Ms. C identified as a Spanish-speaking, cisgender, heterosexual, single female in her 50s. She was separated from most family and living with roommates in a two-bedroom apartment. Diagnosed with early-stage hormone receptor positive breast cancer several years before the COVID-19 pandemic, she was treated with lumpectomy followed by chemotherapy, radiation therapy, and tamoxifen. At the time of this treatment, Ms. C’s disease was in remission. She worked outdoors full-time collecting recyclables, earning low daily wages. Despite working 48 hours/week, she experienced financial insecurity and, at times, hunger. She received no public benefits other than Emergency Medicaid and relied on daily prayer as a coping ritual.
During a routine oncology surveillance appointment, Ms. C appeared distressed, yet she endorsed no symptoms on the nine-item Patient Health Questionnaire (PHQ-9) administered by a triage nurse. Regardless, the oncologist referred Ms. C to behavioral health care on the basis of perceived emotional distress.
At the cancer center, nurses administer the PHQ-2 and/or PHQ-9 (
1) verbally at each encounter and populate responses into the electronic medical record. Although a score ≥10 or endorsement of suicidal ideation warrants a behavioral health referral, patients, such as Ms. C, are sometimes referred after endorsing no or minimal symptoms. This practice is supported by studies showing that patients choose not to disclose depression symptoms to health care providers because they believe that depression falls outside the purview of nurses and physicians (
2).
At the time of Ms. C’s referral, the behavioral health team was integrated within an urban cancer center serving a low-income adult population from an underserved community, with 90% of patients from racial-ethnic minority groups. The team consisted of two providers: a lead psychologist (A.H.) and a clinical psychology graduate student (I.M.) (both participated in the care of this patient). Both of us worked remotely during the surge in COVID-19 transmission, when the hospital’s region became the epicenter of the pandemic. The COVID-19 pandemic significantly disrupted cancer care (
3) and exacerbated baseline disparities in cancer outcomes among underserved communities as COVID-19 disproportionately affected patients from minoritized racial-ethnic groups. These patients were underinsured, experienced social isolation and financial stress, and continued to work in the community despite high transmission rates (
4).
During her initial behavioral health assessment 3 days after referral, Ms. C acknowledged financial and housing insecurity. Upon administration of the PHQ-9 by the psychologist, Ms. C obtained a score of 21 (severe depression with suicidal ideation) (
Table 1). Ms. C’s treatment consisted of 13 half-hour psychotherapy visits, provided by telephone while Ms. C, on breaks from work, found a private place in the community to talk. Ms. C was offered video sessions but declined because she did not have internet access. Sessions took place twice per week and tapered to once per week when symptoms lessened. Ms. C expressed satisfaction with telephone visits and did not miss any phone sessions during the 3-month treatment period. During this time, televisits were provided at no cost, allowing Ms. C to engage in a treatment that would otherwise have been prohibitively expensive.
Suicide risk factors included chronic illness, financial distress, housing problems, history of nonsuicidal self-injury, and having planned to end her life in the weeks leading up to the initial consultation. Ms. C reported that her depressed mood began approximately 2 weeks before referral and that she had thought of hanging herself in her bedroom 1 week before the appointment. Thoughts of harming herself were present several days in the week leading up to the visit, but Ms. C cited no current suicidal ideation, plan, or intent during the first session. Problems with a roommate and housing insecurity were identified as precipitating factors of suicidal ideation. She endorsed one prior depressive episode 4 years prior, which was resolved without treatment. Mitigating factors included strong religious beliefs against suicide; barriers to accessing lethal means (no access to firearm); demonstrated resilience to overcome past hardship; strong connection to the medical institution and providers; and having no history of substance use, chronic persistent mental illness, family history of suicide, or suicide attempts.
During the first session, we (team of graduate student and lead psychologist) focused on hopelessness and suicidal ideation. Using an empathic, autonomy-giving demeanor to help the patient form a safety plan, we educated the patient about options for urgent mental health care, including visiting the emergency department (ED) for further evaluation and medication. Ms. C said she would go to the hospital but not right away. She wanted to finish her day’s work so she could afford food and rent. She cited COVID-19 as a reason to avoid the ED and inpatient units and expressed interest in psychotropic medication. We validated her concerns and reassured her she would be able to receive medication. We also encouraged Ms. C to talk about her experience of trauma and stress and provided contact information for the local crisis management team. When asked further about past trauma and immigration history, Ms. C chose to not disclose these details in order to protect her identity, as is common among undocumented individuals in our patient population. Our hospital policy is to treat all patients regardless of immigration status. When patients express reluctance to disclose immigration details, therapists respond with compassion and respect their privacy, engendering trust.
