Anorexia nervosa is a condition arising most commonly in adolescence, with the highest at-risk group being women between 15 and 22 years. The seriousness of the illness is attested to by long-term follow-up studies, which show high levels of long-term morbidity and a significant mortality (
Deter & Herzog, 1994;
Eckert, Halmi, Marchi, Grove, & Crosby, 1995;
Nielsen et al., 1998; Ratnasuryia, Eisler, Szmukler, & Russell, 1991). There is evidence that the illness has a relatively favourable prognosis where onset is during adolescence and the duration is fairly short (
Morgan & Russell, 1975).
Strober, Freeman, and Morrell (1997) have shown, however, that although most adolescents suffering from anorexia nervosa recover fully, the illness tends to be protracted, lasting 5–6 years on average at a crucial time in a young person’s development. Less severe cases reported from primary care (
Graham, Senior, Lazarus, Mayer, & Asen, 1992;
Mayer, 1994) seem to follow a more benign course.
There are numerous reports of various psychological and physical treatments for anorexia nervosa, although few have been systematically evaluated. The conclusions that can be drawn from the existing studies are further limited by the lack of differentiation between age-specific groups, who might be expected to respond differently to different treatments.
The first accounts of treatment of anorexia nervosa in adolescents were from inpatient treatment programmes (e.g.
Warren, 1968) and it is clear that even today there is a strong tendency to see anorexia nervosa as a dangerous condition requiring admission to hospital unless the patient responds quickly to outpatient treatment. Follow-up studies of adolescent cohorts from inpatient units, however, provide inconsistent evidence about the efficacy of such treatments (
Herpertz-Dahlmann, Wewetzer, Schultz, & Remschmidt, 1996;
Jarman, Rickard, & Hudson, 1991;
Steinhausen & Seidel, 1993;
Strober et al., 1997).
A number of follow-up studies of adolescents with a relatively short history of anorexia nervosa have shown positive response to family therapy (
Dare, 1983;
Herscovici & Bay, 1996;
Martin, 1985;
Minuchin et al., 1975;
Minuchin, Rosman, & Baker, 1978). The reports of Minuchin and colleagues from the Philadelphia Child Guidance Clinic, which combined a well-developed theoretical model of the “psychosomatic family” with a clear account of a particular family therapy approach, have been particularly influential.
To date there have been three controlled treatment studies for adolescent anorexia nervosa involving family therapy. The first compared family therapy with individual supportive therapy as a follow-up to inpatient treatment (
Dare, Eisler, Russell, & Szmukler, 1990;
Russell, Szmukler, Dare, & Eisler, 1987). This study included a predefined subgroup of adolescent anorexic patients (with an onset before the age of 18 and a history of illness of under 3 years) for whom family therapy was significantly more effective as a follow-up treatment than individual therapy. A long-term follow-up has shown that differences between treatment remain evident even after 5 years, with those who had received family therapy continuing to do well while those who had received individual therapy having mostly improved but being less likely to have made a full recovery (
Eisler et al., 1997).
Robin, Siegel, Koepke, Moye, and Tice (1994) compared behavioural family systems therapy (BFST) and ego orientated individual therapy (EOIT). Both therapies were effective with relatively little difference at 1-year follow-up although the family intervention resulted in significantly greater weight gain and greater change in maternal positive and negative communication. The relatively small differences between the two treatments found in this study are of interest when compared with the
Russell et al. (1987) work. Although the two studies are not directly comparable, it is worth noting that the protocol of the latter study specifically excluded the parents from contact with the therapist undertaking the individual supportive treatment and access to any other member of the treatment programme was avoided as much as possible. The comparison individual therapy (EOIT) reported by
Robin et al., (1994) consisted of weekly therapy for the adolescent but also included a 3-weekly support meeting for the parents of the patient.
Le Grange, Eisler, Dare, and Russell (1992b) reported a study in which 18 adolescents with eating disorder were randomly assigned to two forms of family intervention: (1) whole family therapy, drawing on the models of Minuchin (
Minuchin et al., 1978) and
Palazzoli (1974), and (2) a separated family intervention that offered support to the patient and guidance to the parents. The end of treatment effects of the two interventions were similar, although an exploratory analysis of the data suggested that high levels of maternal criticism of the patient were associated with a poor outcome and that this effect was stronger in the whole family therapy group than in the separated family therapy. The differential effect of maternal criticism in the two treatments suggested that there might be different processes involved in the outcome of therapy in these forms of family intervention.
The study reported in this paper is an extension of the above study. The two forms of family intervention, conjoint family therapy (CFT) and separated family therapy (SFT), are later versions of the therapies termed “family therapy” and “family counselling” by Le Grange et al. In this paper the main focus are the end-of-treatment results.
Methodology
The study took the form of a randomised controlled trial (RCT) of two forms of family therapy. Both forms of treatment were provided by the same therapists and the distinctiveness of the therapies was ensured by separate, “live” supervision provided by different supervisors (CD & GR). The treatments were 1 year in duration and were conducted on an outpatient basis, although where there was a serious clinical need patients were admitted to an inpatient Eating Disorder Unit. Previous research had demonstrated that engagement in treatment and treatment progress was related to the level of parental criticism (
Le Grange, Eisler, Dare, & Hodes, 1992a;
Szmukler, Eisler, Russell, & Dare, 1985). The treatment allocation was, therefore, stratified on the basis of the number of parental critical comments to the patient (using two or more critical comments made by either parent as the threshold).
Assessments were conducted by a research psychiatrist (MH) who was independent of the treatment team and interviewed the patient and her family and administered the self-report questionnaires. A similar assessment was carried out at 3 months (T2), 6 months (T3), and at 12 months (T4) to allow for the evaluation of the process of change over the course of the treatment (the details of which will be presented in a further paper). The research assessments (including the “end-of-treatment” T4 assessment) were carried out on all subjects regardless of whether they completed the planned 12-month course of treatment.
Subjects
The patients were from a consecutive series of referrals of adolescents to the Eating Disorder Services of a Postgraduate Psychiatric Teaching Hospital in London (the Maudsley). Of the 57 referrals, 14 did not reach DSM-IV or ICD-10 criteria for anorexia nervosa at assessment (10 of these subjects met diagnostic criteria for bulimia nervosa; their characteristics and treatment are described elsewhere—
Dodge, Hodes, Eisler, & Dare, 1995). A further three refused participation when asked to give informed consent to take part in the study. Thus a total of 40 patients were entered into the study.
