Psychotic symptoms represent one of a number of psychiatric comorbid symptoms or diagnoses associated with chronic posttraumatic stress disorder (PTSD). Other DSM-IV-TR diagnoses include major depression, generalized anxiety disorder, panic disorder, social anxiety disorder, agoraphobia, and alcohol or drug abuse or dependence (
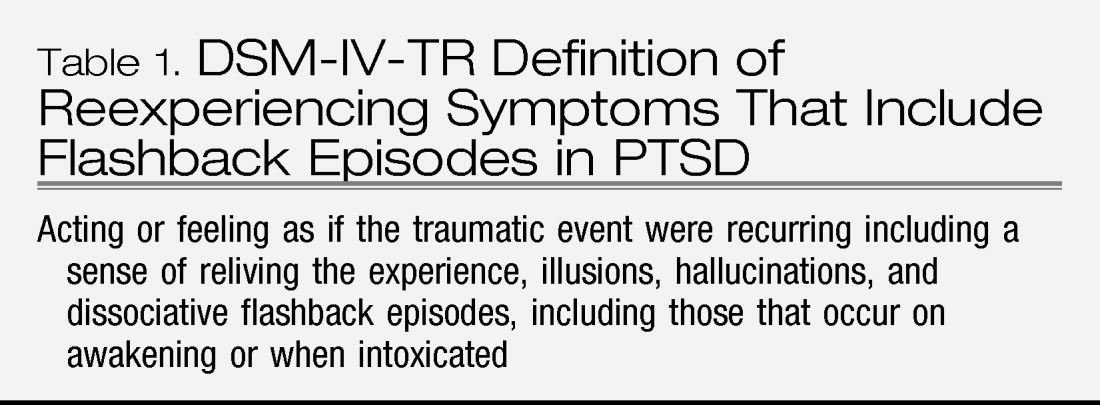
1). Many of these comorbidities also overlap, from a phenomenological standpoint, with the diagnostic symptoms for PTSD. Importantly, psychotic symptoms are included in the definition of criterion B for reexperiencing symptoms, i.e., sudden acting or feeling as if the trauma was recurring (
Table 1). These symptoms may include illusions, hallucinations, and dissociative flashback episodes.
The clinical description of the disorder primarily has been consistent with positive psychotic symptoms, e.g., auditory or visual hallucinations of combat experiences (e.g., people screaming, gunfire, explosions, and others) but with infrequent descriptions of delusions or thought disorder. These symptoms do not occur exclusively during dissociative flashback episodes and are often chronic in nature. If delusions do occur, they are primarily paranoid or persecutory in nature. The lack of complex hallucinations, delusions, or formal thought disorder helps differentiate PTSD with psychotic symptoms from schizophrenia or schizoaffective disorder. Therefore, chronic psychotic symptoms that do not occur strictly during flashback episodes have been of increasing interest. The following case vignette illustrates these symptoms
Mr. A is a 64-year-old veteran of Vietnam combat. He was involved in the Tet offensive and other battles during his tour of duty in the Army between 1968 and 1969. He presented to the PTSD clinic on referral from his primary care physician with a complaint of insomnia and nightmares. He also endorsed intrusive memories of Vietnam combat; psychological reactivity when exposed to reminders of Vietnam or war; avoidance of reminders of war or violence, social isolation, anhedonia; and hyperarousal symptoms including difficulty concentrating, hypervigilance, exaggerated startle, irritability, and the above-noted insomnia. Of particular note, he was most troubled by intermittent visual hallucinations of “burned faces” of soldiers he had seen in an especially intense combat episode. The hallucinations occurred almost daily during the day or night and “seemed real” to the patient. He described in vivid detail the characteristics of the faces, what it was like to see the burned flesh, and so forth. He also had intermittent olfactory hallucinations of “burning flesh” that were simultaneous with the visual hallucinations. The hallucinations could “happen for hours” and were highly distressing. He did not necessarily have other reexperiencing symptoms at these times. He was embarrassed about the symptoms and confided that he had not discussed them with others. His global PTSD symptoms and the hallucinations improved modestly with a combination of sertraline and risperidone and continued supportive therapy. Although he continued to have the hallucinations, they became less intense and frequent.