When Ms. C expressed fear about contacting the crisis service herself, we validated her anxiety about contacting another stranger to talk and offered to contact the crisis service with her. We connected the call and introduced the service. The crisis mental health worker informed Ms. C about the process by which she could receive confidential, free counseling any time in Spanish and further guidance about emergency care; this phone call demonstrated the feasibility of reaching someone immediately. Ms. C expressed appreciation and agreed to consider an ED visit that evening and to call the mental health crisis service if needed. We affirmed Ms. C’s participation in safety planning, encouraged her to follow up with her outpatient behavioral health visits through the cancer center, and informed her that her suicidal ideation, although distressing, would abate and that her depressive symptoms would lessen with help and time.
During the subsequent sessions, Ms. C provided feedback that her initial session resulted in relieved isolation and increased hope. Her suicidal ideation did not recur. We provided additional education and recommendations and set treatment goals through open-ended inquiry. We also provided psychoeducation on common mood-altering side effects of long-term maintenance therapy for breast cancer (tamoxifen) and recommended psychotropic medication evaluation by Ms. C’s primary care physician to improve mood and insomnia; she was prescribed mirtazapine. (As is common in our public hospital system and community, highly specialized providers like psychiatric psycho-oncologists are unavailable, and availability of general psychiatry is limited. Patients with uncomplicated psychotropic medication needs are referred to primary care providers who have access to consultation by a psychiatrist if needed.) Safe housing was identified by Ms. C as the main treatment goal because she did not feel confident asking for help and felt alone in her pursuit of housing alternatives.
Ms. C’s living circumstances became intolerable during the surge in COVID-19 cases when dangerous levels of community infections prohibited leaving the home. She lived with roommates unfamiliar to her, and a male roommate repeatedly presented to common spaces unclothed, played loud music, and exhibited poor hygiene. His refusal to vacate the premises led Ms. C to feel trapped, hopeless, and fearful of seeking governmental support services because of her immigration status.
Sessions 4–9 focused on cognitive skill–building to empower Ms. C to rely on available support and resources. Our primary therapeutic strategies included challenging negative thoughts about herself, encouraging social support network discovery, and increasing exposure to community support. Ms. C initially described her circumstances as complete isolation, but we challenged and reframed this idea. We bypassed Ms. C’s initial resistance to describing her social experiences in detail by normalizing her experience of isolation in the context of COVID-19. We encouraged her to seek counterevidence through empathic inquiry and suggestion and framed her strong connection to her health care providers as an exception to her view of being isolated.
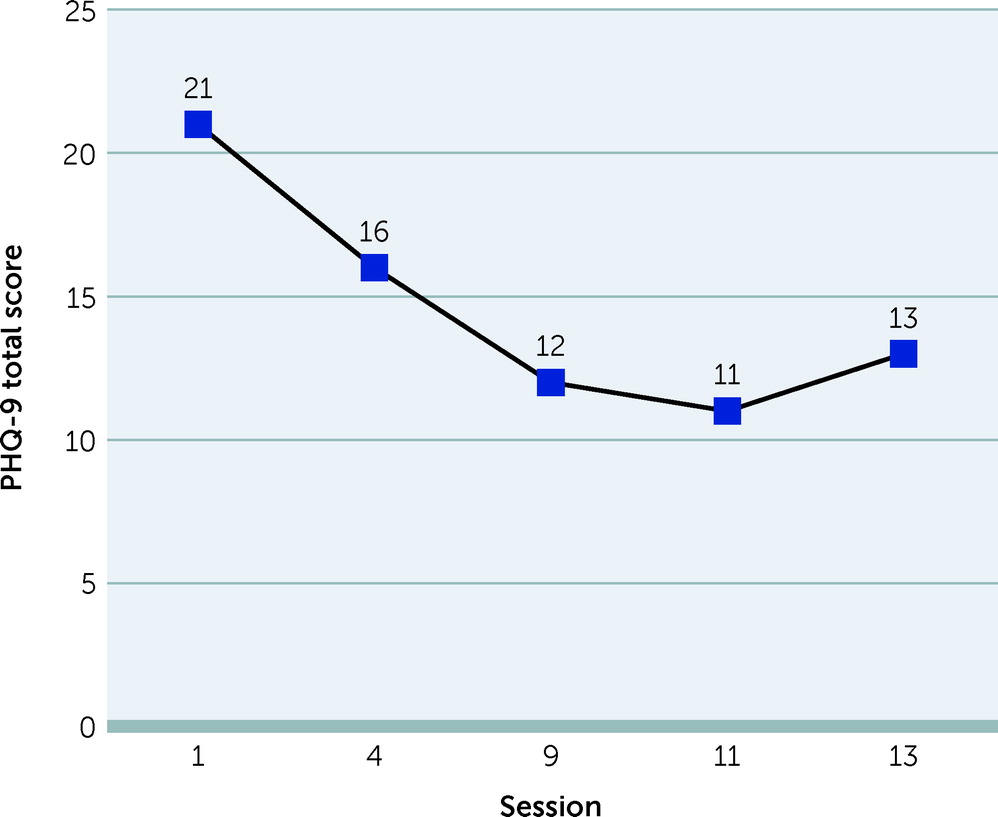