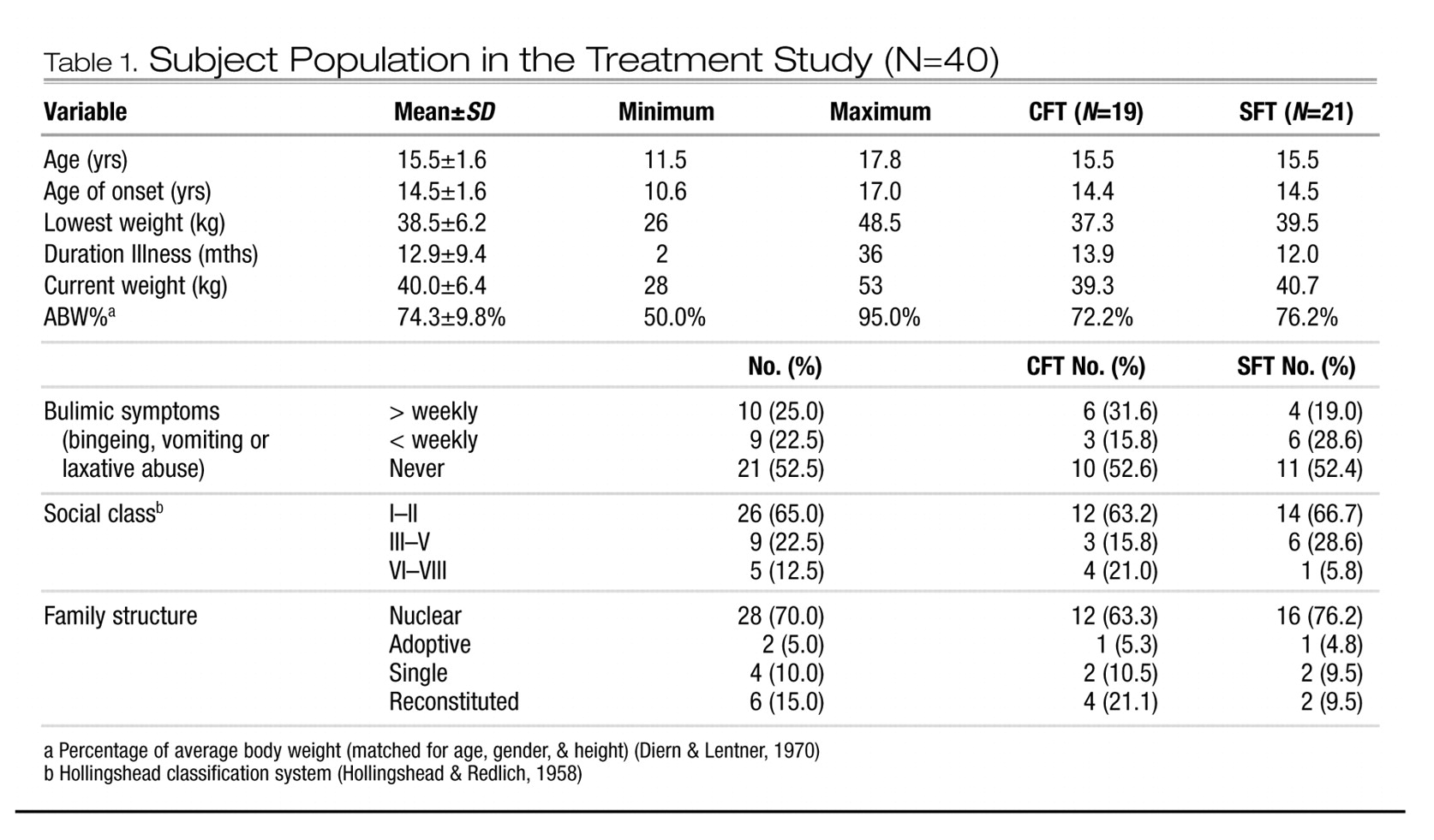
Table 1 shows the basic anamnestic data broken down by the two treatment groups. The patients were on average 15½ years old and had been ill on average for approximately 1 year at the time of admission to the study, although the duration of the illness varied considerably (2–36 months). All but one were female. Most of them were severely underweight (on average 25% below their expected weight) and nearly two thirds had had previous treatment for anorexia nervosa (17 inpatient, 7 outpatient). Twenty-five per cent of the patients were inducing vomiting and/or bingeing (and in some cases also abusing laxatives) at least once a week. Approximately two thirds were from social classes I and II (classified by father’s occupation) and nearly three quarters of the subjects came from intact nuclear families. There were no statistically significant differences on any of the demographic variables between the two treatment groups.
Individual assessment measures
The patients completed a number of questionnaires assessing mood (Short Mood and Feeling Questionnaire—SMFQ;
Angold, Costello, Messer, & Pickles, 1995), self-esteem (Rosenberg Self Esteem Inventory—RSE;
Rosenberg, 1965), and obsessional phenomena (Maudsley Obsessional Compulsive Index—MOCI;
Hodgson & Rachman, 1977), as well as two inventories tapping aspects of eating disturbance (Eating Attitude Test—EAT;
Garner & Garfinkel, 1979; Eating Disorder Inventory—EDI;
Garner, Olmstead, & Polivy, 1983).
A semistructured interview was used to obtain details of the history and clinical manifestations of the illness as well as the psychosocial functioning of the adolescent. The
Morgan and Russell (1975) Scales (M-R Scales) were used to rate these interviews on the adolescents’ Nutritional Status, Menstrual Functioning, Mental State, Psycho-Sexual Adjustment, and Socio Economic Status. The average of these five scales was used as an Average Outcome Score (rated 0–12, with 12 indicating normal functioning). In addition to these scales, an analogous rating was made to score for the presence of bingeing, vomiting, laxative abuse, depression, obsessional symptoms, and psychosomatic tension. At the end of treatment each patient’s overall outcome was also categorised using the classification devised by
Morgan and Russell (1975): (1) A
good outcome classification is used for patients whose weight is within 15% of average body weight (ABW), in whom menstruation has returned and there is no evidence of the advent of bulimic pathology. (2) An
intermediate outcome is the same as a good outcome but without the return of menstruation. If any bulimic symptoms are present they are at a frequency of less than once per week. (3) A
poor outcome categorisation is used for patients whose weight is below 85% ABW, or who are bingeing and/or vomiting with a frequency of once a week or more. We report weight and changes in weight both as actual weight in kilograms and as a percentage of ABW (% ABW). We also report the more customarily used body mass index (BMI) for ease of comparison with other studies, although for adolescents this is a less appropriate measure of change as it does not correct for age and sex.