A comprehensive summary of studies investigating PTSD and secondary psychotic features (PTSD-SP) was conducted by Braakman et al. (2). Twenty-four comparative studies were included in their article. These authors concluded that there currently is not yet full support for PTSD-SP as a nosological entity. However, the delineation of PTSD-SP from other psychiatric syndromes is notable and biological studies seem to support the validity as a separate diagnostic entity. This article is reviewed more in depth below because it offers one of the most comprehensive reviews of the literature to date.
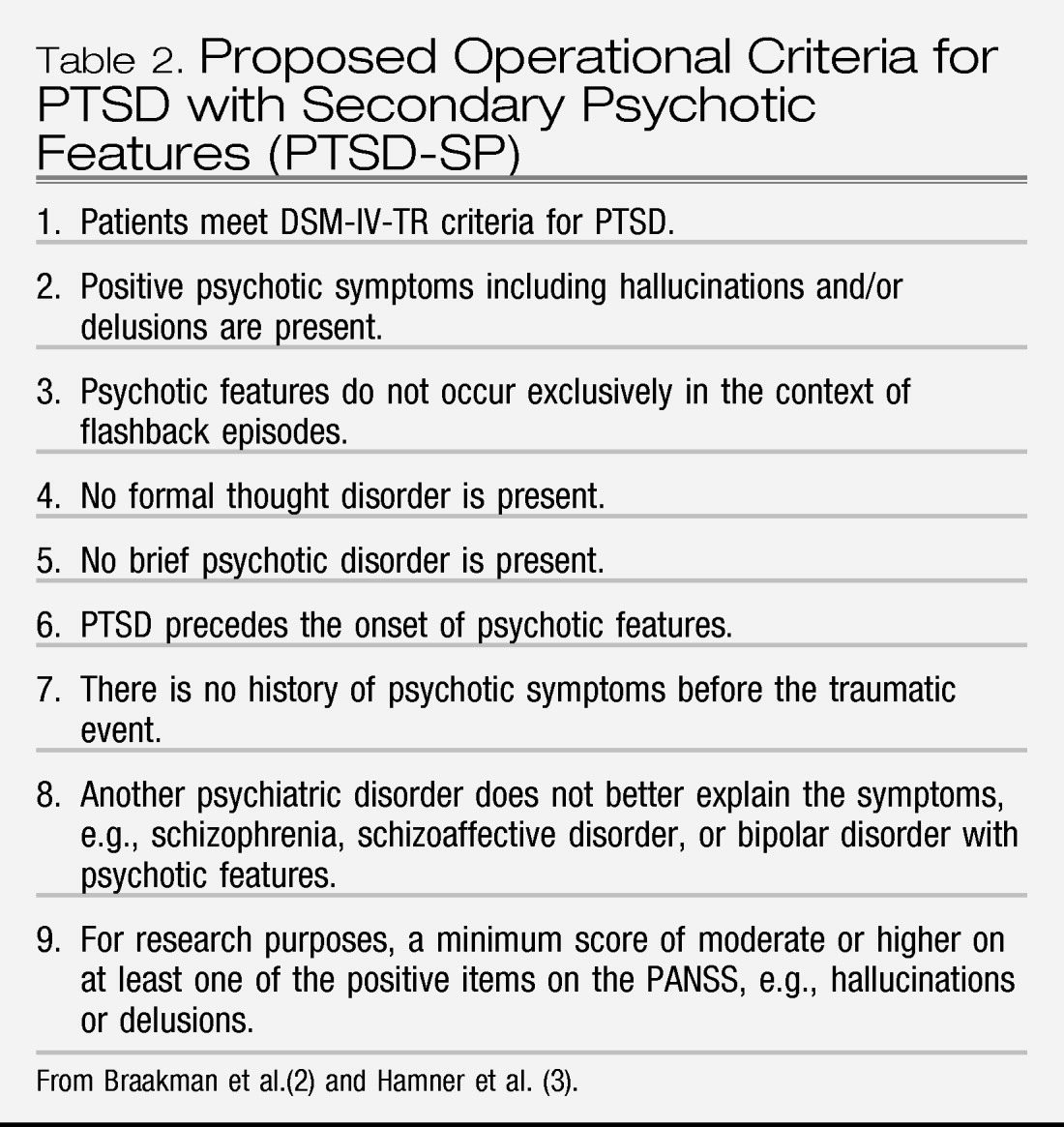
Operational criteria for these symptoms may include the following: symptoms occur after the onset of PTSD and patients do not meet the criteria for another psychotic disorder, e.g., schizophrenia, major depression with psychotic features, schizoaffective disorder, bipolar disorder with psychotic features, brief psychotic disorder, or psychosis associated with substance abuse. These latter diagnoses are important to consider in the differential diagnosis.