Upon detailed guided discovery, we uncovered two people who helped Ms. C and responded to her calls for help, however infrequent. One source of practical support was a neighbor, and another was a friend who provided emotional support. We reframed Ms. C’s belief of her total alienation by encouraging a more realistic view that support sources had made time for her despite their own caregiving responsibilities, which spoke to the strength of these relationships. Ms. C additionally disclosed that she visited church regularly, although she did not speak with anyone; this was identified as a place of potential social support. Additionally, we referred Ms. C to a Latinx community-based organization to access food and legal and financial resources, allowing Ms. C to seek help from nongovernmental sources. Furthermore, this referral gave Ms. C an opportunity to practice help-seeking skills (e.g., exposure). Through these interventions, we expanded Ms. C’s perceived social support sources, and her depressive symptoms progressively decreased (
Figure 1).
During sessions 10–13, Ms. C’s depressive symptoms remained stable and in the moderate range (
Table 1). Ms. C drew on her confidence and belief in her connectedness to others to plan and autonomously execute strategies to obtain safer housing. We role-played how Ms. C would approach her landlord and how she would manage if the landlord did not speak Spanish. The plan was successful, and her landlord approved a transfer to another apartment. She expressed pride in her accomplishment and assertiveness and decided to stop psychotherapy after securing housing. She continued her antidepressant medication. We encouraged Ms. C to reach out if she wanted to resume psychotherapy at any time.
Discussion
Researchers predicted a pandemic-related mental health surge that is now upon us (
5). Cancer patients in underserved regions experience compounding tragedies, such as housing and food insecurity, racial inequity, and income loss. Cancer survivors like Ms. C will present more often to mental health clinicians as survivorship increases, which is consistent with findings that the mental health impact of cancer is significantly worse for Black and Latinx populations compared with non-Hispanic Whites (
6). Although the efficacy of psychotherapy for depression, anxiety, and distress among cancer patients is well established (
7), providers must be prepared to adapt treatments to address the psychosocial stressors, beyond cancer and COVID-19, faced by underserved and underprivileged populations.
Our case illustrates how crisis psychotherapy provided by telephone was used to effectively deliver evidence-based health care during the pandemic to a cancer patient living in poverty (
8,
9). In our discussion of Ms. C, we considered the role of disaster psychiatry interventions to manage distress and maintain functioning. Specifically, we followed the five principles of disaster psychiatry (
10,
11) while adhering to psycho-oncology guidelines for assessing and treating distress (
12). Although no clinical trials of disaster psychiatry interventions were found in the literature, strong justification exists for these empirically supported, expert-identified principles, which include promoting a sense of safety (e.g., developing adaptive cognitions and coping skills, use of grounding techniques), promotion of calming (e.g., breathing and relaxation techniques, psychoeducation, and normalization of stress responses), promoting self-efficacy (e.g., cognitive-behavioral therapy techniques that foster patient autonomy and mastery over stressors), promoting connectedness (e.g., by increasing emotional and practical support), and instilling hope (e.g., interventions aimed at decatastrophizing, future planning, setting novel and achievable expectations) (
11).
