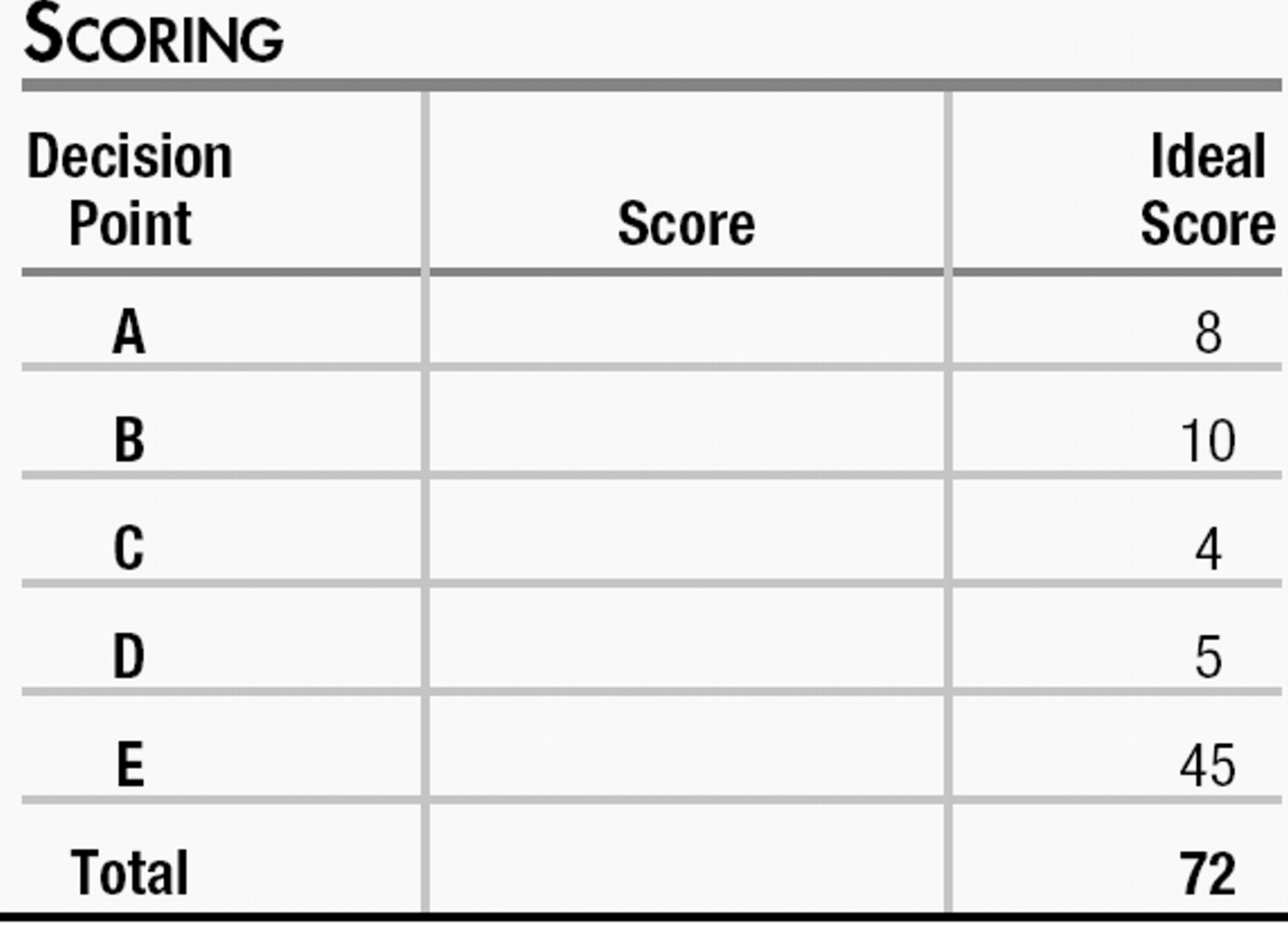
This exercise is designed to test your comprehension of material presented in this issue of FOCUS as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below, to the best of your ability, on the basis of the information provided, making your decisions as you would with a real-life patient.
Questions are presented at “decision points” that follow a section that gives information about the case. One or more choices may be correct for each question; make your choices on the basis of your clinical knowledge and the history provided. Read all of the options for each question before making any selections.