We and others have also proposed a certain threshold severity for these symptoms for research purposes, e.g., a score of at least moderate or higher on one of the positive symptoms items on the Positive and Negative Syndrome Scale (PANSS) items, e.g., hallucinations or delusions (
3,
4) (
Table 2). The term
PTSD with secondary psychotic symptoms (PTSD-SP) has been proposed to describe this syndrome. The following is a compilation of possible criteria for PTSD-SP as proposed by Braakman et al. (
2), David et al. (
5), Sautter et al. (
6), and others (
3).
Early work by our group found an association between the severity of global as well as core (i.e., reexperiencing) PTSD symptoms and psychotic symptoms (
3). This was furthered by work finding a correlation with severity of comorbid major depression (
3) but not an association with alcohol or substance abuse. Of particular interest regarding comorbid psychosis and severity of illness was a comparison of illness severity in PTSD and in schizophrenia (
4). As expected, the patients with schizophrenia had modestly higher PANSS scores, but this was accounted for largely by more complex delusions or hallucinatory phenomena. Otherwise the symptom burden on this rating scale was remarkably similar between the two illnesses.
Along these lines, Sautter et al. (
7) compared PTSD without psychotic features, PTSD-SP, and healthy comparison subjects using the Family Interview for Genetic Studies (FIGS). There was an increased risk for psychiatric disorder (depression) in the patients with PTSD but not for psychotic disorder. This, of course, contrasts with findings in schizophrenia in which one would expect to find an increased risk for psychotic disorder. Thus, family history of psychosis per se may not be useful in delineating psychotic symptoms in a particular patient; this was the case in the patient presented above.
EPIDEMIOLOGY
Earlier studies suggested that the prevalence of PTSD-SP may be up to approximately 40% of veterans with PTSD. These were single site studies that had differing definitions of PTSD with psychotic symptoms (
8). Of note, there may be ethnic variations in the manifestation of psychotic symptoms (
9,
10).
Sareen et al. (
11) described the high co-occurrence of positive psychotic symptoms and PTSD in the National Comorbidity Study. PTSD was found to be associated with an increased likelihood of endorsing one or more psychotic symptoms after adjustment for sociodemographics and psychiatric and medical comorbidity [odds ratio (OR)=1.83; 95% confidence interval (CI) 1.43–2.45, p<0.001]. The co-occurrence of PTSD with psychotic symptoms was associated with greater levels of severity (higher total number of PTSD symptoms, greater levels of comorbidity, and high distress) compared with that for PTSD alone.
A recent additional analysis of data from the National Comorbidity Study further supported evidence for a psychotic symptom subtype of PTSD (
12). Shelvin et al. (
12) reported on a latent class analysis of PTSD symptoms and psychotic symptoms including hallucinations and delusions. Four latent classes were identified. Two had high probabilities of endorsing hallucination and delusion indicators. One class had high probabilities of endorsing both psychosis indicators and PTSD symptoms. This class met the characteristics expected to be evident in a psychotic PTSD subtype.