Family measures
All family members completed the Family Adaptability and Cohesion Evaluation Scales (FACES III ;
Olson, Sprenkle, & Russell, 1979), which is used to assess perception of closeness and rigidity. The questionnaire is completed in two versions (“perceived” and “ideal”) ; the comparison of the two versions provides a measure of family dissatisfaction. These results are not presented in detail here but will be reported in a further paper.
Each family was interviewed using the Standardised Clinical Family Interview (SCFI;
Kinston & Loader 1984), which was used for rating the Expressed Emotion (EE) measure (
Leff & Vaughn, 1985) from both parents to the patient and sibling and that between the parents. The use of a family interview for the ratings of EE was validated in 17 families against the customary Camberwell Family Interview (an interview with a single person) (see
Hodes, Dare, Dodge, & Eisler, 1999).
The treatments
As in the two treatments compared in the study by
Le Grange et al. (1992b), the CFT and SFT contain many similar features. These include: (1) stressing that the family is not seen as the cause of the illness but more as a resource for helping the adolescent to overcome her problems; (2) the provision of detailed information about the psychological effects of starvation; (3) an emphasis on the compulsive quality of anorexic behaviours, which take the symptoms outside the patient’s self-control; (4) the need for re-feeding to be parent-directed without criticising or blaming the patient; (5) the offering of information about the need for support for the adolescent to take back control of her life as soon as possible; (6) support for the two parents (in families within which there is a couple) to show the teenager that the parents have a life together beyond shared care of children.
Both forms of therapy begin with an emphasis on the parents taking control of re-nutrition, with a gradual move towards conversations exploring more general implications of adolescence for children and parents as soon as the nutrition level is safe. The aim is to help the family to disentangle individual psychological issues (e.g. self-esteem, individuation, psychosocial functioning) and family relationship issues from the eating disorder behaviour and the interactional patterns that have developed around it. The way in which these general therapeutic principles are applied in practice, of course, varies from family to family.
The frequency of sessions was dictated by clinical need and was similar in both treatments. Generally, families were seen weekly during the early stages of treatment, with the gaps between sessions gradually increasing to 3–4 weeks (mean number of sessions=16.4 ± 8.9 for CFT and 15.5±6.8 for SFT). In SFT the same therapist saw both the adolescent and the parents. The order of the individual and parental sessions was not prescribed and was left to the therapist to agree with the family as seemed most useful. CFT sessions lasted an hour; in SFT the individual and parental sessions each lasted 45 minutes.
SFT1.
The specific features of SFT are governed by seeing the parents and patient separately. The therapist and the parents discuss strategies for achieving nutritional change in their child, but without the opportunity for the therapist to intervene directly in the process of interaction between parents and child. The parents are actively supported in a warm, personal way by the therapist, who encourages them to discuss the possibility of taking a firm stance around eating whilst emphasising the need for the avoidance of blame. The discussion of marital or relationship problems is not fostered except insofar as it is needed to support the development of a strong interparental alliance in the task of re-feeding.
The adolescent is seen individually for supportive counselling, the content of which is determined by the adolescent’s capacity to engage in a discussion of the experience of anorexia and the confrontations arising from the anxiety and opposition of other family members, especially the parents. Discussion of the way in which the symptoms become the focus of the relationships in the family and the way these might change under the impact of the therapy is also a regular topic. With younger adolescents, who may be reluctant to engage in individual work, sessions sometimes appear to lack continuity and may be limited to issues directly related to the eating problems. However, with older patients an effective therapeutic alliance often evolves allowing important aspects of the patient’s feelings about herself, her friendships, her ambitions, and her relationship with the family to be discussed.
CFT.
In CFT the initial sessions are taken up with engaging the whole family accompanied by a careful monitoring and often an augmenting of the anxiety of the family around the anorexia in a warm, nonblaming manner. The therapist spends a lot of time ensuring that each family member present has the opportunity for her or his voice to be heard and talk between parents and children is continually cultivated. The treatment contains two essentially paradoxical characteristics: (1) the therapist openly talks of the dangers of the self-starvation and implies that the parents might take forceful steps to re-feed their daughter whilst (2) encouraging the daughter to assert her right to be in control of her own way of life and personal ambition. The anorexia is often personified as “an enemy within” who deceives the patient into thinking that the anorexia is her own authentic voice whilst reducing her to a cypher, governed by the psychology of starvation.
The parents are helped to develop a method of improving their daughter’s nutrition using their existing repertoire of parenting capabilities. The therapist looks for evidence of positive coping strategies in the unravelling account of family life and within the family interactions as observed during therapy sessions. The CFT is characterised by a considerable amount of deliberation concerning the patterns of life in the families in which the parents grew up, during which discussions the therapist disavows the pursuit of pathology and stresses the wish to understand the family strengths and traditions as well as the habitual patterns of family organisation, especially around growing up and leaving home. The therapy moves towards endorsing the process of parents and the children finding joint and separate individualised life styles.
Statistical procedures
Continuous data was analysed using ANOVA and ANCOVA procedures whereas categorical data was processed by means of the Fisher Exact test. An α of .05 was decided upon as the level of probability of statistical significance
2. Effect sizes for change were calculated by dividing the score differences between T1 and T4 by the
SD of the difference (giving a standardised
z score allowing a comparison between different measures of change—it should not be thought of as a direct measure of the effectiveness of the treatment as it does not compare the change brought about by treatment with spontaneous change). The statistical programme, from StatSoft Inc. (1997), was STATISTICA for Windows running on a PC. The results comparing the two therapies are reported on an intention to treat basis, that is, regardless of whether or not the patient continued for the whole course of treatment that was offered.