You are given points on a graded scale for the best possible answer(s), and points are deducted for answers that would result in a poor outcome or delay your arriving at the right answer. Answers that have little or no impact receive zero points. On questions that focus on differential diagnoses, bonus points are awarded if you select the most likely diagnosis as your first choice. At the end of the exercise you will add up your points to obtain a total score.
VIGNETTE PART 2
You call her around 9 p.m. that same night to ask how she is feeling. You notice immediately that she is speaking slowly with a very soft voice.
“It's gone,” she tells you. “I took a shower and listened to some music. I'm okay.” You inquire further what she meant by “it's gone.” She tells you that she was feeling helpless, hopeless, and started thinking about dying. “I know you don't know me yet, but I have been going through this…” Her words trail off; she begins to sob. You wait, and after a moment she says, “I'm so sorry. I'm really okay.” You ask if she is thinking about harming herself or killing herself to which she calmly responds, “No. I'm solid. I haven't been to the hospital for this so far and I plan to keep it that way.” She has the phone number for the local psychiatric emergency room and has called it numerous times to talk with a clinician when she starts to feel unsafe and this “always” helps her feel better. There are family members at home with her and she tells you she will not be alone. She tells you that when she feels this depressed she relieves the symptoms by taking a shower, listening to music, sitting in her backyard with a book, or writing in her journal. She also kept the worksheets she used in dialectical behavioral therapy (DBT) and sometimes reviews them, although “not like I probably should. I didn't like that therapy much. I don't freak out on people like the others I met. No distress tolerance,” she announces, as if making a joke.
You ask if something happened today or recently that might have contributed to her feeling so low. She responds, drably, “Nothing out of the ordinary.” She clears her throat and her voice seems more assured. Then you hear her yell to someone in her home, “I'm on the phone!” She then says to you, “I'll be there on Monday. Thank you for calling me, it means a lot.”
DECISION POINT B:
Given what you know about this patient so far, how should you address her risk for suicide? Points awarded for correct and incorrect answers are scaled from best (+5) to unhelpful but not harmful (0) to dangerous (−5).
| B1.___ | The patient admits that she was suicidal just hours before you spoke. She now denies feeling suicidal but you are not comfortable with her “flight to health” and instruct her to go to the local psychiatric emergency room for an evaluation. |
| B2.___ | The patient admits that she was suicidal just hours before you spoke. She now denies feeling suicidal but you are not comfortable with her “flight to health” and instruct her to meet you at the local psychiatric inpatient unit where you have admitting privileges. |
| B3.___ | The patient admits that she was suicidal just hours before you spoke. She says she spent a year doing DBT where she learned how to cope with these feelings, but that was a year ago and in the moment she forgot many of the skills she typically uses in these situations. She now denies feeling suicidal and offers a safety plan that includes calling the emergency department and having family members close by. She mentions coping skills that include taking a shower, listening to music, reading in her backyard, or writing in her journal. You have an appointment with her in 3 days' time. You conclude she is safe and tell her you look forward to meeting her on Monday. |
| B4.___ | The patient admits that she was suicidal just hours before you spoke. She says she spent a year doing DBT where she learned how to cope with these feelings, but that was a year ago and in the moment she forgot many of the skills she typically uses in these situations. She now denies feeling suicidal and offers a safety plan that includes calling the emergency department and having family members close by. She mentions coping skills that include taking a shower, listening to music, reading in her backyard, or writing in her journal. She carries a primary diagnosis of borderline personality disorder, so you conclude that a visit to the emergency room would further complicate her ability to recover by encouraging reliance upon an institution to solve her problems. You conclude she is safe and tell her you look forward to meeting her on Monday. |
| B5.___ | The patient admits that she was suicidal just hours before you spoke. She now denies feeling suicidal but you are not comfortable with her “flight to health” and instruct her to meet you at your office immediately so you can assess her for safety. |
VIGNETTE PART 3
The patient arrives for her appointment as scheduled, dressed casually in jeans and a button-down long-sleeved shirt. She averts her gaze, limply shakes your hand, and then sits with her legs folded underneath her body on the chair opposite you. Her long brown hair appears poorly kempt and is partially covering her face. You welcome her to your office and tell her you are glad she decided to come. For several minutes she does not say anything. You wait. “I hate this part,” she says at last. “Starting over with a new doctor,” she begins. “I'm sick of telling my story because no one believes me.” She reaches for a tissue from the box on the table. “I don't even know what I'm supposed to feel like anymore. All I know is that I hate this.” Her voice thickens. “I'm on 450 mg of Effexor for depression, 200 mg of Seroquel for sleep—which does not work for me, by the way—and when my last doctor wanted to put me back on Depakote I started to cry, so I… .” You are unable to understand the rest of her sentence. She blows her nose. “I'm so sorry about this. You don't know me and I'm already crying like a baby.”
