Patient interview
Detailed information about the nature of the complaint is necessary, such as if insomnia is related to sleep onset, sleep maintenance, early morning awakening, nonrestorative sleep quality, or a combination of these problems. Information obtained here may help to guide the diagnosis, such as a sleep-onset complaint resulting from restless legs syndrome as opposed to an early morning awakening presenting as part of a depressive disorder. Additional information about the onset, course and duration, current presentation, frequency, severity, and precipitating or alleviating factors also helps to define the problem. In particular, a life-long course with an onset in the absence of medical and psychiatric comorbidities may suggest a primary insomnia as opposed to a secondary insomnia that develops in late adulthood in the context of chronic pain.
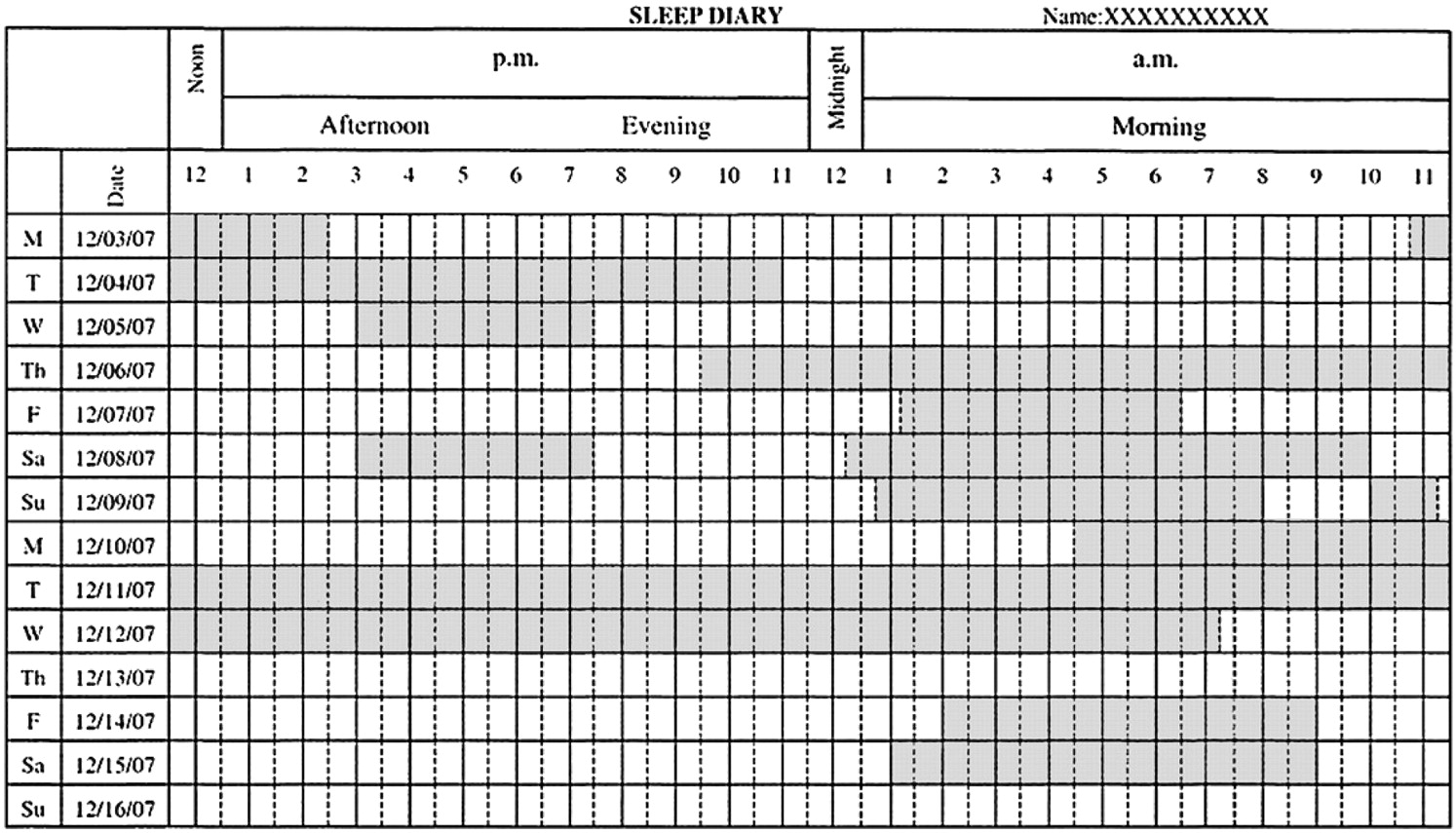
The sleep schedule, including bedtime, sleep latency, number and length of nighttime awakenings, sleep reinitiation time, wake time, time spent in bed, and total sleep time, should be reviewed. A patient's preferred bedtime may not coincide with actual bedtime, as in a circadian rhythm disorder. Similarly, nighttime awakenings caused by nightmares from posttraumatic stress disorder as opposed to awakenings from nocturia caused by prostate enlargement suggest different disorders.
The daytime routine with a review of work schedule, eating and exercise times, and duration and timing of naps is also important. Eating and exercise times that occur in close temporal relation to bedtimes may inhibit the patient's ability to fall asleep. Moreover, naps of long duration that occur in the late afternoon or evening may have a similar negative effect on sleep latency and continuity.
