psychopathology had lower hypermentalizing scores than a healthy control group. For studies that report multiple effect sizes (i.e., multiple measures of psychopathology), pooled effect size and standard error were calculated. For studies that reported an association for both borderline personality disorder and non–borderline personality disorder psychopathology, the non–borderline personality disorder effect size was excluded to avoid dependency in the data. Effect sizes were then converted to Zr by using Fisher’s transformation to control for the skewed distribution of r. Results of the meta-analysis were converted back to r when reported for ease of interpretation. Heterogeneity was calculated, and publication bias was investigated by using Egger’s linear regression. Egger’s linear regression tests for funnel plot asymmetry, which is indicative of publication bias.
To evaluate the hypotheses associated with aim 1, a meta-analysis for the association between hypermentalizing scores and psychopathology was conducted, and borderline personality disorder status was evaluated as a moderator by using moderator analysis. To address aim 2, moderator analysis was also conducted individually for the following moderators: mean age, percent female, and percent White. Moderators were excluded for analyses in which fewer than 10 studies reported the statistic, as advised by Fu et al. (
74).
Discussion
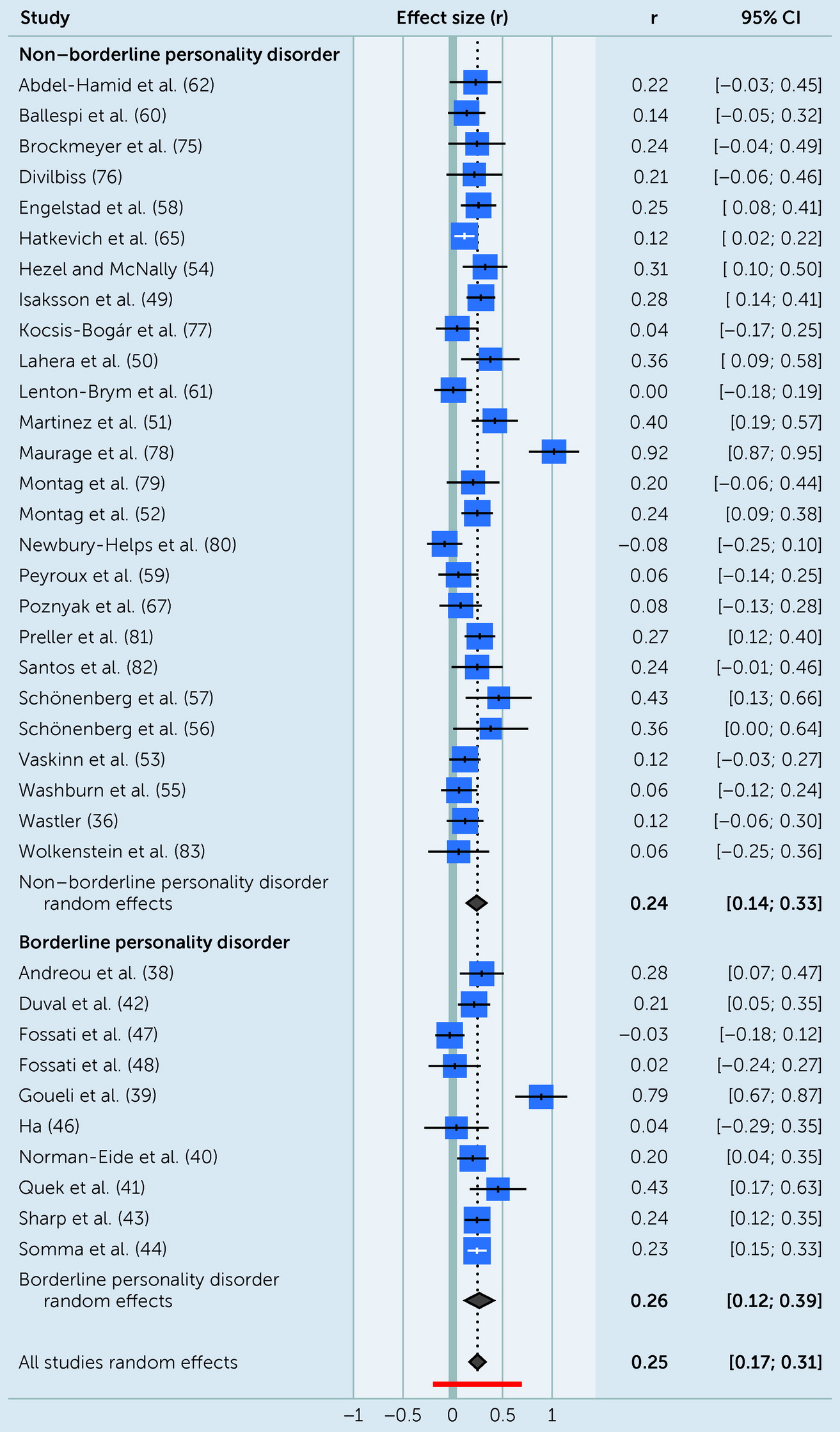
The aims of the current study were to evaluate the relative strength of the association between hypermentalizing and borderline personality disorder compared with other disorders and to assess the impact of moderators on the relationship between hypermentalizing and psychopathology. Both aims were assessed meta-analytically by combining and comparing studies that evaluated an effect size for the association between psychopathology and hypermentalizing score on the MASC.