You tell her that your office is a safe place for her to cry or express any emotion she feels. You remind her that everything you talk about together is confidential unless she says she wants to harm someone in which case you would be obligated to break confidentiality. She smiles and pulls her hair from her face. She is not wearing makeup, and her eyes are bloodshot from crying. You tell her you would like to get to know her better and determine how you can help. You explain that you prefer to organize the interview somewhat because the session is limited to 45 minutes, but that you will need two to three sessions to make your evaluation and that will give her a chance to see if she feels you are a good match for her.
She describes her depression as “feeling hopeless, helpless, worthless. I can't concentrate to save my life, my mind is constantly rolling over things I can't do anything about. I either eat too much or not at all, and I'm bored by things I know I should enjoy, like meeting people, going to a movie, gardening.” She shakes her head. “I can't even garden! My brother is such an idiot! I spent all this time making a little vegetable garden in the backyard and he and his burn-out friends just ran through it playing Frisbee.” She tells you that she cannot speak with anyone in her family. “My father says I'm faking everything. My mother is an alcoholic, so she's usually passed out in their bedroom. She has cancer, by the way. Even the dog hates me.” She chuckles to herself. “Even the damned dog!”
You ask when she began to feel depressed and she says, “I remember the exact moment everything changed.” She tells you she was married for 2 years but they divorced 3 years ago. She met him at the bank where she currently works as a teller. “I've been a teller for 5 years and they will not promote me, but that is another story. I think it is to keep me from getting full benefits since they know I'm sick.” She says the marriage started out “okay” and she was happy just getting out of her family's house. “Maybe that is why I married him, I don't know.” In the past she had several close girlfriends, but they have drifted apart. She has had passive suicidal ideation “off and on” for the past 3 years, but never made an attempt and says she would never have the guts to do it. She does have a history of self-injurious behavior that began at the same time, including cutting her arm with a razor and punching her thigh until she has black and blue marks. The last time she hurt herself was Friday before you spoke. “I punched myself. Then I felt better. Then I wanted to do it again so I called.”
She tells you she has been on too many medications and that “nothing works.” Her past medication trials have included fluoxetine up to 80 mg, escitalopram up to 40 mg, bupropion up to 450 mg, nortriptyline up to 150 mg, augmentation strategies with valproic acid up to 1500 mg, lithium up to 450 mg b.i.d., quetiapine up to 200 mg, risperidone up to 3 mg, lorazepam up to 2 mg, clonazepam up to 2 mg, and zolpidem up to 10 mg. She remembers being on fluoxetine for about 1.5 years and felt better for only the first 2–3 months. Then her doctor kept raising the dose. Then he augmented first with bupropion, then valproic acid, then changed the valproic acid to lithium. She changed doctors because the valproic acid caused her to put on about 40 pounds and she became sick and tremulous on the lithium, so that was discontinued. The fluoxetine was discontinued by her second psychiatrist who started risperidone as a monotherapy. She started at risperidone 0.5 mg b.i.d. and was quickly titrated to 1.5 mg b.i.d. over 2 weeks. She said she felt so tired she could not leave her room.
She stopped taking the risperidone because of the somnolence and when she told her new psychiatrist she “acted angry. She said if I was not going to take my medications she could not treat me. She told me I was borderline. I barely knew this doctor so I figured this was not a good match so I found my third shrink.” The last psychiatrist started the patient on nortriptyline, which helped improve her mood for about 3 months. “That seems like my limit. After 3 months nothing works. I don't understand that. I have had these long bouts of depression that seem to last forever. Then I start to feel better, but then it happens again.” She complains that her insomnia started around the same time as starting fluoxetine. “I had trouble sleeping before that, taking hours to fall asleep or waking several times through the night. Once I started Prozac, I could not sleep well at all. I've tried Benadryl, Trazodone, and Ambien. Some of the other drugs were supposed to help me sleep, too, but it seems like once this problem began, I can't get rid of it. I don't remember having a good solid night's sleep in 3 years. I know I used to sleep well when I was younger.”
