The care of people living with addiction is ethically complex work. Addiction is stigmatized in our society (
1,
2), and clinical services for addiction-related conditions are underdeveloped, raising many ethical issues related to respect, confidentiality, and justice. Addictions of all kinds are associated, by definition, with a lack of personal control over the addictive behavior and are often linked with intermittent or enduring cognitive deficits, creating concerns about affected individuals' capacities for autonomy and shared decision-making with caregivers (
3–
6). Some addictions are associated with risky and/or illegal activities, introducing very difficult considerations related to dangerousness, self-neglect, or self-injury and potential harm toward others (
7). Moreover, the history of treatment for addiction has been riddled with approaches that emphasize punitive consequences, raising issues pertaining to beneficence, nonmaleficence, and medical professionalism (
8). Finally, addiction often co-occurs with other health conditions, which may be difficult to recognize and burdensome to treat because of the addiction, raising ethical issues related to clinical competence. For these reasons, every aspect of clinical care for addictive disorders should be viewed as having important ethical meaning and implications.
Ethical dilemmas in clinical care occur usually because of a conflict between two “good” things or positive values. Such conflicts may involve balancing the need to confront a patient directly about an emerging substance use problem while he or she is going through a difficult divorce, i.e., to act with honesty, with the wish to be empathic and supportive of the patient during a stressful life experience, i.e., to act with compassion, beneficence, and nonmaleficence. Likewise, a clinician who is a provider in a court-mandated treatment intervention or a psychiatrist who performs pretransplant evaluations may be in the difficult position of influencing the decision of whether a patient returns to jail or is denied a life-saving liver transplant because of ongoing addiction issues and lack of treatment adherence. Situations such as these challenge the self-concept of conscientious physicians as professionals who “do good.”
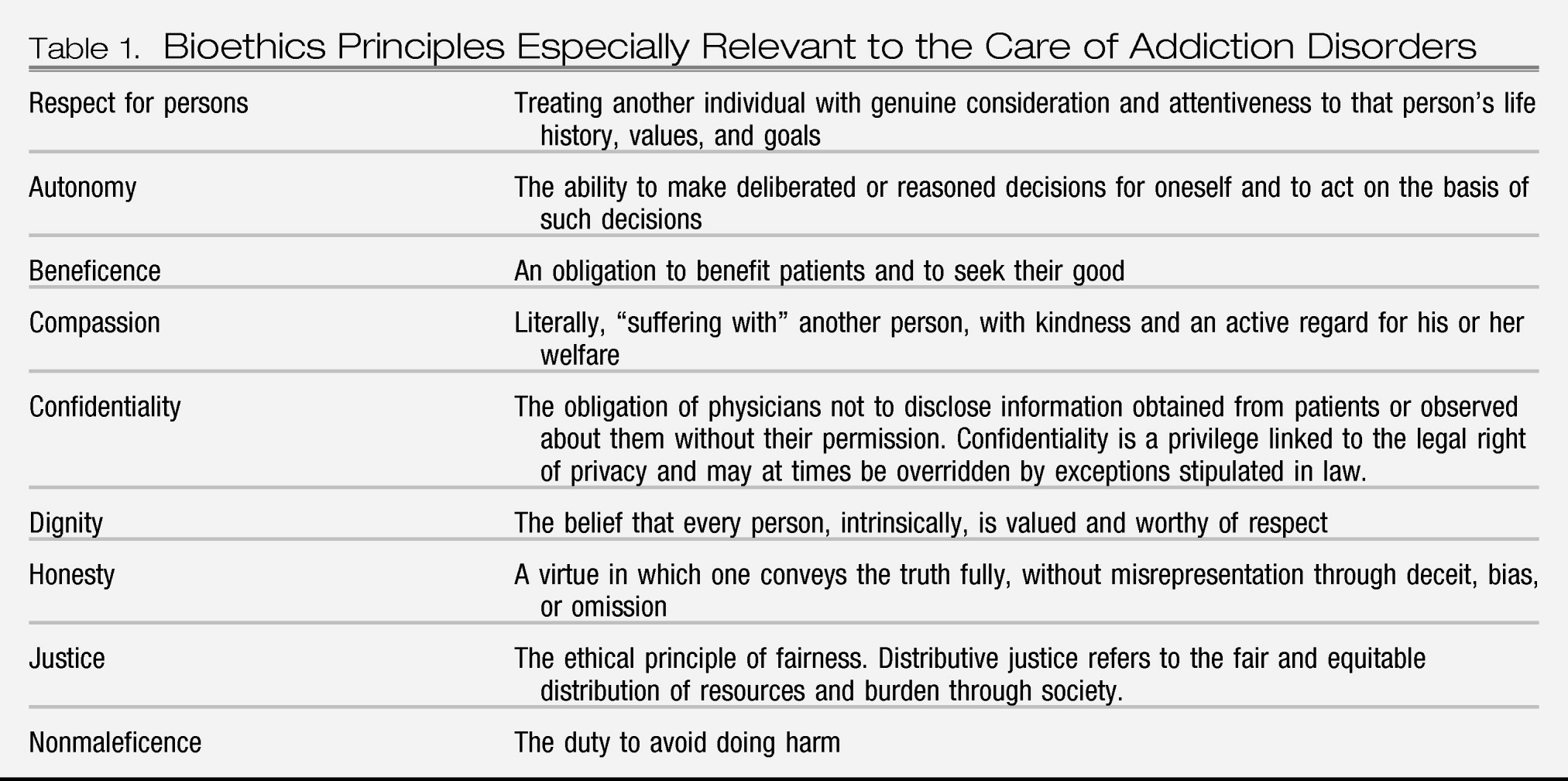
Table 1 describes relevant ethical principles in addiction care.
