Psychiatric problems are frequent after road traffic accidents. An immediate intervention following trauma—psychological debriefing—has been widely recommended as a means of helping with initial distress, and also of preventing later post-traumatic symptoms (
Bisson & Deahl, 1994). Services have been established for those at high risk following disasters and in other post-traumatic situations. Despite the clinical enthusiasm for psychological debriefing, there have been few attempts to evaluate its efficacy (Raphael et al., 1995). There have been no attempts to evaluate group psychological debriefing in randomised trials. A Cochrane Review (Wessely et al., 1998) of the limited evidence from randomised controlled trials of individual debriefing concluded that it was ineffective in preventing later post-traumatic symptoms, and indeed that there were indications that it exacerbated such difficulties.
We have previously described the outcome at 4 months in a randomised controlled trial of 106 patients consecutively admitted to hospital following a road traffic accident and who underwent early debriefing, mostly within 24–48 h (
Hobbs et al., 1996). We concluded that psychiatric morbidity was substantial 4 months after injury, and there was no evidence that debriefing had helped; indeed, there were indications that it might have been disadvantageous. A more recent account of a series of 40 trauma clinic attenders re-assessed at 3 months following the trauma reported similar findings (
Conlon et al., 1999). However, there remain many unanswered questions about debriefing interventions following road accidents and other trauma, which are of theoretical and clinical importance. We now report a 3-year follow-up of the sample on which we reported previously.
Method
Participants
The subjects were consecutive victims of road accidents admitted to the John Radcliffe Hospital in Oxford (we excluded those who had no memory of the accident or were intoxicated at the time of the accident). They were aged 16–65 years and residents of Oxfordshire or adjacent areas. All those who agreed to participate were allocated by a system of random numbers either to intervention or to a non-intervention control group. Our subjects were interviewed by a research worker within 24 h of the accident or as soon as they were physically fit to be seen. They were followed up at 4 months and again at 3 years.
Baseline measures
The length of stay in hospital was classified as “overnight” (1), “under 3 days” (2) and “more than 3 days.”
Follow-up measures
Impact of Event Scale (IES). The total score (sum of intrusion and avoidance symptoms) was used for the main analyses.
Brief Symptom Inventory (BSI); the general symptoms index (GSI) (mean of the 53 symptoms) was used for the main analyses.
Problems with driving. Patients were asked whether they found road travel as a driver and as a passenger less enjoyable than before the accident, and their answers were rated on a scale from “no” (0) to “yes, greatly” (3).
Pain. Patients assessed whether they still suffered pain from their accident injuries on a 4-point scale from “no pain” (0) to “severe pain” (3).
Physical problems. Patients rated how well they had recovered physically from the injuries on a 3-point scale from “back to normal, fully recovered” (0) to “major problems” (2).
Interference with everyday functioning. Patients rated the effect of the accident on their everyday life on a 4-point scale from “not affected” (0) to “greatly” (3).
Financial problems. Patients were rated on a scale from 0 (“not affected”) to 3 (“greatly”).
Insurance problems. Patients were rated on a scale from 0 (“not affected”) to 3 (“greatly”).
Intervention
Subjects in the intervention group were offered a debriefing intervention which lasted approximately one hour. It included a detailed review of the accident, the encouragement of appropriate emotional expression, and initial cognitive appraisal of traumatic experience: that is, an appraisal of the subject’s perceptions of the accident. The aim of the intervention was to promote the emotional and cognitive processes which, it is believed, lead to resolution of the trauma. The intervention ended with the research worker giving information about common emotional reactions to traumatic experience, stressing the value of talking about the experience rather than suppressing thoughts and feelings, and also the importance of an early and graded return to normal travel. Subjects were given a leaflet summarising the principles of the intervention and which also encouraged support from family and friends; it advised consultation with the family doctor if problems persisted. General practitioners were informed of the study and sent a copy of the leaflet.
Statistical analyses
Scores on the IES and BSI were not normally distributed. They were log-transformed, which normalised the distributions. Changes in these scores over time were analysed with repeated measures analysis of variance (ANOVA). Differences between the intervention and control groups were tested using analysis of covariance (ANCOVA), with baseline scores as the covariates.
To investigate whether there were differential effects of the intervention, depending on the initial severity of intrusion and avoidance symptoms, patients were classified as to whether they had low (<24) or high (≥24) initial IES scores. This cut-off point was chosen because it represented the top 25% of the initial IES scores. Group differences were analysed with 2-way ANCOVA, using baseline IES scores as the covariate, and intervention v. control and high v. low initial score as the between-subject factors.