You ask what happened 3 years ago. She tells you that was when she was diagnosed with myasthenia gravis (MG). She gives you the name of her neurologist, her phone number, and signs permission for you to share medical information with her. She had noticed right before she got married that she was starting to have difficulty sustaining her energy, her legs would get weak, and sometimes her eyesight would become blurry, and she blamed it on stress. At their wedding, she tells you, she was having difficulty speaking and swallowing. She thought it was because she was nervous about the wedding but found she really could not swallow. She asked her ex-husband if she could trade her plate of food for his soup so she could eat something and he refused. “That is when I started seeing how cruel he could be.”
She reaches for more tissues. “It just got worse,” she explains. “I went to the doctor and after a bunch of tests they told me I had MG. I told my ex and do you know what he did? He had a gun and put it to his head.” She shapes her hand like a pistol and points it at her temple. “He said he was going to kill himself if I did not stop lying to him. Lying? Why would I lie about having MG? Then he pointed the gun at me and I ran out of the house. That was the only time my father actually came over to our apartment. He picked me up and took me home. But he did not say a word the entire time. Like I was causing him some huge problem. Gee, Dad, I'm sorry I'm sick! I'm sorry my husband pulled a gun on me after threatening to kill himself. It is all my fault! I'm sorry I have to get IV treatments every weekend. I'm sorry my medications are so-o-o-o-o expensive. I should just die already. What use is it to go through all this treatment if nothing matters?” She bangs her fists on the armrests of her chair.
“I'm so sick of this!” She is inconsolable for a few minutes then calms down. “They want to fire me at work all the time. I know it is because they do not want to pay my insurance or let me go to doctor's appointments, which I have every week! The bitch that sits next to me keeps a heater on all the time and she just does not get it that it makes me feel worse.” She complains that she feels depressed most of the time and finds it difficult to speak with her coworkers as she thinks they believe she is “faking her MG” to get special treatment at work. I don't have to be in early to open up, but I do stay late. I don't think my fellow tellers realize that is not a benefit!”
You ask what medications she takes for her MG. She responds that she takes cyclosporine and has weekly intravenous immunoglobulin (IVIG) treatments. She has had three inpatient treatments with high-dose steroids and was treated with prednisone for about 3 months but had to stop because she could not tolerate the medication. “I know not to drink grapefruit juice since I take cyclosporine, so don't worry about that.”
DECISION POINT C:
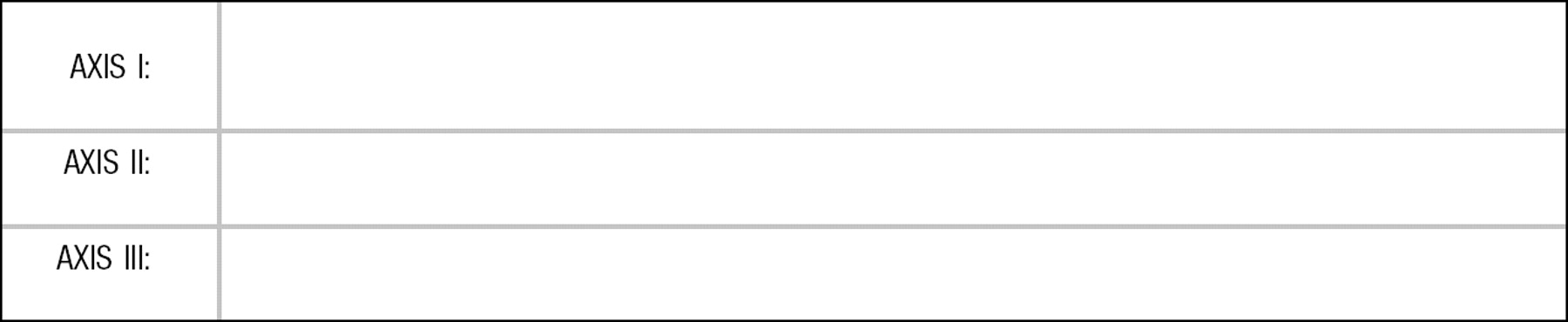
Given what you know about this patient, what is your differential diagnosis? +2 points given for correct answers, including rule-outs. −2 points are given for incorrect answers.