Our hypothesis that borderline personality disorder would have a stronger association with hypermentalizing than other psychopathology was not supported. Although a positive association between hypermentalizing and borderline personality disorder was supported via meta-analysis, the magnitude of this association did not differ for borderline personality disorder compared with other disorders; both borderline personality disorder and other psychopathology demonstrated a robust association with hypermentalizing. Thus, we found no evidence for the specificity of hypermentalizing to borderline personality disorder. This finding suggests that hypermentalizing as measured by the MASC is related to psychopathology more broadly. However, to fully contextualize the implications of this finding, it is important to delve into the nature of the hypermentalizing construct captured by the MASC. Specifically, although resembling mentalizing required in real-life interactions, the MASC lacks two important characteristics of real-world mentalizing. First, the scenarios about which participants are asked to mentalize do not have personal relevance for the participants; the MASC asks individuals to reflect on the thoughts of actors in a movie. Second, although complex, mentalizing the characters in the MASC may be associated with less emotional salience than, for instance, attachment-related stimuli. These characteristics may be especially important in the context of borderline personality disorder, given the role of attachment hyperactivation in the hypermentalizing model of this disorder. Therefore, the question remains whether hypermentalizing in general or merely hypermentalizing in non–self-referential situations of relatively low emotional salience is broadly related to psychopathology. To answer this question, further research investigating the relationship between psychopathology and hypermentalizing that probes instances of attachment hyperactivation is necessary. This type of mentalizing may be better captured by using interview-based methods or instruments like the Self-Referential Hinting Task (
36), which asks participants to imagine themselves as a participant in hypothetical interactions before making inferences about the mental states of others. However, although it is not yet clear the extent to which other forms of hypermentalizing are related to broad psychopathology versus borderline personality disorder uniquely, there does appear to be a relationship between broad psychopathology and hypermentalizing as measured by the MASC.