Ratings for loss of enjoyment when driving or being a passenger, pain, physical problems, and interference with everyday functioning at 3 years were analysed with t tests. ANCOVAs were used to control for the possible effects of injury severity on the outcome measures. Ratings for financial and insurance problems were analysed with Mann-Whitney U-tests, because of very skewed distributions. Driving behaviour and driving problems were analysed with χ2-tests.
Results
Of the 106 patients who had originally participated in the intervention study, 61 patients (30 from the intervention group and 31 controls) were assessed at 3 years post-intervention. This proportion was similar to that in other studies of road accident victims and in part reflects the high mobility of road accident victims, who are mostly young and frequently appear not to receive questionnaires sent to their original addresses. Patients who responded to the 3-year follow-up did not differ from those who did not respond in terms of initial symptom severity (scores on the IES and on the BSI), age, gender, marital status, social class, driver v. passenger, vehicle type, length of hospital stay, history of emotional problems and initial emotional response to the accident. However, follow-up participants had been more severely injured (mean severity 1.85 v. 1.58, t(104)=2.13, P=0.035).
There were no significant differences between follow-up patients who had received the debriefing intervention and controls in terms of age, gender, marital status, social class, driver v. passenger, vehicle type, length of hospital stay, severity of injury, history of emotional problems and initial emotional response to the accident. However, when types of injury were considered separately, it was found that the intervention group had more severe injuries of their extremities (mean severity 1.33 v. 0.71, t(59)=2.22, P=0.030). There was no difference between intervention (27%) and control groups (29%) in the proportion of patients classified as having high initial scores (χ2(1,61)=0.42, P=0.84).
Post-traumatic symptoms at 3 years
Intrusion and avoidance symptoms as measured by the IES were lower at the 3-year follow-up than at initial assessment: F(1,59)=6.33, P=0.015. The ANCOVA did not show a significant effect of intervention on IES scores at 3 years: F(1,58)=2.03, P=0.16.