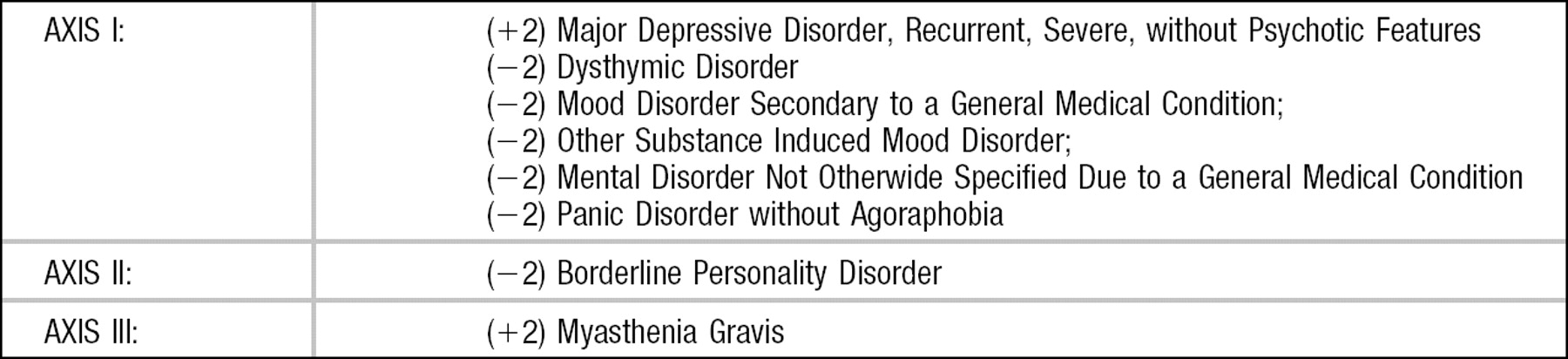
DECISION POINT D:
Which of the patient's diagnoses would you consider to be her primary diagnosis? +5 points for correct answer. 0 points for incorrect answer.
| D1.___ | Major Depression |
| D2.___ | Dysthymia |
| D3.___ | Mood Disorder Secondary to a General Medical Condition |
| D4.___ | Myasthenia Gravis |
| D5.___ | Other Substance Induced Mood Disorder |
| D6.___ | Mental Disorder Not Otherwise Specified Due to a General Medical Condition |
| D7.___ | Borderline Personality Disorder |
| D8.___ | Panic Disorder without Agoraphobia |
DECISION POINT E:
Given the patient's medication history, 1 year's worth of DBT, and the apparent resistance of her depressive symptoms to these interventions, how would you proceed with your evaluation? Points awarded for correct and incorrect answers are scaled from best (+5) to unhelpful but not harmful (0) to dangerous (−5).
| E1.___ | Obtain laboratory results of her complete blood count (CBC), liver function tests, basic metabolic panel, thyroid function panel, and cholesterol panel, and check urine toxicology. |
| E2.___ | Get permission to speak with her neurologist about her treatment for MG. |
| E3.___ | Research the psychiatric side effects of MG and the treatment she is receiving for MG. Determine what psychiatric medications would be contraindicated to use in conjunction with MG treatment. |
| E4.___ | Ask the patient about her understanding of MG and what daily life is like for her given this illness. |
| E5.___ | She has not tried a monoamine oxidase inhibitor (MAOI). Start the Selegiline patch immediately, as it will take 4–6 weeks to reach therapeutic levels. |
| E6.___ | She is at high risk for suicide and resistant to pharmacotherapy. Begin electroconvulsive therapy (ECT) treatments to achieve remission of symptoms as quickly as possible, followed by either maintenance ECT if warranted or continued pharmacotherapy. |
| E7.___ | Try a combination of cognitive behavior therapy (CBT) or interpersonal psychotherapy (IPT) with psychopharmacological intervention. |
| E8.___ | Ask for permission to speak with family members. |
| E9.___ | Consider a day treatment program or a partial program. |
| E10.___ | Ask for permission to speak with former psychiatric treating clinicians. |
ANSWERS: SCORING, RELATIVE WEIGHTS, AND COMMENTS
High positive scores (+3 and above) indicate a decision that would be effective, would be required for diagnosis, and without which management would be negligent. Lower positive scores (+2) indicate a decision that is important but not immediately necessary. The lowest positive score (+1) indicates a decision that is potentially useful for diagnosis and treatment. A neutral score (0) indicates a decision that is neither helpful nor harmful under the given circumstances. High negative scores (−5 to −3) indicate a decision that is inappropriate and potentially harmful or possibly life-threatening. Loser negative scores (−2 and above) indicate a decision that is nonproductive and potentially harmful.