Newer approaches to treatment, as demonstrated in the articles in this issue of
FOCUS, have done much to advance the field of addiction care and, with it, the underlying ethics of this special clinical work. For example, Danovitch (
9) illustrates the
Five As clinical practice guidelines in his article in this issue. Motivational interviewing is particularly oriented toward supporting patient strengths (respect, autonomy) and the reduction of harm (nonmaleficence) associated with consequences of addiction. It is affirming (beneficence) and empathic (compassion) in its approach and has a strong evidence base of effectiveness (beneficence). It emphasizes transparency (honesty) while sidestepping the problem of punitive limit setting or enabling pathological behaviors (nonmaleficence).
People living with addictions often become “difficult” patients (
10). Providers may have naturally negative reactions (countertransference) when treating patients who minimize or lie about their substance use patterns or who do not adhere to prescribed treatments. These issues may be of greatest concern when patients resemble their caregivers, for example, when the patient is a colleague or an accomplished professional. Patients who are perceived as drug seeking and who recruit a psychiatrist into “rescuing” them with medications that have addictive potential are particularly troubling. When patients are unkempt, disheveled, impulsive, threatening, agitated, or belligerent, providers can react quite strongly.
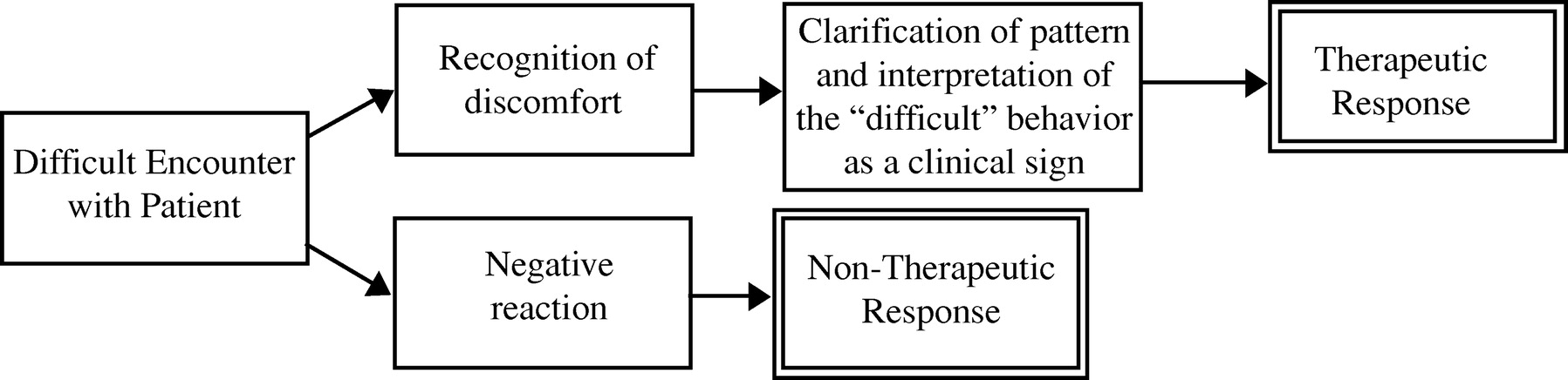
The key to ethically competent care of patients with complex problems is to remember that “difficult” attributes are a clinical sign—a manifestation of an illness process that should be recognized for its informational value in the care of the patient (
Figure 1). A psychiatrist who exhibits true professionalism will seek a therapeutic response to the situation, which may be as basic as ensuring the safety of the patient, keeping the patient engaged in care, and avoiding reactions that may be anchored in prejudicial attitudes rather than self-reflective clinical skills.
