Major depressive disorder is a serious mental illness and is among the leading causes of global disability (
1,
2), with major health, economic, and social consequences (
3,
4). The disorder is associated with reduced quality of life (
5) and hampered psychosocial functioning and cognition, including deficits in attention and speed of execution (
2,
6). Quality of life is partly determined by an individual’s perception of their health status and position in their sociocultural context in relation to their expectations and values (
5). Studies of depression, including those using interpersonal psychotherapy (IPT) in Iran, have shown that patient-rated increases in quality of life are associated with improved mental health (
7).
In Iran, the prevalence of depression in the general population is 25%–35%, and depression is about twice as prevalent among women than among men (
2,
4). With respect to gender-based social roles, women are more interpersonally oriented and play key roles in families, parenting, and upholding cultural traditions within the community, whereas men are more achievement oriented, with external career and goal-oriented values (
4). Thus, women with depression in Iran may be especially amenable to an interpersonally focused therapeutic intervention.
IPT is an evidence-based and time-limited (eight to 16 sessions) psychotherapy for depression that underscores the importance of interpersonal relationships in the genesis of mental disorders. As an acute, affect-focused, structured depression treatment, IPT focuses on stressful relational life events, including grief, social role transitions, role disputes, and interpersonal deficits, that are temporally linked to the onset or worsening of depression symptoms and encourages patients to connect with people who can offer them support (
8–
10). IPT has demonstrated transdiagnostic effectiveness globally, and several studies of IPT have been conducted in Iran with women with subclinical depression symptoms (
7,
11–
13). However, IPT has never been studied as a treatment for major depressive disorder among Iranian women. In Iran, cognitive-behavioral therapy and medication are typically used as depression treatments. In light of the strong evidentiary base for IPT and the lack of studies of IPT among women with major depressive disorder in Iran, this pilot trial sought to fill a gap in the literature.
The aim of this study was to conduct a preliminary investigation of the effects of IPT on depressive symptoms and quality of life among women with major depressive disorder in the city of Isfahan, Iran.
Methods
This study was approved by the Iran National Committee for Ethics in Biomedical Research (IR.IAU.KHSH.REC.1400.018) and registered with the Iranian Registry of Clinical Trials (IRCT) (IRCT20210706051804N1). The IRCT is a primary registry in the World Health Organization Registry Network, overseen by the Ministry of Health and Medical Education and hosted by Iran University of Medical Sciences.
Assessments of depression and quality of life were administered pre- and posttreatment (i.e., at baseline and 12-week follow-up) by using the validated self-report Beck Depression Inventory–II (BDI-II) (
14–
16). The BDI-II evaluates depressive symptoms on a scale from 0 to 63, with higher scores indicating higher levels of depression. Scores of 0–13 indicate subclinical symptoms of depression, 14–19 mild severity of depression symptoms, 20–28 moderate severity, and 29–63 severe severity (
14–
16). The brief version of the World Health Organization Quality of Life Questionnaire (WHOQOL-BREF) is a 26-item self-administered instrument consisting of four domains: physical, psychological, social relationships, and environmental. Raw domain scores are transformed to a 0–100 scale for ease of comparison, with higher scores indicting better quality of life. The WHOQOL-BREF has been tested and shown to be reliable in an Iranian sample (
7,
17,
18).
Women ages ≥18 diagnosed as having depression by a general medical doctor in a general practice setting were referred to the research study (N=56). Potential participants were then screened for study eligibility with the BDI-II and the Structured Clinical Interview for DSM-5 Disorders (
19), administered by the first author (N. R. A.). Inclusion criteria were being at least 18 years old and female and having a BDI-II score >30, a diagnosis of major depressive disorder with a current depressive episode, and the ability to participate in all informed-consent procedures. Exclusion criteria included having obsessive-compulsive disorder (OCD), bipolar disorder, posttraumatic stress disorder (PTSD), current psychosis, current substance misuse, or acute suicidal ideation. Fifty-six women were screened, 19 were ineligible, and seven declined to give consent. Reasons for ineligibility included not meeting criteria for major depressive disorder (N=4), depression symptom severity (N=6), OCD (N=2), bipolar disorder (N=3), PTSD (N=1), current psychosis (N=1), current substance misuse (N=1), and acute suicidal ideation (N=1).