DECISION POINT A:
| A1.___ | −5 This answer suggests a preconceived notion about the negative attributes of a patient with borderline personality disorder before you adequately evaluate the patient or establish a therapeutic relationship. You should keep an open mind about her diagnoses and assess her yourself before making quick judgments, especially if your countertransference toward patients with this presumed disorder will compromise your ability to treat her. |
| A2.___ | +2 This is true. You have not established a doctor-patient relationship with this woman and you are under no obligation to “begin treatment” by making a telephone call, whether it is 9 p.m. or any other time of day or night. She did make it clear by her second message that she will come to her appointment on Monday. |
| A3.___ | −5 Despite being correct about not being obliged professionally or ethically to engage this patient before establishing a doctor-patient relationship, as well as acknowledging that she has made it clear that her crisis has passed and she will come to the appointment on Monday, the final statement about her diagnosis of borderline personality disorder and your subsequent preconceived notion about how to deal with such patients suggests you would not give her appropriate and yet-to-be-determined care once she does arrive in your office. |
| A4.___ | +3 The decision to call back a patient who has not established a doctor-patient relationship with you, but was referred to you and is in apparent distress, endorsing suicidal ideation, is appropriate but, from a medico-legal perspective, not a requirement. Work done by Linehan, Rathus, and Miller suggests that the use of the telephone for coaching purposes, with chronically suicidal patients who have poor coping skills, who are engaged in DBT, and are in a crisis state, can be useful despite the paucity of evidence that it is necessary. They also contend that these patients tend not to abuse the privilege of using the telephone but find comfort knowing they could reach their therapist if they feel desperate. |
| A5.___ | +3 See answer for A4. In the absence of clear and replicated evidence that this improved some measurable outcome, the answer would receive more points. |
DECISION POINT B:
| B1.___ | +3 It is almost always recommended that patient be sent to the emergency room if you fear the patient may still be suicidal. In this case you certainly can address her risk of suicide over the telephone, but this answer suggests that you are not completely comfortable with her “flight to health” and feel that she is still at risk. A better answer would include asking whether there are any other family members, friends, or social supports who could be called to check on the patient immediately. Additionally, you should evaluate whether the patient is able to bring herself to the emergency room or whether you should send emergency medical services to pick her up. |
| B2.___ | +3 See answer for B1. Whether you have admitting privileges at the nearest emergency room is immaterial to her safety. |
| B3.___ | +4 You have assessed the patient over the phone and concluded that she can keep herself safe and has well-thought-out plans for maintaining that safety, and you have a follow-up plan to see her. She should be reassessed, however, the next day, especially if you do not know the patient well. A suggestion to call you or to call the local emergency room or crisis line to call the next day would be appropriate, assuming you would be available for follow up on this plan.___ |
| B4.___ | −5 Although the evaluation and plan seem perfectly reasonable and you are confident in the patient's ability to remain safe, you made the mistake of reacting to your preconceived notions of a patient for whom another clinician diagnosed borderline personality disorder. Your job as the new treating clinician, assuming you accept this patient into your practice once you meet her, is to perform your own complete evaluation and diagnose according to your own impressions. A great disservice is done to patients who have been labeled with certain especially stigmatized illnesses such as borderline personality disorder by subsequent doctors who blindly accept the diagnosis, are influenced by its perceived negative attributes, and begin a doctor-patient relationship with prejudice. |
| B5.___ | −5 You do not know this patient. If you do not feel she is safe, it is appropriate to assess her in person. However, this should be done in an emergency department for both the patient's protection and for your protection. You are not required to be the psychiatrist who assesses her. She has not given you the impression that she is psychotic, but there have been cases of doctors being assaulted or even killed by psychotic patients who were seen in an emergency situation in a private office. |
DECISION POINT C:
(+2) Major Depressive Disorder, Recurrent, Severe, without Psychotic Features: The patient meets the criteria, having depressed mood and anhedonia, explaining that she is bored by things she normally enjoys doing. She complains of poor mood most of the time, disturbed sleep, fatigue, feelings of hopelessness, helplessness, worthlessness, difficulty at work, and recurrent suicidal ideation. Her worry that co-workers consider her to be “faking” an illness to get special treatment was not fully explored as a paranoid delusion as she does leave work weekly, is excused from arriving at work early, staying late instead, and she does not express any other psychotic symptoms.
(−2) Dysthymic Disorder: The patient does report feeling depressed more often than not, but has had remission of symptoms each year lasting up to 3 months at a time. Subsequently she does not meet the criteria for dysthymic disorder, which requires depressive symptoms more often than not for a consecutive period of 2 years.
(−2) Mood Disorder Secondary to a General Medical Condition: There is sparse literature regarding psychiatric manifestations related directly to MG. It is likely the major depressive symptoms experienced by the patient are not the direct result of the physiological illness but rather the experience of the illness, ruling out this diagnosis.