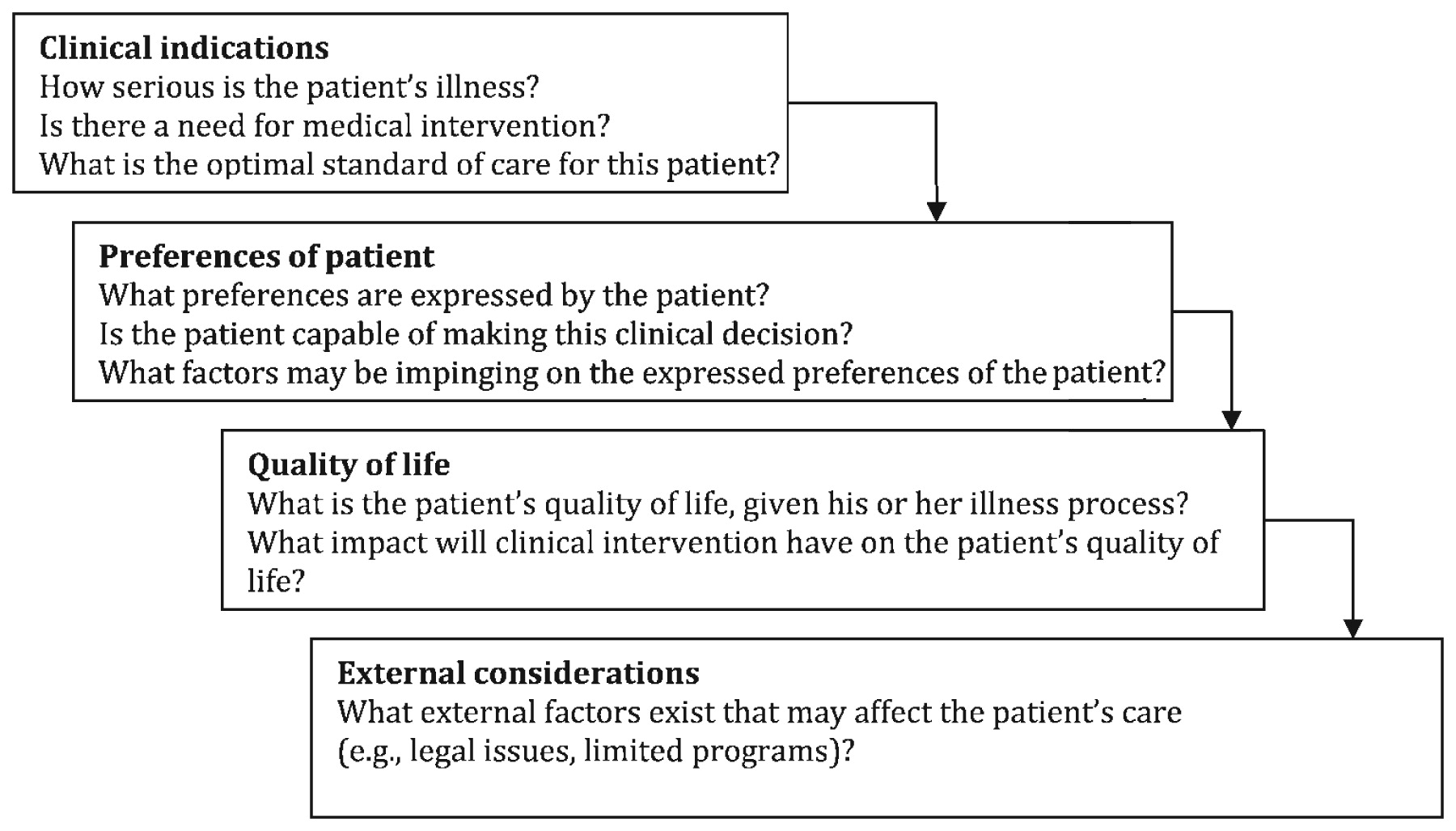
Figure 2 describes steps for optimal clinical ethical decision-making, and
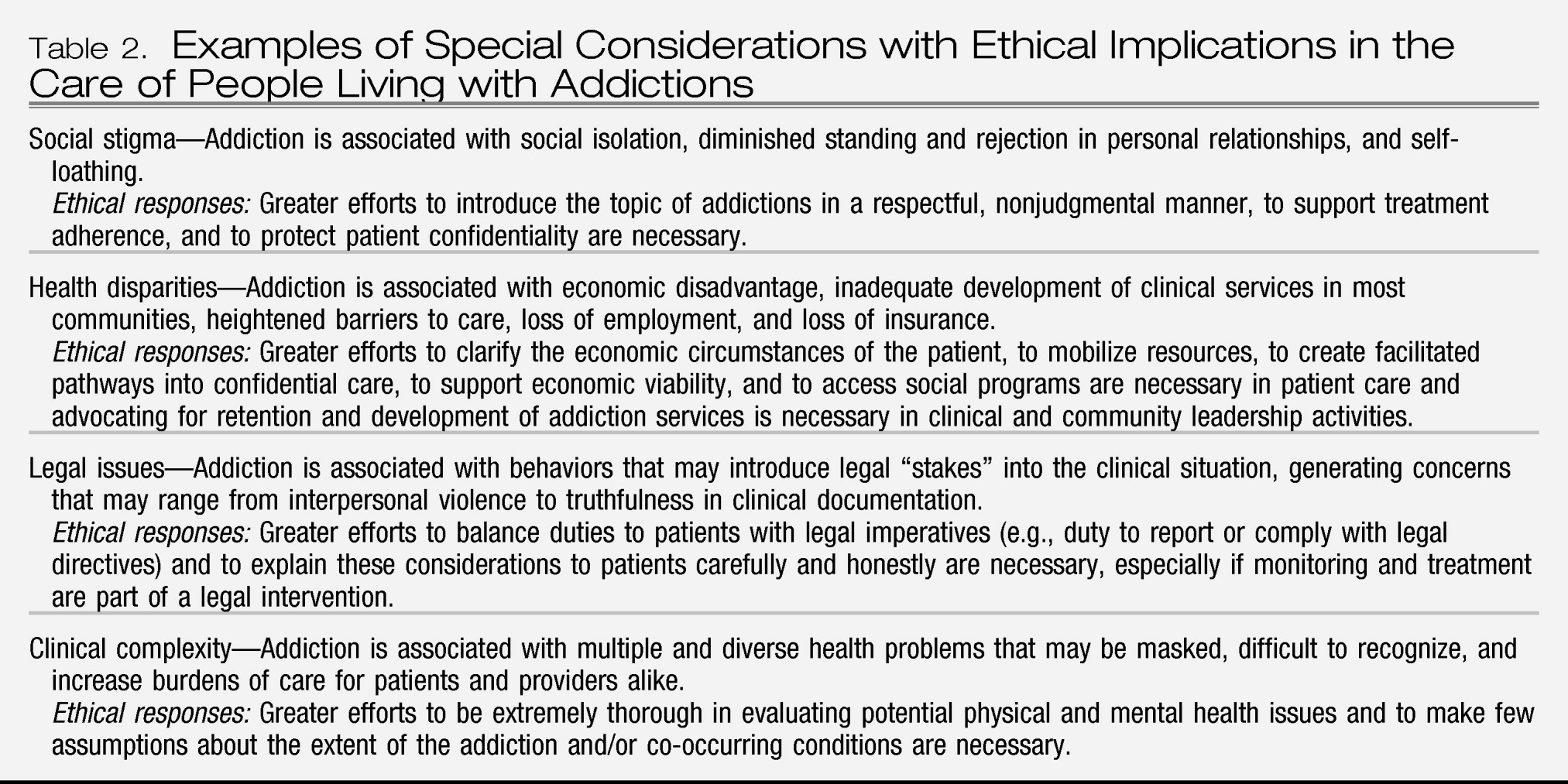
Table 2 provides special considerations in the care of people with addictions, including ethical responses.
Roughly 9% of the population fulfilled the diagnostic criteria for substance dependence or abuse in the past year according to results from the 2009 National Survey of Drug Use and Health. Lifetime estimates of addiction are now thought to be as high as 35%, which is higher than earlier estimates of closer to 15% (
11,
12). Experimenting with substances occurs early. Among eighth graders, 37% report having tried alcohol, 16% have tried marijuana, and 28% have tried some illicit drug other than marijuana (
13). More than 1 million persons with addiction received treatment at outpatient mental health centers and 714,000 in a private doctor's office.
For these reasons, addictions represent a critical concern for public health and a clinical area of competence necessary for all practicing psychiatrists. People with addictions deserve appropriate care, characterized by the ideals of the profession including dignity, respect, and compassion. This aspiration represents a profound challenge, particularly given the underdeveloped system of care that exists in this country for people with addictions. For example, of the 23.5 million persons in need of treatment for an illicit drug or alcohol use problem, only 11.2% received treatment in 2009 (
14). This fact alone suggests that psychiatrists will find themselves having to “stretch,” i.e., to serve in extended roles without adequate preparation or support to provide adequate clinical care for people living with addictions. Because addictions are increasingly prevalent, psychiatrists' strengths, including their deeply held professionalism, will be increasingly called upon to address the complex concerns of this underserved population in the years ahead.