In contrast, Gaudiano and Zimmerman (
13) argued that their data did not support a psychotic subtyping of PTSD. These researchers assessed 1800 patients who completed diagnostic interviews. The lifetime prevalence of psychotic symptoms in this sample was 17% (OR=3.48, 95% CI 2.52–5.21). Excluding comorbid conditions associated with psychosis, the prevalence of PTSD with psychosis was 2.5% (OR=0.6, 95% CI 0.08–4.52). Rates of major depression did not change between PTSD with or without psychosis. Although the conclusions of this study appear to be conflicting, it does not address the fact that there is a strong overlap between symptoms of PTSD and those of depression, e.g., irritability, difficulty concentrating, insomnia, diminished interest or participation in significant activities.
Many patients with PTSD meet the criteria for major depression, and, in fact, there is a substantial symptom overlap between the two disorders. Moreover, some studies have demonstrated a positive correlation between the severity of depression and psychosis in patients with PTSD (
3,
14). However, clinical descriptions also are published in these comparative studies of patients with PTSD-SP who do not have comorbid depression.
To summarize the epidemiology, there evidently may be a broad range in the prevalence and manifestation of psychotic symptoms in PTSD.
SUPPORTING EVIDENCE FOR THE CONCEPT OF PTSD-SP
Braakman et al. (
2) have provided the most comprehensive comparative study regarding the validity of PTSD-SP, which is elaborated on here. These authors used the criteria of Robins and Guze as applied to a psychiatric syndrome.
They reviewed a total of 184 publications on PTSD, trauma and psychosis, or psychotic features. They excluded 126 publications because of a primary focus on other diagnoses besides PTSD, other psychotic disorders preceding the onset of PTSD, e.g., schizophrenia, clear postpsychotic PTSD (i.e., psychosis per se may have caused the PTSD), and psychosis in childhood or adolescents. This resulted in 58 articles on adult PTSD-SP. Of these, 16 were excluded because they did not contain original empiric data. Moreover, 18 were excluded because they were below level three of evidence. Finally, a total of 24 studies were included for comparison. Fourteen of these studies were conducted in U.S. male combat veterans.
As noted by Braakman et al. (
2), the supporting evidence for PTSD-SP is strong in several of the Robins and Guze criteria. However, more data are needed regarding the longitudinal course of illness and family history before PTSD-SP could be defined as a distinct entity. A consistent definition of the syndrome is needed and is proposed above and in
Table 2.
BIOPSYCHOSOCIAL UNDERPINNINGS
Biological studies
Several biological studies support the notion that PTSD-SP may be a distinct subtype of PTSD. An early study found differences in plasma activity of the enzyme dopamine β-hydroxylase (DBH) in individuals with PTSD-SP compared with those with PTSD without SP and healthy control subjects (
15). DBH converts norepinephrine to dopamine. We found elevated DBH in PTSD-SP. This result may be counterintuitive because elevated DBH would be expected to result in lower dopamine (and therefore a reduced propensity for psychosis). However, given data implicating norepinephrine in PTSD, this elevated DBH may be consistent with a more severe variant of PTSD, also consistent with our earlier data (
16). Activity of DBH has been reported to be low or normal in schizophrenia and in major depression with psychotic features. However, DBH may be elevated in bipolar disorder with psychotic features.
Smooth pursuit eye movement (SPEM) abnormalities have been reported in schizophrenia (
17). Smooth pursuit allows the eyes to follow a moving stimulus. Cerebone et al. (
17) compared SPEM in subjects with PTSD-SP with schizophrenia with that in healthy control subjects. Altered SPEM was found in subjects with PTSD-SP compared with control subjects and subjects with schizophrenia. Subjects with PTSD-SP had impaired SPEM at higher velocities, whereas subjects with schizophrenia had deficiencies at lower velocities.
Functional alterations in the hypothalamic-pituitary-adrenal axis have long been described in PTSD (
18). Sautter et al. (
6) assessed cerebrospinal fluid concentrations of corticotrophin-releasing hormone in subjects with PTSD, subjects with PTSD-SP, and healthy subjects. Subjects with PTSD-SP had significantly elevated corticotrophin-releasing hormone levels compared with subjects with PTSD without psychotic features and healthy control subjects. Somatotropin release-inhibiting hormone was also measured in the cerebrospinal fluid in this study, but no differences in levels were found among comparison groups.