Outcome according to initial IES scores
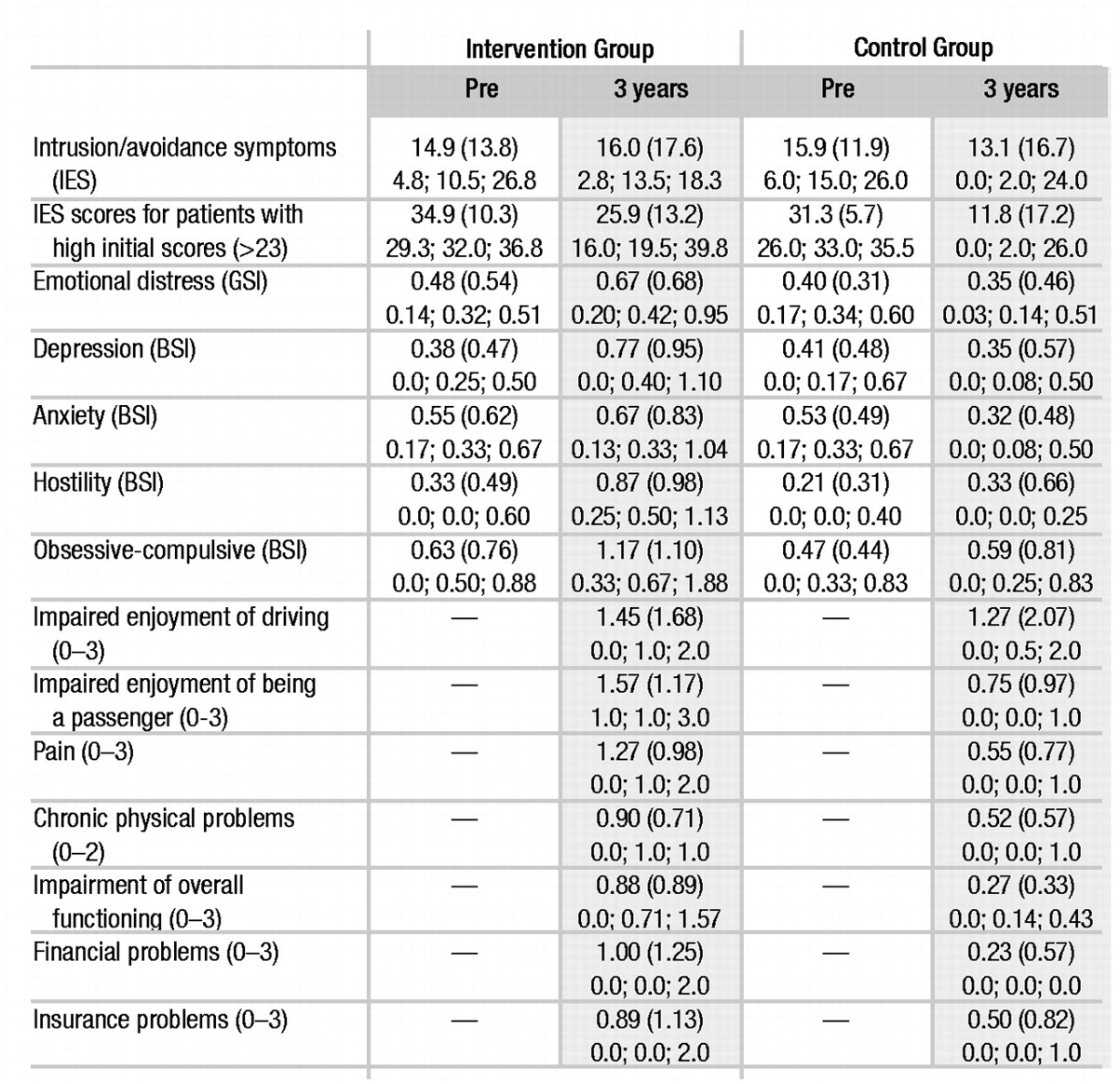
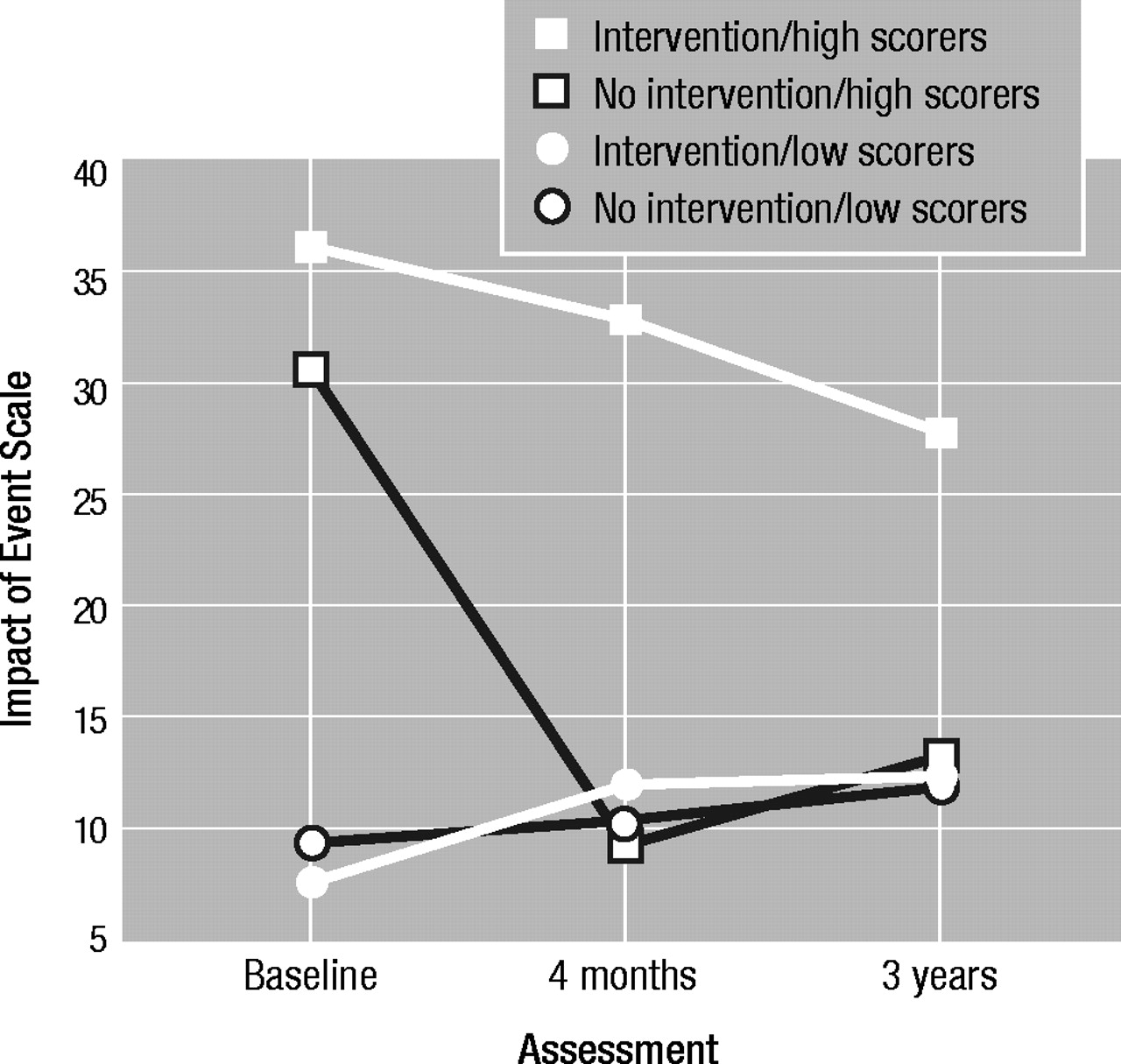
We then examined the possibility of differential effects of the intervention on patients with high and low initial IES scores (see Table 1 and Fig. 1). The ANCOVA of IES scores at 3 years showed a significant effect of intervention: F(1,56)=4.91, P=0.031; and a significant interaction of intervention and IES group (high v. low initial scores): F(1,56)=4.29, P=0.043. For those with low initial scores, there were no differences between intervention and control patients, but the intervention group had a significantly worse outcome among those who had high initial scores (t(14)=2.56, P=0.023; observed difference 0.74, 95% CI for difference 0.11–1.28). Patients with high scores who received the intervention still showed symptoms, whereas those who did not receive the intervention improved and had scores comparable with those of patients with low initial scores at follow-up.
In order to examine the course of the worse outcome of treated patients with high initial IES scores, outcome at 4 months was included in a further ANCOVA (Fig. 1). The results again showed an effect of intervention (F(1,52)=7.32, P=0.009) and an interaction between intervention and IES group (F(1,52)=5.46, P=0.023). The results indicated that the negative effects of the intervention on patients with high initial IES scores were already present at 4 months post-intervention and were maintained at follow-up.
We next tested whether the worse outcome at 3 years of the high IES scorers who had received the intervention was due to differences in the severity of their injuries. Intervention patients with high initial IES scores had more severe injuries (2.0 v. 1.2, t(15)=3.29, P=0.005) and stayed marginally longer in hospital (2.2 v. 1.4, t(15)=l.80, P=0.092). When the injury severity for different body parts was considered separately, it emerged that the intervention group had more severe injuries to their extremities (1.6 v. 0.3, t(15)=2.99, P=0.009). Analyses of covariance tested whether any of these variables could account for the higher IES scores of the intervention group at 3 years. This was not the case. In all instances, the intervention factor remained at least marginally significant (all P<0.07).