Results
Engagement in treatment and follow-up
Of the 40 patients enrolled in the study, 36 either completed a full year of treatment (29 subjects with a mean number of sessions=18.9 ± 6.5) or at least continued for a significant period of time (defined in this study as a minimum of 3 months) (7 subjects with a mean number of sessions=12.0±4.4). Only four subjects dropped out within the first 3 months of treatment (mean number of sessions=3.3±4.4). The number of dropouts was the same in both treatments. The end-of-treatment follow-up was complete for all patients insofar as the patients’ symptomatic status was concerned, although some patients did not complete all of the questionnaires and similarly some families did not attend the follow-up interview, hence ratings of EE could not be completed for all families. This will appear in the report of statistics by the size of N for particular measures.
Overall response to treatment
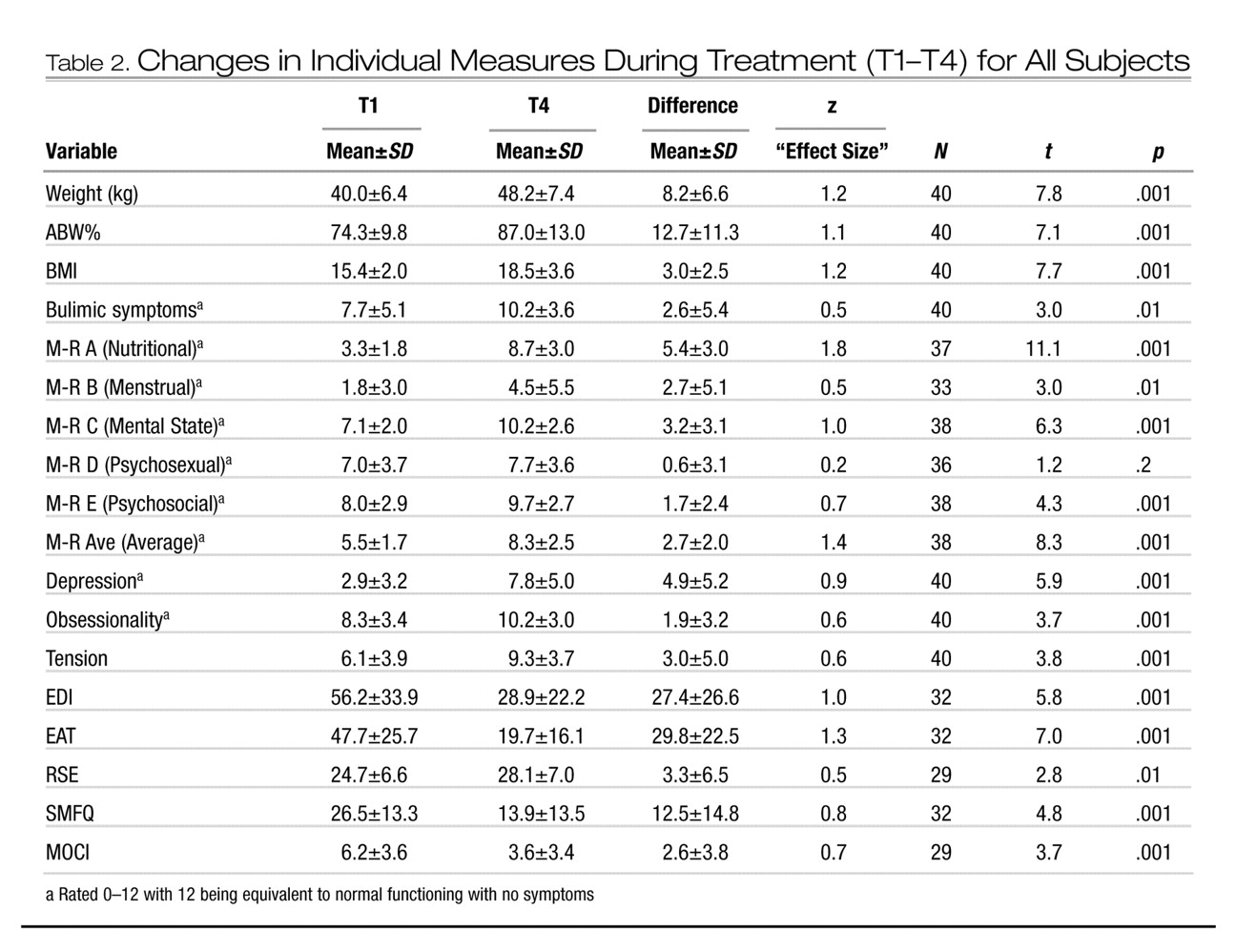
Table 2 shows the changes between T1 and T4 for the group of patients as a whole. All measures show significant improvements except for one: the M-R Psychosexual Scale. The changes in weight (an average of 12.7 ± 11.3%), and the gains on the M-R Nutritional Scale (5.4±3.0) reflect the striking improvement in nutrition of the patient group as a whole. Changes in menstrual functioning are at a relatively low level, as reflected in the modest (though statistically significant) improvement in the M-R B scale (2.67±5.07). Forty-four per cent of the patients (excluding the prepubertal and the one male) were menstruating at the end of treatment. (The male patient had a good outcome and of the three pre-pubertal children who had not reached the menarche, one had a poor outcome and two were doing well in all respects.) The modest changes in the mean menstrual score on the M-R evaluation is parallelled by the relative lack of overall change on the Psychosexual Scale. In terms of the categorised outcome classification, 15 (37.5% ) had a good outcome, 10 (25% ) intermediate, and 15 (37.5% ) a poor outcome.
Of the 10 patients who had significant bulimic symptoms at T1, 2 remained unchanged and 8 improved. One additional patient, who had been a pure restricter at T1, started inducing vomiting on a regular basis. There were marked differences between T1 and T4 in the questionnaire measures of eating pathology (EAT 29.8 ± 22.5; EDI 27.4±26.6) and of mood (SMFQ 12.5±14.8). Self-esteem and obsessional questionnaire changes showed statistically significant improvements but with modest effect sizes (RSE 3.3±6.5; MOCI 2.6±3.8). The M-R Scale ratings of Mental State showed a clear improvement (M-RC3.2±3.1), as did the changes in the clinical rating of depression (4.9±5.2), which improvements parallel the questionnaire measures. The cumulative score of the M-R evaluation of outcome shows a clear improvement for the whole group of cases (M-R Ave 2.7±2.0).