In another study of catecholamine metabolism in these patients (
19), platelet monoamine oxidase B (MAO-B) activity was found to be elevated in PTSD-SP. This study also investigated the genetics of platelet MAO-B in four groups: subjects with PTSD-SP, subjects with PTSD, combat-matched subjects without PTSD, and healthy control subjects. The MAO-B intron 13 polymorphism (G/A substitution) was assessed, and no significant effect of this genotype was found among groups (see also Genetic Considerations below). However, controlled for smoking status, the PTSD-SP group had significantly elevated MAO-B activity compared with that of the other three groups.
Altered platelet serotonin levels have been reported in a number of psychiatric disorders. Pivac et al. (
20) investigated platelet serotonin levels in veterans without PTSD, veterans with PTSD, and veterans with PTSD-SP. Platelet serotonin levels were elevated in subjects with PTSD-SP compared with those in the other two groups. The serotonin levels had a positive correlation with the PANSS positive syndrome subscale, in particular with delusional thinking. This study also provides evidence to support a biological differentiation of subjects with PTSD-SP from subjects with PTSD and healthy subjects.
Genetic considerations
There is little research investigating the genetics of psychotic symptoms in PTSD. However, approximately 30%–40% of the variance associated with anxiety disorders may be heritable as reviewed by Norholm et al. (
21). Special emphasis is given in their review to the importance of studying gene × environment interactions in anxiety disorders in general. Nugent et al. (
22) have reviewed the genetics of PTSD, noting that the field is still in its infancy. These authors cite studies supporting further investigation of the genetics of PTSD. They reviewed literature from family studies noting that the syndrome is heritable, in particular twin studies, e.g., that of True et al. (
23). They cite literature supporting the notion that genetic influences common to generalized anxiety disorder and panic disorder symptoms account for 60% of the genetic variance in PTSD. In their review of case control candidate gene associations in PTSD 10 studies were identified. These studies support gene associations with certain dopamine receptors (D2A1) and dopamine and serotonin transporter genes in particular.
Only one genetic study addressing psychotic symptoms in PTSD has been conducted. Pivac et al. (
19) measured platelet MAO-B activity and MAO-B intron 13 polymorphism (a G/A substitution) in male war veterans (N=106) with DSM-IV-TR-diagnosed current and chronic PTSD, divided into subgroups of patients with PTSD with (n=28) or without (N=78) psychotic features, combat exposed veterans (N=41) who did not develop PTSD, and healthy control men (N=242). Although genetic (MAO-B) polymorphisms did not differentiate the groups, the results suggested that platelet MAO-B activity, controlled for smoking status, might be used as a peripheral marker of psychotic symptoms in PTSD. To our knowledge, this is the only study that has investigated the genetics of PTSD without psychotic features versus PTSD-SP. In particular, there are no published studies investigating DBH genotypes and PTSD without psychotic features versus PTSD-SP. Because of the above hormonal and enzyme findings, it is reasonable to explore genetic contributions to psychosis in PTSD. This is especially relevant given the variation in DBH levels between patients with psychotic and nonpsychotic PTSD and because DBH is a genetic marker.
A brief review of general PTSD genetic studies follows. No significant association between Leu7Pro polymorphism (reflecting the neuropeptide Y gene) and PTSD was determined in an earlier report despite the potential role of neuropeptide Y in the stress-response (
24). Alterations in function of the hypothalamic-pituitary-adrenal axis have long been implicated in PTSD. However, in an initial report, glucocorticoid receptor genetic analyses showed no significant association between glucocorticoid receptor polymorphisms and PTSD (
25). Although brain-derived neurotropic factor is probably involved in stress and resilience, no association was determined between three genetic variants and PTSD (
26) in a preliminary study.