Eligible participants (N=30) were randomly assigned to either IPT (N=15) or a waitlist control (WLC) group (N=15). The participants were randomly assigned to each group in a 1:1 ratio by a computer program. The IPT intervention consisted of 12 individual treatment sessions, each 50 to 60 minutes long and administered by the first author (N.R.A.), that followed IPT therapeutic guidelines (
8). The therapist was trained and supervised by an Iranian psychiatrist (H.Z.) with many years of clinical experience in providing IPT to patients in Iran. Neither the patients in the IPT group nor those in the WLC group were receiving pharmacotherapy at the time of the study. Although this study was conducted during the COVID-19 pandemic, all individual sessions were conducted in person. The WLC group did not receive any other treatments during the assessment period (the period of waiting for their IPT treatment). According to the protocol and in compliance with ethics standards, patients in the WLC arm received IPT when the intervention-arm treatment was completed, after the study ended.
Descriptive statistical methods, including mean and standard deviation, were used to summarize the data. Inferential statistics, including multivariate analysis of covariance (MANCOVA), were conducted by using SPSS, version 24. MANCOVA was selected to analyze and compare posttreatment scores between groups because of the small sample and for a balanced design (equal numbers of participants in each group). Analyses were conducted with depression and quality of life as dependent variables, group assignment as the independent variable, and pretreatment (baseline) values of variables as covariates in the model.
Results
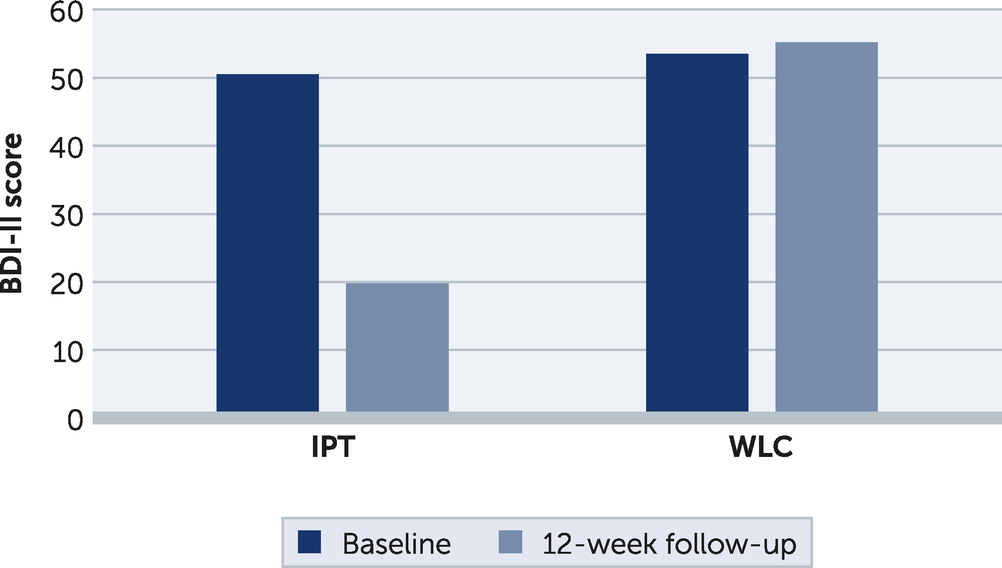
The results showed no significant differences in demographic or clinical variables between the IPT (BDI-II mean±SD=50.47±7.60; WHOQOL-BREF mean±SD=64.36±18.79) and WLC (BDI-II mean±SD=53.53±4.17; WHOQOL-BREF mean±SD=55.86±28.52) groups at baseline (
Table 1,
Figure 1). The mean±SD age of participants was 35.90±10.76 years, with a range of 20–50 years. Sixty-three percent (N=19) of patients were married, 43% (N=13) had a high school degree or less, and 57% (N=17) had postsecondary education, ranging from several years to earning a doctorate (
Table 1). As part of the informed-consent procedures, all participants agreed to attend all 12 sessions of IPT if they were assigned to this condition. All IPT participants attended all 12 IPT therapy sessions, and no participants left the study in either treatment condition.
After we controlled for baseline scores, the results showed statistically significant differences in poststudy depression symptoms as measured by the BDI-II (F=155.1; df=1 and 26; p<0.001; Cohen’s d=4.76) and in poststudy quality-of-life scores on the WHOQOL-BREF (F=137.5; df=1 and 26; p<0.001; Cohen’s d=4.16), with better outcomes on both measures for the IPT group.
Discussion
This pilot study provides preliminary evidence of the usefulness of IPT as a treatment for major depressive disorder among women in Iran. The results showed statistically significant differences in depression and quality-of-life scores over time between the study groups, suggesting that IPT may be a promising approach to reduce depression symptoms and improve quality of life in this population. Although IPT previously has been evaluated in Iran for women with subclinical depression (
7,
11–
13), it has never been examined as a treatment for women with major depressive disorder.