A relationship between psychopathology in general and hypermentalizing raises several questions requiring further research. First, we recommend the exploration of hypermentalizing as an etiological factor behind risk for and severity of psychopathology in general, not just borderline personality disorder. Specifically, we recommend the investigation of mechanisms leading to hypermentalizing for various disorders. Although the relationship between hypermentalizing and various psychopathology was not found to differ in the current study, it is unclear whether this relationship is a result of distinct mechanisms for different disorders or to a shared cross-diagnostic mechanism. Second, should hypermentalizing be supported as a source of shared etiological risk for psychopathology broadly, we recommend the investigation of hypermentalizing as a potentially important transdiagnostic treatment target. For example, such a finding would provide support for further investigation of the use of treatments targeting mentalizing, such as mentalization-based treatment (MBT), for disorders beyond borderline personality disorder. MBT targets impaired mentalizing through a therapeutic focus on mental states—those of the patient as well as of others, including the therapist (
84). In the case of hypermentalizing, MBT specifically targets impairments in integration across poles of mentalizing that occur in situations of high emotional arousal and that lead to hypermentalizing (
85). The patient and therapist build flexibility and balance across these dimensions by working together to develop new models of minds in real-time interactions (
31). As a result, interpersonal functioning improves and symptoms alleviate. Indeed, one recent study (
86) found that for individuals with borderline personality disorder, high levels of hypermentalizing pretreatment were associated with improved interpersonal functioning. Furthermore, evidence supports the efficacy of MBT in the treatment of borderline personality disorder among adults and adolescents, and preliminary support has been found for its use in other disorders, such as eating disorders, depression, and self-harm (
87,
88).
Although no evidence was found in the current study to support the specificity of hypermentalizing to borderline personality disorder, challenges in the organization of psychopathology introduce two additional questions warranting further research. In particular, other studies have found evidence that borderline personality disorder is strongly related to both the p-factor (the common factor of psychopathology, potentially representing severity or risk of developing any form of psychopathology) (
89,
90) and the general factor of personality pathology, suggested to represent severity, affective dysregulation, or criterion A of the alternative model (
4,
91). These lines of research suggest that borderline personality disorder features may be common to all psychological disorders or borderline personality disorder may represent the same latent variable as one or both general factors (
4,
90). Considering the current study in light of these findings introduces the possibility that hypermentalizing may be specific to the borderline personality disorder construct if borderline personality disorder features present in other psychopathology account for the association between other kinds of psychopathology and hypermentalizing. This possibility is further supported by evidence suggesting that p-factor scores are sensitive to epistemic mistrust, or mistrust in the veracity of interpersonally transmitted knowledge, which has in turn been implicated in the development of mentalizing ability (
92). However, this is an open empirical question that can be the focus of future research.
For our second aim, we had no priori hypotheses for the moderator analyses, and, in fact, no significant moderator effects were found for age or gender. However, because significant residual heterogeneity was found among the reported effect sizes for the association between psychopathology and hypermentalizing, future research is warranted on other moderators that may explain this heterogeneity. For example, the strength of the association between psychopathology and hypermentalizing may differ for internalizing and externalizing disorders.
Meta-analytic studies are constrained by the limitations of existing research. The biggest limitation of the current literature may be treatment of race-ethnicity. Racial-ethnic demographic information was rarely reported, and when it was, samples were predominately White. Lack of diversity in sampling limits the generalizability of these results to non-Whites, and lack of race-ethnicity reporting prohibited the inclusion of race as a moderator, meaning that potential differences in the association between psychopathology and hypermentalizing caused by race could not be examined. We recommend a standard of inclusion of race-ethnicity and other culture-related demographic information in reports of psychological research. Additionally, future research should include more diverse samples and investigate associations among race-ethnicity, psychopathology, and hypermentalizing.
Although we found no evidence of publication bias, according to some estimates, the number of included studies was too small to be sufficiently powered to detect all types of publication bias by using Egger’s linear regression, especially in the borderline personality disorder group (
93). However, because the significant heterogeneity of the sample ruled out other tests of publication bias, such as failsafe N, Egger’s was the most appropriate test for this body of literature. Thus, despite this lack of evidence, publication bias could not be fully assessed, so the possibility remains that nonsignificant results, which would diminish the overall effect size, were unpublished.
Because the current meta-analysis was based on data from one measure of mentalizing, we were limited by the properties of that measure. The MASC was chosen because it is a commonly used, complex, ecologically valid, experimental task that separates suboptimal mentalizing into hyper- and hypomentalizing. Thus, it is consistent with the framework of mentalizing previously used to detect mentalizing deficits among individuals with borderline personality disorder. Despite these strengths, the MASC represents only one theory of mentalizing and may be biased against non-White participants because of its entirely White European cast of characters.