(−2) Other Substance Induced Mood Disorder: The medications the patient takes for MG include cyclosporine and weekly IVIG treatments. IVIG can cause anxiety, chills, dizziness, drowsiness, fatigue, fever, headache, irritability, lethargy, malaise, and aseptic meningitis syndrome. Some researchers have linked it specifically to depressive symptoms, especially when it is used as a treatment for cytokine-induced illness. Cyclosporine by itself is not known to cause psychiatric side effects. In the past the patient has received pulses of high-dose steroids and spent approximately 3 months taking prednisone, which she stopped because she was not able to tolerate it. It is well known that the use of steroids can cause psychosis and mood dysphoria. However, she is not taking these medications and has not them in awhile, and there is little evidence of these psychiatric side effects lasting after the discontinuation of the medication. One cannot, of course, rule out this possibility.
(−2) Mental Disorder Not Otherwise Specified Due to a General Medical Condition: This diagnosis is reserved for situations in which the psychiatric symptoms are directly related to physiological effects of the medical condition, but the criteria are not met for a specific mental disorder due to a general medical condition. A direct link between the physiological effects of MG and psychiatric manifestations has not been adequately established.
(−2) Panic Disorder without Agoraphobia: The patient has not given any information that would lead you to this diagnosis. You should explore the history of this diagnosis, however, in future sessions to determine whether the patient had panic attacks in the past and if she would require continued antidepressant medication that would address this diagnosis.
(−2) Borderline Personality Disorder: This patient has unstable interpersonal relationships with coworkers and with her family. She gave no indication that she felt this way before the onset of her MG. Additionally, she does not display frantic efforts to avoid real or imagined abandonment, her interpersonal relationships are not characterized by alternating extremes of idealization and devaluation, she has not demonstrated or indicated she has an unstable self-image or sense of self, and she does not display affective instability. She does have recurrent suicidal ideation, not behaviors, she is impulsive in her maladaptive coping behavior of self-harm, does have chronic feelings of emptiness and seems to have a great deal of anger and possibly stress-related paranoid ideation. However, the feelings of emptiness, anger, and possible paranoia all can be traced to discernable and understandably reasonable psychosocial stressors. Her anger is not disproportionate or inappropriate, and she has worked at the same job for 5 years, indicating her behavior at work is probably not considered intolerable. The reasons for the bank not promoting her may have nothing to do with her psychiatric symptoms or personality structure. Finally, the symptoms that caused previous clinicians to label this patient as having borderline personality disorder may have been more severe in the past, but your present evaluation does not suggest an axis II diagnosis, but rather the sometimes maladaptive, but otherwise seemingly appropriate reaction to psychosocial and personal stressors relating to her medical illness.
(+2) Myasthenia Gravis: True; this is her medical diagnosis and belongs in axis III.
DECISION POINT D:
| D1.___ | (+5) Major depression. See answers for Decision Point C. She does have a primary neurological illness, myasthenia gravis, and this is very likely the precipitant for her mood symptoms. However, in the context of a psychiatric evaluation, her primary diagnosis is major depression, recurrent, severe, without psychotic features. |
DECISION POINT E:
| E1.___ | (+5) Before making a decision about pharmacotherapy, and especially after this patient has been taking medications that have harmful effects on liver, kidney, and thyroid function, as well as a risk for metabolic syndrome, it is prudent to get baseline laboratory values to better inform your decisions. Additionally, it is important to rule out other medical conditions that may be causing the depression, such as anemia, occult malignancy, hypothyroidism, or substance abuse. |
| E2.___ | (+5) It is good practice to coordinate care with other treating clinicians, especially those who are concurrently treating a major medical condition. You and the other clinicians will be better informed about the conditions each is treating, and establishment of such collaborative relationships will enhance the overall treatment of the patient. |
| E3.___ | (+5) This patient has a major neurological condition. If you do not already have expertise in the area of MG, a better understanding of the illness will enhance your informed decisions regarding the psychiatric issues you are treating. Finally, although the treatment with steroids stopped 3 months before you met the patient, the medication could have had an impact on her condition. For all of these reasons, close collaboration with her neurologist and obtaining as much collateral information as possible will help you in your diagnosis and treatment. |
| E4.___ | (+5) Exploring the patient's understanding of her MG, as well as her day-to-day experience coping with this illness, will better inform your psychiatric evaluation and understanding of the patient's daily life experiences. |