Serotonin function is altered in PTSD and, in fact, two selective serotonin reuptake inhibitor antidepressants are U.S. Food and Drug Administration-indicated for the treatment of PTSD (
27,
28). Altered serotonin function is relevant in PTSD-SP in light of the above noted findings by Pivac et al. (
19). Serotonin function is also relevant in psychoses, but studies have not addressed its relevance in PTSD with psychosis per se. In major depression, considerable interest had been focused on alterations in the serotonin transporter gene as a predictor of the development of depression, which may also be the case in PTSD. With this in mind, Lee et al. (
29) reported excess s allele in subjects with PTSD compared with healthy control subjects. More recently, a significant association was described between the s/s genotype of SLC6A4 and PTSD in adults with high exposure to hurricane trauma and low social support (
30). Therefore, genetic markers of serotonin function may serve as predictors of vulnerability to PTSD and should be studied for PTSD-SP.
Dopamine function has long been of interest in psychoses. Of particular significance, preliminary biological studies have been consistent with elevated urinary dopamine excretion (
31) and plasma dopamine (
16) in PTSD. These studies suggest alterations in DBH function as also noted above in our plasma DBH (pDBH) study. Although pDBH may not reflect acute changes in sympathetic nervous system function, activity of pDbH may reflect alterations in long-term dopaminergic as well as noradrenergic function (
32). This is especially relevant given the dopamine hypothesis of psychosis. It follows that subjects with PTSD-SP may have unique alterations in the dopamine system compared with subjects with PTSD without psychosis and with healthy control subjects.
Further elaboration of genetic dopamine function studies follows. Comings et al. (
33) screened Vietnam veterans who were hospitalized on an addiction treatment unit for PTSD. They found that 58.3% of those veterans with PTSD carried the dopamine receptor D2A1 allele. Of 8 subjects who did not meet criteria for PTSD, only 12.5% carried the D2A1 allele (p=0.04 versus subjects with PTSD). A replication study showed similar findings in 13 subjects with PTSD and 11 subjects without PTSD. For the combined groups 59.5% of subjects with PTSD carried the D2A1 allele versus 5.3% of those without PTSD. The authors concluded that a dopamine D2 receptor variant in linkage disequilibrium with the D2A1 allele gives increased risk for PTSD and that the absence of this variant may be protective against development of PTSD.
In contrast to these findings, Gelernter et al. (
34) found no association between the D2A1 allele and PTSD. Young et al. (
35) reported an association between the D2A1 allele and PTSD only in those patients with “harmful drinking.” One study (
36) has reported genetic alterations in the dopamine transporter gene with an excess 9-repeat allele noted only in subjects with PTSD. These investigators examined the association of the dopamine transporter SLC6A3 3′ variable number tandem repeat polymorphism with PTSD. They evaluated patients with chronic PTSD (N=102) and a comparison group of 104 trauma survivors who did not have PTSD. A significant increase in the 9-repeat allele was found in subjects with PTSD (43.0%) compared with the control subjects (30.5%, p=0.012). These authors also concluded that genetic alterations in dopamine function contribute to the risk for developing PTSD. Similar studies should be undertaken in PTSD with psychosis.
The only study to investigate pDBH activity and the −1021C/T polymorphism of the
DBH gene in PTSD found significantly lower pDBH activity (p<0.001) associated with the −1021C/T variant in combat veterans with PTSD (N=133) compared with combat veterans without PTSD (N=34) (
37). Patients with or without psychotic features were not specifically addressed in this report.
In summary, genetic studies in general support alterations in certain candidate genes associated with catecholamine or indolamine function in PTSD. These techniques should be extended to comparing PTSD-SP with PTSD without psychotic features. In particular, genetic correlates of dopamine function in PTSD-SP, including alterations in the DBH gene, should be determined.
Psychosocial considerations
There is little information addressing the issue of psychological and social correlates of psychotic symptoms in PTSD in the literature. It is possible that the interpretation of certain reexperiencing symptoms, e.g., hallucinations or intrusive memories, may lead to behaviors that further complicate the symptoms in addition to causing considerable psychological distress. Importantly, low social support in the aftermath of trauma has been shown to increase the risk for and severity of PTSD (
30). Most studies of PTSD-SP have consistently reported more severe symptom burden in these patients, so it would follow that viability of social supports played a role. Research investigating correlations between the original traumatic experience as well as new psychosocial stressors and the severity of psychotic symptoms should be undertaken. It is conceivable that the presence of these symptoms may lead to further social isolation and compound treatment and recovery.