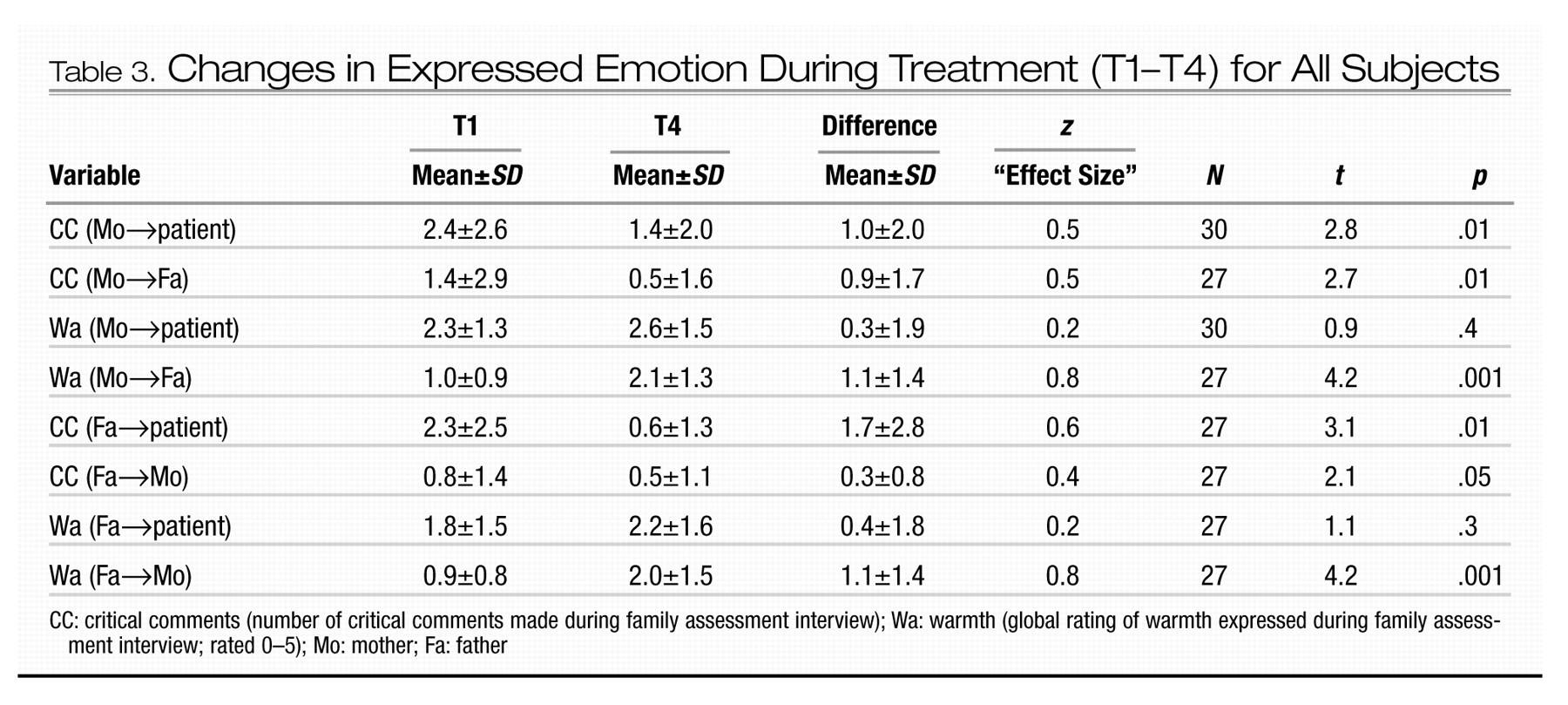
Table 3 shows changes in ratings of EE over the course of treatment. There were significant reductions in the levels of criticism from the parents to the adolescent as well as between parents. The parents were also warmer to one another at the end of treatment than they had been previously, although ratings of warmth from the parents to the adolescent did not improve significantly. On the FACES questionnaire there were changes on the Cohesion Scale, showing that family members rated themselves as being less close at the end of treatment than at the initial assessment (mean family Cohesion [Perceived] score
3: T1=37.5 ± 5.0; T4=33.4±5.5;
t=5.3;
p<.0001). Interestingly, there were similar changes in how family members would ideally like the family to be (mean family cohesion [Ideal] score: T1=39.9 ± 3.4; T4=36.5±3.5;
t=4.7;
p<.0001). There were no significant changes on the ratings of family adaptability over the course of treatment for the group as a whole (mean family Adaptability [Perceived] score: T1=25.2 ± 4.0; T4=24.8±5.0; mean family Adaptability [Ideal] score: T1=30.7±2.6; T4=29.3±2.3).
Predictors of outcome
Compared to other treatment studies in anorexia nervosa, our sample was relatively homogenous, consisting of adolescents with a comparatively short history of illness who might be expected to have a good prognosis. However, given the high percentage of subjects who had not responded to previous attempts at treatment, we were interested to know whether there were identifiable factors that could predict response to treatment. Several variables were found to have a strong relationship to outcome: the amount and type of previous treatment for the eating disorder, the duration of the illness, the degree of weight loss at the beginning of treatment, and maternal criticism.
The clearest association was between previous treatment and outcome. Of the 16 patients who had had no previous treatment, 13 had a good or intermediate outcome whereas half of those who had been treated before had a poor outcome. At the other end of the continuum, patients who had had repeated treatment (inpatient or outpatient) generally did not do well, with 8 out of 11 having a poor outcome (no treatment vs. repeat treatment: p=.01, Fisher Exact test). There was also a clear association between the length of the illness and outcome: those who were classified as having a poor or intermediate outcome at the end of treatment had been ill for a significantly longer period than those who had a good outcome (poor 15.9 ± 9.7 months; intermediate 15.8±10.9 months; good 7.9±5.7; F=3.78, p=.03). There was also a significant difference in the degree of emaciation at the time of referral to our clinic between the three outcome groups (poor 69.5 ± 11.0 %ABW; intermediate 73.4±7.4; good 79.7±7.5; F=4.99, p=.01).
Using the M-R Average Outcome score as the outcome measure, initial maternal critical comments (using a cutoff point of 3 or more CC) predicted outcome (low CC:M-R AveT4=9.0 ± 2.7; high CC: M-R AveT4=7.3 ± 1.67; F=5.13, p=.03). There was an indication that patients with primary amenorrhoea had a worse outcome than those with secondary amenorrhoea (F=4.12, p=.002) and similarly that patients with a non-eating-disorder psychiatric history fared worse than patients without such a history (F=5.48, p=.025). However, the numbers were small (three patients with primary amenorrhoea and five with a previous psychiatric history) and these results therefore need to be treated with caution.