There was a marginal association between overall injury severity and IES scores at 3 years (r=0.23, P=0.076), but no significant associations with hospital stay (r=0.20) or severity of injuries to the extremities (r=0.18).
Other psychological outcomes
Other psychiatric symptoms
Table 1 shows the results of the GSI score of the BSI. In contrast to the IES results, there was no overall improvement from the initial assessment to the 3-year follow-up on this measure (P>0.40). The ANCOVA of 3-year follow-up scores, controlling for baseline scores, showed a significant effect of intervention (F(1,57)=5.21, P=0.026). Patients in the intervention group reported more severe psychiatric symptoms at follow-up (observed difference 0.08; 95% CI for difference 0.009–0.15).
The difference between the groups at 3 years remained at least marginally significant when the severity of injury of the extremities, overall injury severity or hospital stay were statistically controlled by ANCOVA (all P<0.07). When the sub-scales of the BSI were considered separately, the intervention group had significantly higher scores (P<0.03) at 3 years for anxiety, depression, obsessive-compulsive problems, and hostility.
Travel anxiety
There were no differences between the groups in driving behaviour: one patient in each group had given up driving as a result of the accident. The groups did not differ in terms of enjoyment of driving (t(57)=0.37). However, people in the intervention group enjoyed being a passenger less than those in the control group (t(54)=2.87, P=0.006; observed difference 0.82, 95% CI for difference 0.25–1.40).
Other outcomes
Pain
At the 3-year follow-up, those in the intervention group reported more severe pain (t(59)=3.19, P=0.002, observed difference=0. 72, 95% CI for difference 0.27–1.17) (see Table 1). The effects were the same when mean severity of injury, length of hospital stay, or injuries of extremities were controlled in analyses of covariance (all P<0.007). Whether or not a patient had high initial IES scores did not have any effect on pain at 3 years.