Treatment considerations
The treatments for psychosis in the context of PTSD have also been minimally researched. We reported (
4) a global reduction in psychotic symptoms with the antipsychotic risperidone as measured by the PANSS (
38). Positive symptoms of psychosis showed a trend level of improvement as opposed to the overall PANSS improvement; however, this study was probably underpowered to detect change in the individual subscales of the PANSS. This study conducted by our group did suggest that PTSD-SP patients improved with adjunctive risperidone in terms of global reduction in PANSS scores and in CAPS cluster B (reexperiencing symptoms) scores. This is the only randomized, placebo-controlled trial of adjunctive therapy with risperidone for PTSD-SP reported to date. The study population had been relatively refractory to prior medication as well as to psychotherapeutic interventions and had a high PTSD symptom burden at study entry.
A number of studies have now investigated the use of atypical or new generation antipsychotics in the PTSD population (not necessarily with psychotic symptoms) as reviewed elsewhere (
2,
8,
38). The largest database is for risperidone. However, it should be emphasized that psychotic symptoms in the context of traumatic stress may not respond to antipsychotic medications, analogous to other psychoses, e.g., schizophrenia or bipolar disorder or major depression with psychotic features. The atypical antipsychotics should be reserved for patients with psychotic features or for patients with treatment-resistant conditions because of concerns about metabolic syndrome or other side effects such as extrapyramidal syndromes (
8).
Other agents that may have efficacy as monotherapy or adjunctive treatments could also be considered (
8,
39). One agent under consideration is prazosin, which has potential efficacy for nightmares and other sleep disturbances. As an α-1 receptor blocker, prazosin dampens noradrenergic function. The aforementioned elevated DBH levels in PTSD-SP would be consistent with high norepinephrine function. Therefore, clinical trials investigating the efficacy of prazosin for psychotic symptoms would be of interest for PTSD-SP. Further study should also be undertaken to confirm the clinical impression that an antidepressant plus an antipsychotic may be more efficacious for PTSD-SP, analogous to the treatment of major depression with psychotic features (
40).
To the author's knowledge, studies addressing specific psychotherapies for psychotic symptoms in this population have not been undertaken. The patient presented in the Introduction improved with a combination of medication and supportive therapy. Cognitive behavior therapies have been shown to be effective for PTSD in general. Components of cognitive behavior therapy specifically targeting psychotic symptoms should be developed for PTSD. In addition, group therapies to facilitate social integration may prove effective. Patients with more severe psychosis may benefit from partial hospitalization programs.
SUMMARY AND FUTURE DIRECTIONS
Clinicians should inquire about positive symptoms of psychosis not only during an initial diagnostic interview but also during follow-up sessions with a patient with PTSD because many patients are embarrassed about these symptoms, as well as about other facets and consequences of the traumatic experience, and may need some time in a trusting relationship to disclose these symptoms. This was the case with the patient in the Introduction. Biological and epidemiological studies suggest that these symptoms may be relatively prevalent in the PTSD population. Initial biological studies have indicated that patients with these symptoms may have a unique subtype of the disorder, but replication and extension of these studies is needed. More studies are also needed to investigate, in particular, the longitudinal course and treatment of psychotic features. The impact of these symptoms on social and global function should be studied. Genetic studies may shed light on differentiation of PTSD-SP as well as other PTSD comorbidities. The DBH candidate gene in may help shed light on this biological differentiation. Drug treatment most likely involves an antidepressant combined with an antipsychotic, analogous to the treatment of major depression with psychotic features. However, prospective controlled studies are needed to confirm this clinical impression. Supportive psychotherapy is probably beneficial, but studies investigating more specific CBT and other therapies are needed.