Comparison of outcome between CFT and SFT and the effect of EE
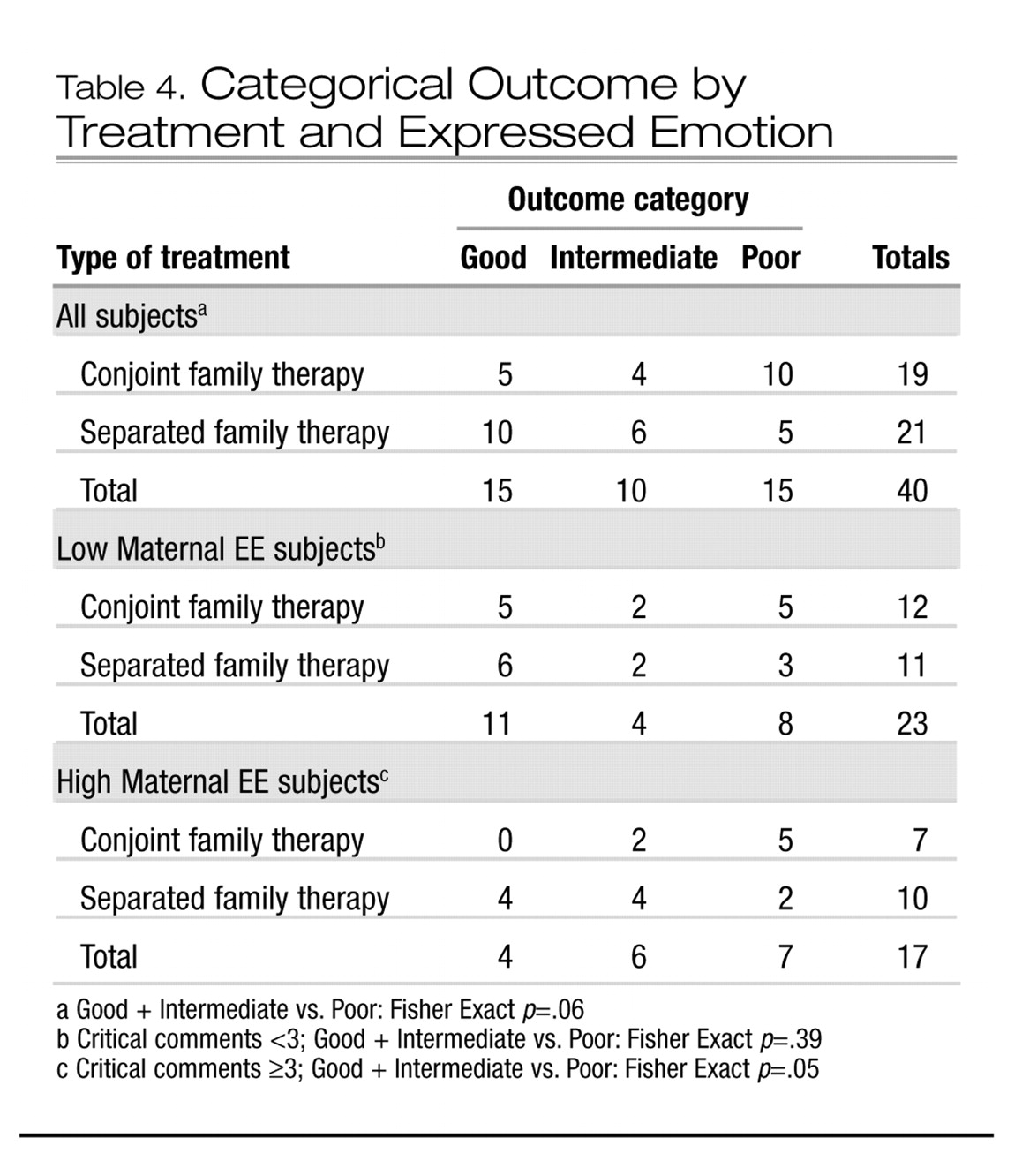
Table 4 shows the general outcome of the patients in the two treatments. Overall a smaller number of patients did well in CFT (47% good/intermediate outcome) than in SFT (76% good/intermediate), although the difference is below the level of statistical significance (Fisher Exact test, p=.06). When the patients from the high and low EE families are considered separately, a statistically significant finding emerges for the high EE cases, with 2 of 7 cases in the CFT having a good/intermediate outcome compared with 8 of 10 in the SFT group (Fisher Exact test, p=.05). For the low EE families (mothers’ CC less than 3), the results were similar in the two treatments, with 7 of 12 in CFT being in the good/intermediate group as opposed to the poor categories whereas for SFT the figures are 8 of 11.