IPT is underused in Iran, despite being evidence based and recommended in many consensus depression treatment guidelines, and in some countries therapists have only limited access to training and supervision. This pilot study provides initial support for using IPT in this context. Of note, this study was done during the COVID-19 pandemic, which may have further contributed to interpersonal stressors. Indeed, IPT’s emphasis on interpersonal factors suggests that this approach may be especially relevant to Iranian women.
IPT is based on the premise that depression, regardless of its severity, phenomenology, or possible factors and causes, occurs in an interpersonal context and can be treated accordingly (
8). In addition to acute symptom remission, potential long-term benefits of this treatment include improved social functioning and prevention of symptom recurrence (
7,
11–
13).
Several cultural and gender-based predisposing, precipitating, and perpetuating etiological and vulnerability risk factors affect women in Iran. Social status, gender-based violence, inequities, discrimination, and dysfunctional relationships in families and communities may increase women’s vulnerability to depression (
2,
4). In addition, Iranian culture is not individualistic and values relationships, especially family ties. Adult children, especially daughters, are often expected to live with their parents until they marry, in accordance with religious practices. Iranians also presume that family members will ask for assistance in times of need and maintain close relationships with their family of origin, even when married or living far away. In Iran, respect for parents, elders, and individuals with a high social status is highly valued. These individuals are assumed to have authority over others; therefore, it is not permissible for a person of lower social status to disagree or be assertive with them or to directly confront or argue with them, as might be done in Western cultures.
Because of these cultural values, resolving disagreements respectfully with elders in the context of IPT role disputes might be challenging or unacceptable in some Iranian families, necessitating cultural adaptations of IPT for women in Iran. Thus, IPT therapists sometimes focus on social role transition (rather than on role disputes), concentrating on the fact that patients are now adult children with opportunities to understand and modify how they manage difficult interpersonal relationships and conflicts with parents, elders, or individuals with a high social status. In addition, in Iran, women traditionally value collective, nonindividualistic aspects of culture, such as marriage and the social role of being a homemaker. In recent times, individualist vocational aspirations have become more commonly held by all genders, which can sometimes underlie disagreements or nonshared expectations associated with the onset or worsening of depression among women. Taken together, cultural values about relationships and family, along with both gender-based violence and inequities, provide a rationale for using IPT as a promising depression treatment for Iranian women with depression.
Seeking and receiving mental health care has been historically stigmatized in Iran, but recent cultural shifts have increasingly normalized and even prioritized seeking guidance or treatment. Trends have been observed of individuals seeking professional support to aid with the selection of vocational goals, with a growth in the fields of educational psychology, industrial psychology and marketing, marital counseling (from engagement to conflict), and counseling for children. Although some pockets of Iranian society remain opposed to psychotherapy and stigmatize psychiatric disorders, a majority of Iranians accept clinical psychology and psychotherapy as essential parts of health care.
Limitations of this study include its small sample. The data were drawn from women patients in Isfahan, Iran, and the findings may not be generalizable to other Iranian populations. Additional limitations include the absence of independent ratings by assessors blinded to group allocation, a weak comparator condition, and the absence of externally rated fidelity measures to ensure IPT quality. Of note, in this initial pilot study, we opted to use a low-intensity comparator condition (i.e., WLC) to increase the likelihood of detecting a difference between the active treatment and the control condition. This approach is appropriate for early-phase studies such as this one to avoid prematurely disregarding a promising treatment because of a seeming absence of effect in an underpowered trial (
20). We recognize that having no missing data might be unusual for a clinical trial. Having a complete data set without missingness can likely be attributed to the informed-consent procedures, the strong desire of patients for free treatment, and Iranian cultural values related to rule following and to potential reluctance to disappoint a medical provider. Subsequent studies should be adequately powered to detect differences between IPT and an active comparator. In addition, all individual psychotherapy sessions were conducted in person by the first author (N. R. A.), which could increase the possibility of confounding therapist effects with treatment effects. Future randomized controlled studies with larger samples, independent ratings by assessors blinded to group allocation, and active comparator arms should adapt IPT and examine the treatment for other Iranian clinical populations, including individuals with bipolar disorder or somatic symptom disorders.
Conclusions
Treatment for depression among Iranian women diagnosed as having major depressive disorder by using IPT led to reduced depression symptoms and improved quality of life. IPT should be formally evaluated for its effectiveness as a depression treatment in Iran in a larger randomized controlled trial.
Acknowledgments
The authors thank Paula Ravitz, M.D., F.R.C.P.C., who provided invaluable support along the way. The authors also thank the individuals who participated in this research project and the clinicians and staff who contributed to the conduct of this trial.