| E5.___ | (−5) She is taking venlafaxine and quetiapine. Trying an MAOI is a reasonable choice given that she has not done well when taking numerous other classes of antidepressants, mood stabilizers, and neuroleptic medications, and the MAOIs are indicated for treatment-resistant major depression. However, before starting an MAOI she must be weaned slowly from venlafaxine as its half-life of 5 hours along with the 11-hour half-life of its metabolite, O-desmethylvenlafaxine, causes a withdrawal syndrome. Venlafaxine is contraindicated for concurrent use with MAOIs because of the risk of serotonin syndrome (hypertension, hyperthermia, myoclonus, tremor, diarrhea, and mental status changes), so the transition must follow a washout period of 5 times the drug's half-life or at least 2 weeks (5 weeks if transitioning from fluoxetine, whose half-life is 84 hours or 7 days if its metabolites are included). This patient was taking venlafaxine 450 mg, which is twice the recommended upper-end dose. There is little evidence that this medication is more effective at more than 225 mg daily. Moreover, this patient has a greater likelihood of achieving remission of symptoms with ECT as treatment-refractory severe major depression is a clear indication for such treatment, long before so many medications were tried. |
| E6.___ | (+5) If the patient is willing, ECT is entirely appropriate, is clearly indicated, and could have been tried earlier than at this stage of her treatment, given her poor response to all other medication trials. It has also been demonstrated that muscle relaxants and ECT premedications can safely be given to patients with MG with appropriate precautions. Many argue that ECT should be tried after as few as two “failed” antidepressant trials. This patient has taken numerous antidepressants including selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, an atypical antidepressant (bupropion), and tricyclic antidepressants, as well as atypical neuroleptics, two mood stabilizers, and an assortment of benzodiazepines and hypnotics. The response rate to ECT is generally accepted as being in the 70%–90% range in patients who have not already demonstrated such resistance to pharmacotherapy, and it is efficacious in 15%–20% of pharmacotherapy treatment-resistant patients. Antidepressants generally will lead to full remission of symptoms in 50% of patients with treatment at an adequate dose for at least 6 weeks, 10%–15% will show some improvement, and the remainder will have little to no improvement of symptoms. Although ECT is not indicated for treatment of personality disorders, borderline personality disorder has not been clearly established and may have spuriously been diagnosed. The severity of her mood symptoms warrants immediate action. |
| E7.___ | (+5) Although there is an increasing number of studies indicating the effectiveness of IPT for depression (in this case, the patient's interpersonal relationships seem to be worsening her symptoms of depression since she became sick with MG) and CBT, especially when combined with psychopharmacological interventions, the gravity and duration of her severe symptoms suggest the need for immediate intervention, such as ECT. Once the severe symptoms have remitted, beginning psychotherapy such as IPT or CBT in conjunction with a pharmacological intervention such as an MAOI (given the history of her poor response to other classes of medications) may be appropriate for maintenance, and many studies indicate that this approach is more effective than pharmacotherapy alone. |
| E8.___ | (+5) The patient gave permission to call the neurologist and provided contact information. This will help you to firmly establish the diagnosis of MG, determine the medications the neurologist is using, and work collaboratively to help the patient's psychiatric issues. Further background obtained from family will help shed light on any prior psychiatric condition that may have existed on its own or become manifest because of the neurological condition of MG. Additionally, a family meeting will help you better understand the function of this family system and its potential for being supportive to the patient. The patient, of course, would have to consent to your speaking with her parents, with whom she clearly has a difficult relationship. You want to preserve your therapeutic working relationship and at the same time gather as much collateral information about the patient as is possible. Your approach to asking the patient's permission will therefore need to be empathic toward her difficulties with her family, but clear about the medical benefits from your being able to discuss hers and her family's history. |
| E9.___ | (+5) Given the difficulty the patient has with continuing work and the fact that she seems to be doing so to keep her insurance active, an exploration with the help of a social worker into a part-time or day hospitalization program until she is more stable may help this patient recover and more rapidly obtain additional services if such are available to her in her area. |
| E10.___ | (+5) Absolutely. You cannot proceed in this case without first speaking with as many of her previous clinicians as you can to determine why medications were chosen, how long they were used before something else was tried, what were the criteria for moving between agents, what were the results of each trial, why were so many medications tried before ECT was considered, and where did the diagnosis of borderline personality disorder come from. The other clinicians will provide invaluable information in a complicated case such as this. |