A discussion of daytime functioning and associated symptoms includes daytime sleepiness; fatigue; difficulty with memory and concentration; depression; anxiety; irritability; impairment at work, school, or home; and overall quality of life. A report of daytime impairment and patient distress may underscore the severity of symptoms, and highlight the need aggressively to treat insomnia. In this area, collateral report from family, teachers, or coworkers may prove helpful if the patient is unaware of the extent of his or her symptoms.
Safety issues, such as the negative effect on driving and work performance in potentially hazardous areas, should be broached and may provide an opportunity for patient education.
Sleep conditions and routines should be discussed, such as the conditions of the room used for sleep (eg, effect of light, temperature, and noise); use of television, computer, or radio both in the prebedtime routine and during periods of nighttime awakenings; the effect of anxiety during sleep latency and sleep reinitiation periods; and the presence of clock-watching before and during sleep times. Too much noise or light exposure in the sleeping room may inhibit sleep initiation. Similarly, clock-watching with each nighttime awakening may only further heighten an already raised level of anxiety. Specific difficulty falling asleep at home but not while out of town may suggest insomnia related to the bedroom environment.
Previous treatments tried and their effects and side effects should be discussed. Treatments may include over-the-counter, homeopathic, herbal, or prescription medications and behavioral therapies. In addition to providing information on potential treatments that may not have yet been offered to the patient, information obtained in this area may provide a sense of the kind of treatment for which the patient is looking.
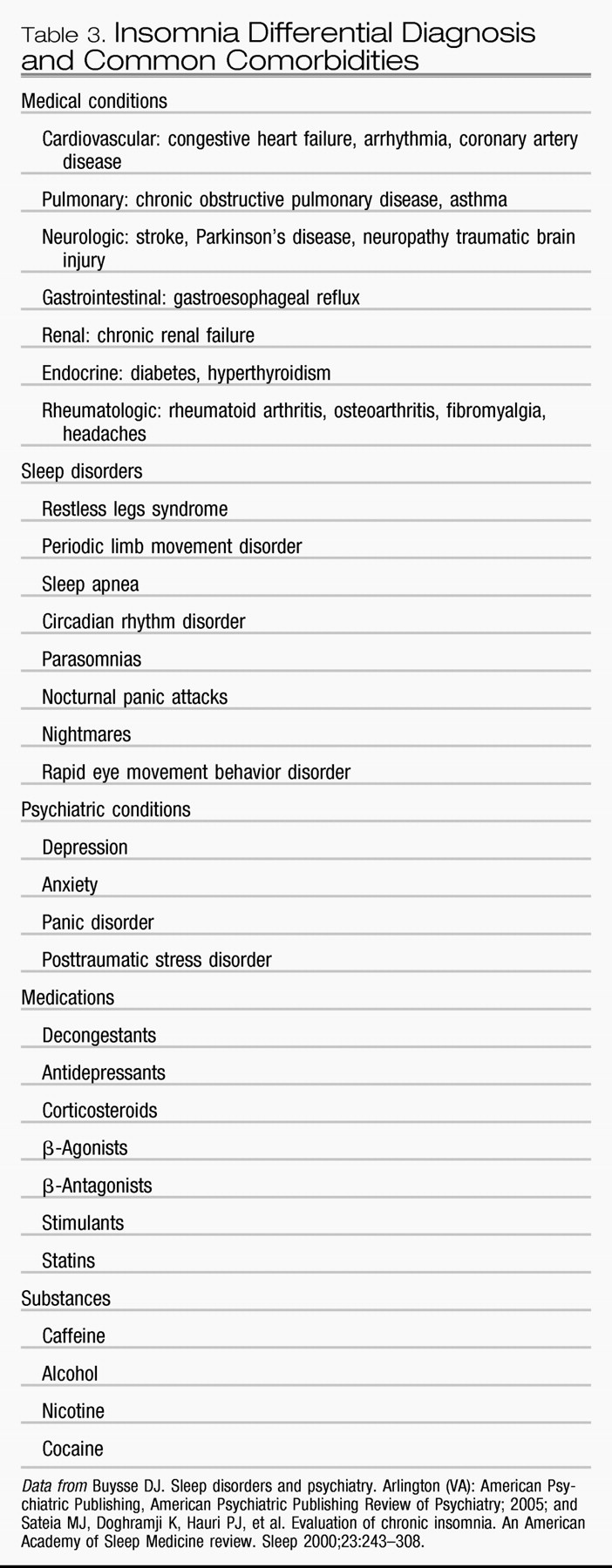
Symptoms of other sleep disorders that could be affecting the complaint include such conditions as restless legs syndrome, periodic limb movement disorder, sleep apnea, and sleep phase syndromes. These should be considered as possible contributors to insomnia.
One should review comorbid medical conditions that could play a role in the presentation. General categories to consider include cardiovascular, pulmonary, neurologic, gastrointestinal, renal, endocrine, and rheumatologic.
Review of underlying psychiatric conditions and psychosocial stressors should be included. Eliciting symptoms of depression, bipolar disorder, anxiety, panic (including nocturnal panic attacks), and psychosis can help to clarify the diagnostic picture while emphasizing the need to obtain or continue psychiatric care.
A review of substance use, including nicotine, alcohol, and caffeine, should cover amount, frequency, and time of day the substance is used because all of these substances may contribute to an insomnia complaint. Patient education about the effects of nicotine, alcohol, and caffeine on sleep should also be undertaken if it seems that substance use has a negative effect on sleep quality.
Finally, one should undertake a review of family history of sleep, medical, and psychiatric disorders.