Physical problems
At the 3-year follow-up, patients in the intervention group reported having recovered less well physically than controls (t(59)=2.33, P=0.023, observed difference=0.38, 95% CI for difference 0.05–0.71). Of the intervention group, 20% described major chronic health problems, compared with 3.2% of the control group. The difference between the groups was only partially accounted for by differences in severity of injury, because the worse outcome for the intervention subjects remained marginally significant in analyses of covariance controlling for mean injury severity, length of hospital stay, or injuries of extremities (all P<0.07). Whether or not a patient had high initial IES scores did not have any effect on the degree of physical recovery at 3 years.
Quality of everyday life
On the overall score, patients in the intervention group reported more impaired functioning than controls (t(54)=3.48, P=0.001; observed difference=0.61, 95% CI for difference 0.26–0.97). The group difference remained highly significant when severity of injury to the extremities, overall injury severity, or length of hospital stay were statistically controlled for with analysis of covariance (all P<0.008). When scores on the individual ratings were considered, significant group differences were found for home maintenance, leisure, friends, work and hours worked.
The intervention group described greater financial problems as a result of the accident, U=279.5, Z=2.67, P=0.008. There was no effect of insurance problems on everyday life between the groups.
Discussion
There are some methodological limitations to our study. There were baseline differences in injury severity and length of hospital stay in the initial sample. Follow-up was incomplete, but it is reassuring that the characteristics of responders and non-responders were similar. For patients who participated in the follow-up, there was no significant group difference in overall injury severity, but the intervention group had more severe injuries to their extremities. However, group differences in the outcome measures at 3 years held up when overall injury severity or severity of injuries to the extremities were statistically controlled by analysis of covariance.
Our debriefing intervention was carried out with individuals who were unprepared for highly stressful experiences, was relatively short and had limited internal structure. It contrasted in significant ways with the models of psychological debriefing described by Mitchell (
Mitchell, 1983) and Dyregrov (
Dyregrov, 1989), both of which were devised for groups of emergency services and rescue personnel, are substantially longer (2–3 hours minimum) and are conducted in a highly structured manner.
Outcomes
The first aim was to determine whether we could replicate at 3 years our previously published report of outcome at 4 months. The findings strongly support our earlier conclusion, that a 1-hour debriefing intervention and written information had no benefit for a range of psychological and social outcomes, and reinforce the conclusion that the intervention may have made patients worse. We are now able to report a follow-up considerably longer than is available for any other published randomised controlled trial. The conclusions are in agreement with those of the Cochrane Review (
Wessely et al., 1998) and in particular with the findings of the only other long-term follow-up, which reported outcome at 13 months following acute burn injury (
Bisson et al., 1997).
Our second aim was to examine the differential effects of intervention on those with high and low initial IES scores. For patients with low IES scores, it does not seem to make any difference whether or not they receive intervention; but for patients with high scores, post-traumatic stress disorder (PTSD) symptom outcome is significantly worse if they receive the intervention.
Our other aim related to outcomes other than PTSD. It is apparent that there is an adverse outcome in the intervention group for emotional distress, subjective report of physical symptoms and physical functioning for pain, and for ratings of the main domains of everyday life. Although most of the measures were simple rating scales, the effect sizes appear to be of clinical significance.
Mechanisms
The mechanisms of the adverse effects are unclear. One may speculate that very early exposure to the memory of the traumatic event is counter-productive in that it may interfere with the normal cognitive processes that lead to recovery. It is possible that the instructions led patients to ruminate excessively about the accident rather than putting it behind them. It is also possible that the process and recommended content of debriefing have effects on psychological processing very different from those of the cognitive interventions which have so far been used with apparent benefit at a somewhat later stage after trauma. The adverse effects of the intervention may not apply to other forms of debriefing involving later intervention or group debriefing. However, it is difficult to see how group debriefing could be applied to sufferers from road traffic accidents who experience different types of accident at different times. Furthermore, as yet there is no empirical evidence that group debriefing has positive effects on later PTSD or other symptoms.
Clinical implications
Our results strengthen the conclusions of the Cochrane Review (
Wessely et al., 1998). Those who are most at risk of persistent PTSD and other poor outcomes are unlikely to be helped by a short 1-hour intervention following widely accepted debriefing principles. Indeed, our findings strengthen the argument that such interventions are harmful.
We do not conclude, however, that those who are distressed should be denied immediate support and practical help; nor do we oppose efforts to increase recognition of significant problems in the early weeks and months after major trauma. There is also encouraging evidence that psychological treatments involving cognitive restructuring and other elements can be highly effective. We suggest immediate support and practical help, together with follow-up, to identify those with persistent problems who may benefit from extra help. Such help should be proven cognitive restructuring and behavioural techniques provided in an individualised and flexible manner.