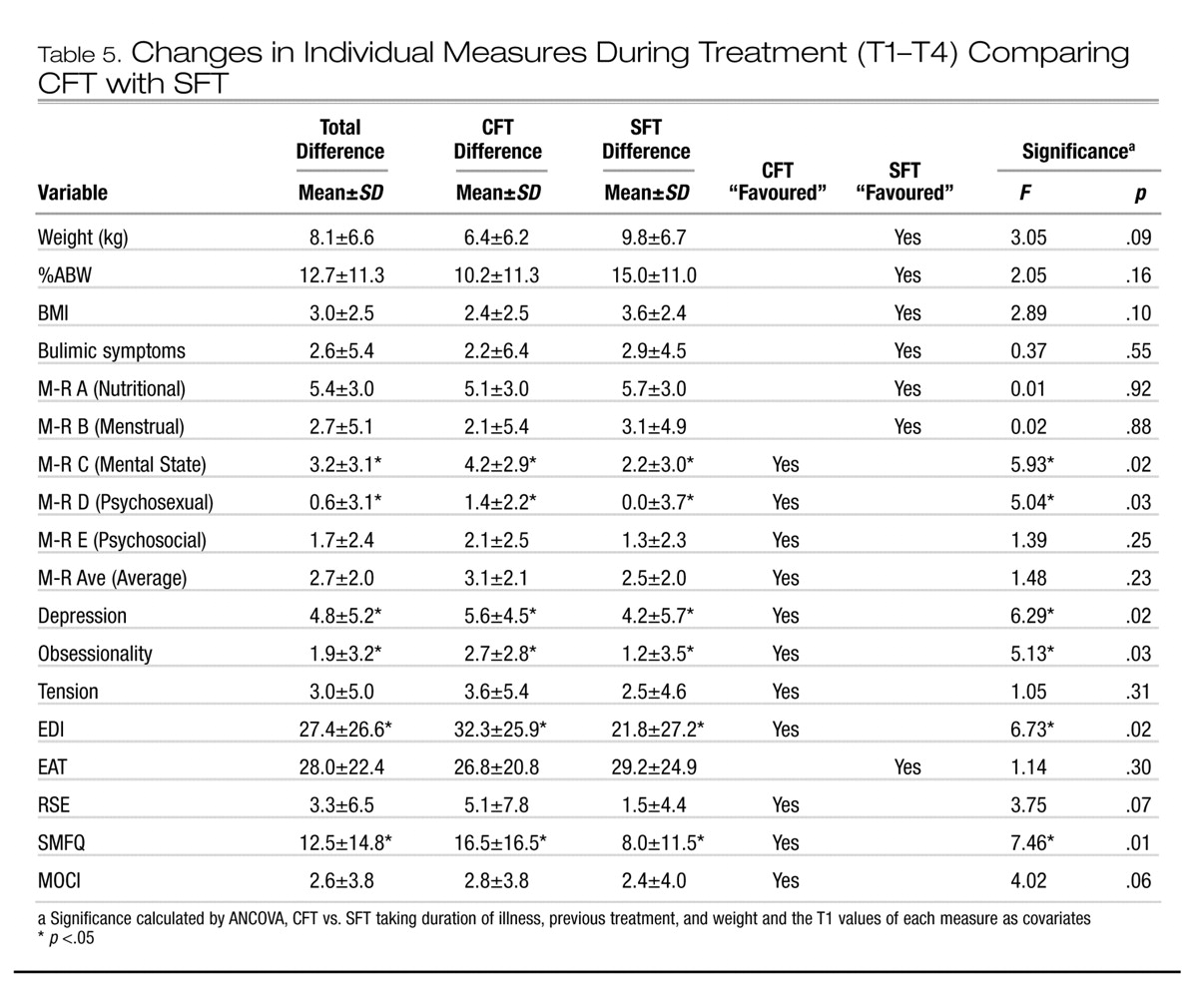
The differences between therapies on specific measures
Table 5 shows a comparison of the changes on a number of variables between the beginning (T1) and end of treatment (T4) in the group of patients as a whole and in the SFT and CFT. The differences between the end-of-treatment outcome status for the two forms of therapy is shown as favouring (that is, being more substantial) in either CFT or SFT. The statistical significance (last column) is calculated using an Analysis of Covariance for the two treatment groups at T4 using the three main predictor variables (duration of illness, previous treatment, and weight) and the T1 values of each measure as covariates.
It is apparent that only relatively few of the measures show a statistically significant difference between the two treatments. None of the variables for which SFT produces a greater improvement than CFT are statistically significant. In contrast, CFT produced more favourable results on clinical ratings of mental state, psychosexual adjustment, mood, and obsessionality and on three of the self-report measures (EDI, SMFQ, and MOCI).
The differences between treatments on the other variables are relatively small and do not reach statistical significance. Nevertheless, there is a consistency in the direction of the differences which is of interest. Broadly speaking, measures of eating disorder symptomatology (weight, nutritional status, menstrual functioning, bingeing and vomiting, EAT questionnaire) improved more in SFT than in CFT. Thus the patients in SFT gained on average 15% body weight (taking them to over 90% ABW) as opposed to 10% for those in CFT (who did not quite reach 85% ABW on average). Similarly, the three patients who had significant bulimic symptoms at the end of treatment were all in CFT. On the other hand, measures of individual psychological and psychosocial functioning (rated both clinically and on self-report) changed more for adolescents who were seen in CFT.
Measures of family functioning generally showed little difference between the two treatments. Changes in the levels of criticism and warmth on the EE scales described earlier for the whole group were comparable in both treatments. Similarly, changes in mean family ratings of Cohesion and Adaptability on the FACES self-report measure did not differ between treatments. However, when individual family members’ ratings were considered separately one clear difference did emerge. Adolescents seen in CFT rated their families as having become more flexible over the course of the year (Adaptability [Perceived] score: T1=26.4 ± 8.0; T4=28.6±5.6) whereas those in SFT saw their families as actually becoming more rigid (Adaptability [Perceived] score: T1=25.6±2.8; T4=22.9±5.4; F=7.6, p=.01—using T1 values as covariate). These differences were not found in the questionnaire responses from mothers or fathers.
Additional treatments
In the context of a randomised treatment trial it is sometimes unavoidable that, for clinical reasons, patients are given additional treatments not planned for in the study. One patient continued in individual psychodynamic psychotherapy (arranged privately) after entering the trial. None of the other patients were offered individual psychological treatments beyond those described and none were taking psychotropic medication during the study. Four patients had to be admitted to hospital because of continuing weight loss (in one case combined with deliberate self-harm).
One patient in the SFT group, having discontinued outpatient treatment after two sessions, required admission to hospital (for 7 weeks). She received no further treatment after discharge from hospital and at follow-up had a good outcome. A further patient in this group dropped out after five sessions and also had a good outcome at follow-up. In the CFT group three patients required admission to hospital for 2½–5½ months; all three also had a significant number of family sessions (17–25) and all three had a poor outcome at follow-up. Two additional patients in the CFT group dropped out early from treatment, one after four sessions who did well at follow-up, and one after a single session who had a poor outcome.
Discussion
This study, in line with a growing number of others, shows the efficacy of family interventions in the treatment of adolescent anorexia nervosa and indicates some possible differential effects between the two comparison treatments. Overall there were significant gains both in symptoms and in individual psychological measures and in measures of family functioning across the two treatments. Nearly two thirds of patients regained weight to within a normal range without the need for admission to hospital. There were similar gains for patients with bulimic symptoms, with only two continuing to manifest significant symptoms and one additional patient developing new bulimic symptoms. The patient group as a whole also showed striking improvements in a wide range of measures of individual psychological functioning and ratings of parental EE. Changes on the FACES questionnaire suggest a move to a greater sense of independence both in how family members perceived their families and in how they wished their families to be.