The five principles of disaster psychiatry have been studied among individuals experiencing homelessness during the pandemic in a rapidly implemented response program in which no overdoses or suicide attempts during the follow-up period occurred (
13). A model informed by the five principles was also used during the pandemic with cancer patients in a private academic medical center through telehealth (
14); however, no effectiveness data are available. Another disaster model intervention implemented by Doctors Without Borders concluded that brief psychodynamic/interpersonal psychotherapy resulted in increased functioning and reduction in symptom severity after humanitarian crises (
15). This model utilizes similar strategies as the five principles, emphasizing empathy, creating a holding environment for calm and safety (
16), listening to externalized patient trauma, and referring to resources.
Through our interventions with Ms. C, we expanded the five-principle model by identifying an application of psychotherapeutic technique to accomplish framework goals, with an emphasis on establishing a safety plan for suicidal ideation (promotion of safety) and then strengthening connectedness by using cognitive-behavioral strategies to challenge negative perceptions of oneself (promotion of connectedness). Therapists’ collaboration with community-based resources were critical. Providing psychoeducation, normalizing cancer treatment side effects, and encouraging antidepressant medication contributed to establishing calm (promotion of calming through normalization and psychoeducation). Our demeanor was highly engaged, affirming, autonomy-giving, active, and problem focused (promotion of self-efficacy). This engagement style helped Ms. C remain in treatment long enough to make critical life changes and improved functioning. Ms. C remained employed and did not miss workdays.
Several situations surfaced during this case that may be of interest to clinicians working with vulnerable cancer patients. We followed psycho-oncology guidance requiring valid and reliable screening for distress, screening at key intervals of treatment, and triaging patients to the level of care needed on the basis of symptoms (
17). We also used screening to guide treatment interventions, and, importantly, Ms. C’s suicidal ideation was identified during the administration of the PHQ-9 by the psychologist. Our case demonstrates, however, that screening does not always provide an accurate measure of severity, especially when considering language barriers and social stressors, which must also be assessed. Without the oncologist’s ability to acknowledge Ms. C’s distress, she would not have been referred to behavioral health care. Screening tools are important, but training staff to perceive and address distress directly is essential, as is training in administering screening measures in a culturally sensitive manner, in the patient’s preferred language, and using interpreters when appropriate.
An additional issue of relevance for behavioral health providers providing care to underserved populations with cancer is flexibility regarding patients’ location during the peak of the pandemic. Therapists obtained patients’ locations in case of emergencies, and risks and benefits of these sessions were discussed and documented before proceeding. Patients ideally receive telehealth services from their homes, but flexibility allows access for homeless and hard-to-reach patients during a crisis. Ms. C’s high-risk status as a cancer patient precluded hospital visits because of high community transmission of COVID-19, while the high-risk situation in her home that precipitated suicidal ideation precluded her from feeling safe engaging in psychotherapy in her residence.
Ms. C needed safe housing and community-based support. However, without first challenging her negative thoughts regarding her ability and efficacy in seeking support, she might not have accessed housing alternatives. Addressing social determinants without providing therapeutic support can at times be less effective for patients experiencing depression and social stressors.
There were limitations to this case study to consider. The lead psychologist in this case spoke English, and, despite use of interpreting services, connection with the patient was hindered by language discordance. Communication and comprehension may be limited when interpreters are used to provide services to non-English speakers, given the lack of guidelines and training on mental health interpreting (
18,
19) and the scarcity of providers able to speak languages other than English (
20). Using an interpreter may have affected Ms. C’s choice to not disclose immigration-related trauma. Ms. C may have been more open to disclosure with language-concordant care or continued treatment. Offering interpreter services, however, allows for the provision of nondiscriminatory services to communities with languages other than English—consistent with the Patient Protection and Affordable Care Act (
21). Additionally, televisits through videoconferencing might have increased disclosure; however, videoconferencing was not possible in this case because of the patient’s lack of internet access. Although studies of telehealth for cancer patients reveal promising results in the treatment of mood symptoms (
8,
9), research on the efficacy of telephone versus telehealth services delivered through video is scarce (
22).
Conclusions
Ultimately, our experience with this patient underscored that attention is needed to operationalize crisis psychotherapy models, develop methods across patient populations, and train mental health workers to implement crisis psychotherapy during future disasters (
23).