Case vignette
Robert is a 28-year-old male who was referred to you by his internist; he moved to town a month earlier and had asked his primary care physician for referral to help with the management of bipolar disorder.
When he scheduled his initial appointment, Robert had reported that “I've had bipolar disorder since college and need help with my meds.” The referral form indicated diagnoses of “bipolar disorder, hypothyroidism, mild chronic renal compromise.”
When the patient came in for his evaluation, he reported that he had been “frequently sad and moody” as a child but had first come to psychiatric attention while he was a college freshman. He related that “I had been stressed out with my first semester finals. I guess I was studying around the clock for a few days when I ‘lost it’… my mind went into overdrive, I didn't need to sleep or eat, and I thought that I didn't need to study any more because I would get the test answers telepathically from Zeus … which sounds crazy, I know, but at the time it felt so real.” He reported that he showed up for an exam dressed in a toga, with a wreath of ivy in his hair, “talking a blue streak,” and the campus security staff escorted him to the hospital; he was an inpatient for “about a week,” during which time he received lithium and olanzapine. After 2 months, his olanzapine dose was tapered and then discontinued, and he was managed on lithium alone for about 9 months before he persuaded the student health psychiatrist to discontinue it as well.
He did well for a year before he slumped into a depression in the context of “more than social” alcohol consumption at his fraternity and a full course load; poor academic performance happened at the same time, but he was unsure “which was the chicken and which was the egg” in terms of his depression and his academic failings. After about a month of “feeling like my world was falling apart,” he attempted suicide via lithium overdose; he was found by a roommate who called 911. He was hospitalized in the intensive care unit with acute renal failure, requiring hemodialysis temporarily for 2 weeks. Although medically stable, he was still endorsing active suicidal ideation at that point, and recalled “My life was going down the tubes and I really wanted to be dead. If I had been a little more brave, I would have done something lethal at dialysis.” Given the urgency of his situation, he received a course of electroconvulsive therapy (ECT), to which his mood and suicidal urges responded. After ECT, valproate (the divalproex formulation) was started and he did well; he took the semester off to “get my life back in balance” and to recover more fully from the cognitive side effects of his ECT treatment. After some initial protestations, he engaged in psychodynamic psychotherapy and learned more fully the importance of medications in staying well. He described that he began to be adherent to treatment, and his mood was generally stable. He denied any other periods of believing he had special powers such as his telepathic belief.
His academic performance improved considerably and he was able to graduate with honors in business administration. He entered a management training track at the regional office of a large company, which is headquartered in your area, and had done well over the past several years. He was promoted to a position in the main office and moved to town. He reported that it has been challenging to make new friends in this new locale but that his work was going well, although with a bit more stress and longer hours than he had imagined would be the case.
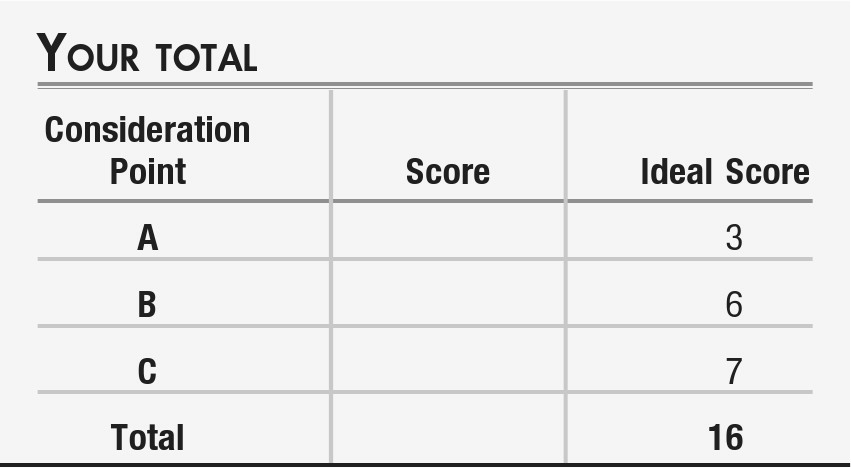
Consideration Point A:
At this point in your evaluation, the diagnosis that seems most appropriate for this patient would be
| A1._____ | Bipolar disorder type I |
| A2._____ | Bipolar disorder type II |
| A3._____ | Bipolar disorder not otherwise specified |
| A4._____ | Schizoaffective disorder, bipolar type |
Vignette continues
The patient decided to follow your recommendations for continued use of valproate and for seeing a therapist for social rhythm therapy. He did well for 6 more months, then started to note the return of some depressive symptoms—sleeping longer than expected, feeling lethargic during the day, and experiencing difficulties in making decisions about prioritizing tasks at work. He called to set up a visit sooner than his scheduled follow-up appointment, because “my mood is depressed more days than not, and I'm worried about another full-blown episode.” When he comes to the office, he described that he also had feelings of guilt with low self-esteem about “not deserving my job,” and feeling like he was “weighed down … my shoulders feel like they're covered in cement.” He told you he has been strictly adherent to daily valproate and has been trying to temper his social patterns as his therapist had taught him.
Consideration Point C:
What recommendation do you offer the patient at this point?
| C1._____ | Offer a trial of an adjunctive selective serotonin reuptake inhibitor (SSRI), starting at a low dose |
| C2._____ | Refer him for cognitive behavior psychotherapy |
| C3._____ | offer a trial of quetiapine monotherapy or of olanzapine-fluoxetine combination (OFC) treatment. |
Vignette concludes
With combined pharmacotherapy and psychotherapy, with valproate, an atypical antipsychotic agent, and cognitive behavior therapy, Robert's depressive symptoms came under control. He adjusted his schedule and used a second alarm clock to regularize his bedtime. He started volunteering at a nonprofit organization focused on “greening” the town (e.g., with tree planting events), and widened his circle of friends. He also built a program of exercise into his weekly schedule to avoid any weight gain associated with his medication. He continued to do well in follow-up.