The data suggest that there may be important differences in the impact of the two family treatments. There were relatively small differences between treatments in the rates of change in eating disorder symptomatology but they were consistently in the direction favouring SFT. The lack of statistical significance in comparing the individual measures of symptomatic change between the treatments should not automatically be interpreted as showing equal effectiveness. It is worth noting that the small differences found favouring SFT are consistent with those reported by us in our earlier study (
Le Grange et al., 1992b). These differences are reflected in the larger number of patients being classified as having a good or intermediate outcome in SFT and, similarly with our previous findings (
Le Grange et al., 1992a), this appeared particularly true of families where there were high levels of maternal criticism. Future research with larger samples will need to clarify these questions.
Clearer differences between treatments were found on measures of individual psychological functioning. Both the clinical ratings and self-report measures showed significantly greater gains for those in CFT in terms of mood, obsessionality, and psychosexual adjustment. Similar differences favouring CFT were found on the EDI (a detailed analysis of the EDI data is beyond the scope of this article and will be presented in a later paper). Again a degree of caution is needed in accepting these findings. The levels of significance were in the range of .05–.01 and some authors would argue that with the number of comparisons being made, a more stringent α should have been adopted to correct for the possibility of obtaining “significant” differences by chance. There are two reasons why we have not adopted this strategy. First, the measures used are not randomly selected, uncorrelated variables. Correcting the α level for the number of comparisons being made would therefore lead to a conservative estimate, increasing the likelihood of a Type II error (
Bland & Altman, 1995). Second, it is important to consider the state of knowledge in the field as a whole. There have been very few treatment trials in adolescent anorexia nervosa (all with samples sizes smaller than the current study), which makes it important not to adopt an overly conservative position and reject potentially meaningful findings. On the other hand, it also follows that our findings have to be viewed with considerable caution, which can only be set aside through further research, preferably with larger samples that will provide greater statistical power.
The differences between the treatments may seem surprising at first sight. In SFT the therapist had an opportunity to work individually with the adolescent and one might have assumed that areas of individual psychological functioning would be more readily addressed. There are a number of factors that may have contributed to the results pointing in the opposite direction. In SFT the sessions with parents would often continue to focus on eating behaviours even when the adolescent was out of the real danger zone. This is understandable, because the parents continue to worry even when the immediate physical risks are reduced and are likely to want to talk about their concerns. Although this may help the parents to continue to ensure that their daughter goes on gaining weight, it may sometimes be at the cost of other issues not being fully addressed. In contrast to this, when the whole family is seen together, the family sessions provide an opportunity for discussing the eating disorder not only in the immediate context of the way the family is organised around the eating problems but also in the context of the wider family, bringing into the discussion family beliefs and history, including sometimes those issues that have become taboo subjects. The presence of siblings also provides an opportunity to broaden the discussion to general issues about adolescent development. There may also be an indirect effect of seeing the family together in that the therapist needs to make sure that the adolescent, like other family members, has space for her voice to be heard during the family discussions. This is important, particularly as the treatment develops, for as the youngster is made to give up the option of expressing herself through eating behaviour, she often feels ever more powerless. The acknowledgement of the importance of her independent voice may in itself allow her to start addressing other important issues (during or outside of therapy sessions). Paradoxically, in SFT, because the individual sessions provide the adolescent with an opportunity to speak with the therapist about her own issues, both she and the family may feel that they do not need to discuss these issues together.
It is important to compare the findings of this study with the other controlled trials with this patient population. There are three studies that provide the most direct comparison, the
Russell et al. (1987) study, which compared family and individual therapy following inpatient treatment, the
Le Grange et al. (1992b) study, which served as a pilot for our current study (the main difference from the current study being that the treatments lasted only 6 months), and the
Robin et al. (1994) RCT comparing BFST with EOIT. There have been two other controlled treatment studies in anorexia nervosa that have included adolescent patients (
Crisp et al., 1991;
Hall & Crisp, 1987). Both studies, however, also included adult patients and the results are not reported separately for the adolescent subgroup. This makes it difficult to make meaningful comparisons with the current study.
The common finding in all four studies is that treatments that encourage parents to take charge of the adolescent’s eating are effective in bringing about both symptomatic and psychological change. Involving the parents in a way that is supportive and understanding of their daughter but that encourages them to step back from trying to influence her eating (EOIT treatment in
Robin et al., 1994) appears slightly less effective, whereas when parents are not involved in the treatment at all, the process of recovery is considerably delayed (
Eisler et al., 1997;
Russell et al., 1987). Both the current study and the
Le Grange et al., study (1992b) showed that whole family meetings with families where there are high levels of criticism can be difficult and may perhaps diminish the effectiveness of treatment. There is some evidence (
Squire-Dehouck, 1993) that this may be associated with feelings of guilt and blame being increased as a consequence of criticisms or confrontations occurring in the context of family sessions. In our clinical experience with families with high levels of criticism or overt hostility, conjoint family sessions may be more usefully applied in later stages of treatment, when the anxiety around weight and eating is no longer a central issue.
The role of individual therapy remains unclear from these studies. Although individual supportive therapy with no parental involvement leads to inferior results, seeing the adolescent on her own in combination with regular meetings with the parents appears comparable in effectiveness to conjoint family therapy. The effects of the individual intervention, however, seem fairly non-specific.
Robin et al. (1994) did not find evidence to support their hypothesis that in EOIT the main mechanism of change is through enhancing the ego strength of the adolescent. On the contrary, as in our own study, they found that changes in individual psychological functioning were, if anything, smaller than the change found in adolescents seen in conjoint family sessions. The paucity of randomised studies in this area makes it, of course, difficult to draw firm conclusions about the role of individual therapy in the treatment of adolescent anorexia nervosa, whether used on its own or in combination with family therapy. A limitation of all the above studies (including the current study) is that they have been based on relatively small samples and, in spite of the consistency of the findings, caution is needed in interpreting the results.
Conclusions
Family involvement in the clinical management of anorexia nervosa in adolescents has become standard practice, even though all too often the main thrust of treatment remains nutritional restoration in hospital and individual psychotherapy or counselling for the adolescent. Although some adolescent anorexic patients may continue to need inpatient treatment, there is growing evidence that the mobilisation of family resources may be the key to effective treatment, which can obviate the need for admission to hospital. Family therapy is an effective intervention both in managing the illness itself and in bringing about important psychological and family changes.